Diabetes Mellitus, Hba1c and Risk of Hospitalization for Pneumonia
Senay Ozturk Durmaz1*, Ece Celik2 and Mehmet Celik3
1 Department of Infectious Diseases and Clinical Microbiology, Antalya Kepez State Hospital, Turkey
2 Division of Allergy and Clinical Immunology, Antalya University Medical Faculty, Turkey
3Department of Endocrinology and Metabolism, Antalya Kepez State Hospital, Turkey
Submission: March 18, 2019; Published: April 10, 2019
*Corresponding author:Senay Ozturk Durmaz, Department of Infectious Diseases and Clinical Microbiology, Antalya Kepez State Hospital, Antalya, Turkey
How to cite this article:Senay O D, Ece Celik, Mehmet C. Diabetes Mellitus, Hba1c and Risk of Hospitalization for Pneumonia. J Endocrinol Thyroid Res. 2019; 4(2): 555634. DOI: 10.19080/JETR.2019.04.555634
Abstract
Objective: To evaluate the hospitalization rates for pneumonia in patients with diabetes mellitus and to evaluate the effect of HbA1c on hospitalization for pneumonia.
Materials and Methods: We defined patients hospitalized with pneumonia between January 2018 and January 2019, and the health services databases were retrospectively reviewed. Relative risk and risk factors for pneumonia in diabetic and non-diabetic patients were evaluated.
Results: The files of 597 patients hospitalized for pneumonia were evaluated retrospectively. The mean age of the patients was 66.8±15 years. 353 (59.1%) of the patients were males and 244 (40.9%) were females. Diabetes mellitus (DM) was present in 80 (13.4%) patients and 517 (86.6%) patients did not have DM. Mortality was seen in 5 patients (6.3%) with DM and 27 patients (5.2%) without DM. There was no statistically significant difference between two groups in terms of mortality (p = 0.70). Six (7.5%) patients with DM and 66 (12.8%) non-diabetic patients were hospitalized in intensive care unit. There was no statistically significant difference between two groups in terms of admission to intensive care unit (p=0.17). Patients with COPD were excluded from the study after statistical analysis; intensive care unit stay was significantly lower in diabetic patients (p: 0.010). No statistically significant difference was found between two groups in terms of pneumonia-associated mortality (p: 0.478).
Conclusion: In diabetic patients, HbA1c values higher than target level and poor long-term glycemic control clearly increase the risk of hospitalization with pneumonia
Keywords: Pneumonia; Diabetes Mellitus; HbA1c
Introduction
Diabetes mellitus (DM) is one of the most common chronic diseases in the world. It constitutes a huge economic burden on countries’ health resources [1]. Studies have shown that community-acquired pneumonia is more common in diabetic patients and response to treatment is poor among these subjects. Although some studies suggest increased pneumonia related mortality for diabetics, others confirm no association [2-5]. The aim of this study was to evaluate the incidence of acquired pneumonia in diabetic population and to evaluate the effect of HbA1c on hospitalization due to pneumonia.
Materials and Methods
Between January 2018 and January 2019, we identified patients hospitalized with pneumonia, and health services databases were retrospectively reviewed. Relative risk and risk factors for pneumonia in diabetic and non-diabetic patients were evaluated. Data were analyzed using a commercially available software package (SPSS for Windows, version 22.0; SPSS Inc; NY,). In univariate analyses, differences in proportions were tested with the X2 test or Fisher exact test, and differences in the means of dimensional variables were tested with the Student t test. The level of significance was set at p <0.05.
Results
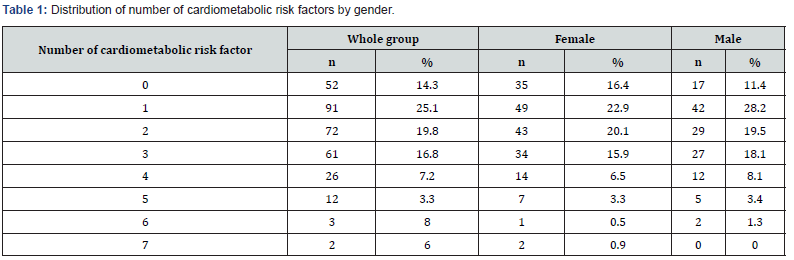
In this study, the files of 597 patients who were hospitalized in Antalya Kepez State Hospital between January 2018 and January 2019 were evaluated retrospectively. The mean age of the patients was 66.8 ± 15 years. While 353 (59.1%) of the patients were males, 244 (40.9%) were females. While chronic obstructive pulmonary disease (COPD) was present in 321 (53.8%) of the patients, 276 (46.2%) had no COPD. Diabetes mellitus was present in 80 (13.4%) patients and 517 (86.6%) patients did not have DM. The number of patients with HbA1c ≤ 7% was 17 (21.25%), HbA1c was > 7 - %10 in 50 subjects (62.5%) and HbA1c was> 10 in 13 patients (16.25%) (Table 1). While 72 (12.1%) of the patients were followed up in intensive care unit, 525 (87.9%) patients were hospitalized in the ward.
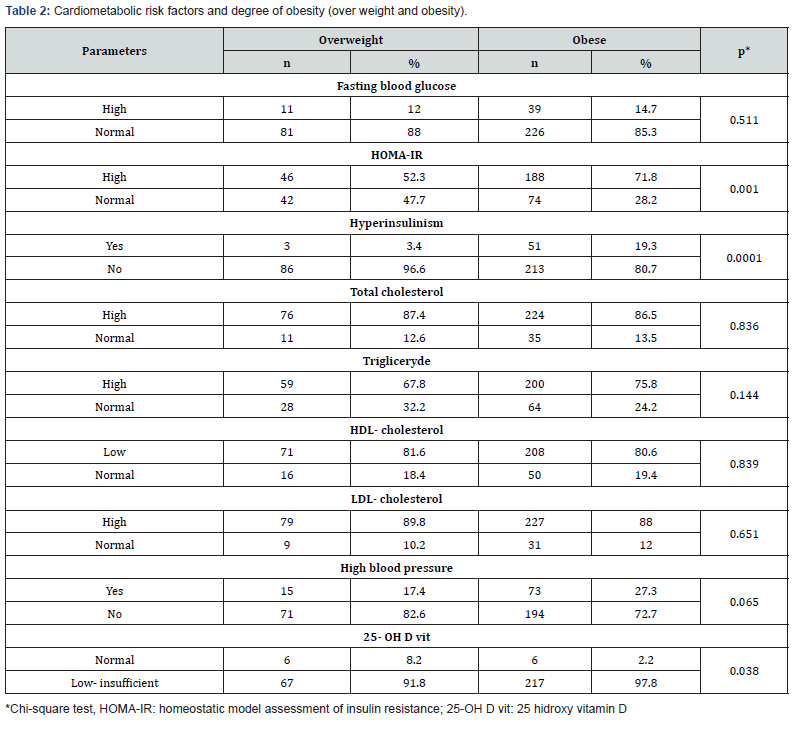
While 32 (5.4%) of the patients had mortality, 565 (94.6%) patients were discharged. Mortality was seen 5 patients (6.3%) with DM and 27 patients (5.2%) without DM, there was no statistically significant difference between two groups (p=0.70). Six (7.5%) patients with DM and 66 (12.8%) non-diabetic patients were hospitalized in intensive care unit. There was no statistically significant difference between two groups in terms of admission to intensive care unit (p=0.17). After excluding patients with COPD, patients with pneumonia were evaluated as two groups according to the presence of diabetes mellitus; intensive care unit hospitalization was significantly lower in diabetic patients (p: 0.010). There was no statistically significant difference between two groups in terms of pneumonia associated mortality (p: 0.478) (Table 2).
Discussion
In this observation, patient had symptoms of gestational transient thyrotoxicosis. A similar picture of gestational transient thyrotoxicosis and thyrotoxicosis often leads to several diagnostic errors and leads to incorrect treatment tactics and to prescribing unreasonable appointment of antithyroid drug. Thus, when observing symptoms of thyrotoxicosis at the beginning of pregnancy, more attention to complaints, history of thyrotoxicosis, the severity of clinical signs of thyrotoxicosis, thyroid ultrasound, low levels of TSH receptors antibodies and slightly elevated levels of free T4 and TSH. During the diagnosis of gestational transient thyrotoxicosis, antithyroid drug not recommended, more preferred symptomatic treatment. By the middle of the second trimester, patient’s clinical condition is improving, and indicators of the hormonal status are normalized due to the physiological decrease of hCG.
References
- Shaw JE, Sicree RA, Zimmet PZ (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 87(1): 4-14.
- Shah BR, Hux JE (2003) Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care 26(2): 510-513.
- Falguera M, Pifarre R, Martin A, Sheikh A, Moreno A (2005) Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest 128(5): 3233-3239.
- Kornum JB, Thomsen RW, Riis A, Lervang HH, Schønheyder HC, et al. (2008) Diabetes, glycemic control, and risk of hospitalization with pneumonia: a population-based case-control study. Diabetes Care 31(8): 1541-1545.
- Eurich DT, Gamble JM, Marrie TJ, Majumdar SR (2010) Dysglycaemia and 90 day and 1 year risks of death or readmission in patients hospitalised for community-acquired pneumonia. Diabetologia 53(3): 497-503.
- Debczyński W, Pietruska Z (1994) Chemotaxis and spontaneous migration of neutrophil leukocytes from patients with diabetes. Pol Tyg Lek 49(1-3): 11-13.
- Marhoffer W, Stain M, Maeser E, Federlin K (1992) Impairment of polymorphonuclear leukocyte function and metabolic control of diabetes. Diabetes Care 15: 256-260.
- Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, et al. (1997) Impaired leucocyte functions in diabetic patients. Diabet Med 14(1): 29-34.
- Marfoffer W Stein M, Schleinkofer L, Federlin K (1994) Monitoring of polymorphonuclear leukocyte functions in diabetes mellitus..A comparative study of conventional radiometric function tests and low-light imaging systems. J Biolumin Chemilumin 9(3): 165-170.
- McManus LM, Bloodworth RC, Prihoda TJ, Blodgett JL, Pinckard RN (2001) Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol 70: 395-404.
- Senior PA, Marshall SM, Thomas TH (1999) Dysregulation of PMN antigen expression in Type 2 diabetes may reflect a generalized defect of exocytosis: influence of hypertension and microalbuminuria. J Leukoc Biol 65(6): 800-807.
- Alfonso C, Han JO, Williams GS, Karlsson L (2001) The impact of H2-DM on humoral immune responses. J Immunol 167(11): 6348-6355.
- Aberegg SK (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354(19): 2069-2071.






























