Could Hormone Remission be Achieved in Prolactinomas with Surgery?
Palamar O*, Huk A, Aksyonov R, Okonskyi D andTeslenko D
Department of endoscopic and craniofacial neurosurgery, Romodanov Neurosurgery Institute, Ukraine
Submission: May 24, 2018;Published: July 18, 2018
*Corresponding author: Palamar O, Department of endoscopic and craniofacial neurosurgery, Romodanov Neurosurgery Institute, Kiev, Ukraine
How to cite this article: Palamar O, Huk A, Aksyonov R, Okonskyi D, Teslenko D. Could Hormone Remission be Achieved in Prolactinomas with Surgery?. J Endocrinol Thyroid Res . 2018; 3(5): 555622. DOI:10.19080/JETR.2018.03.555622
Abstract
We retrospectively analyzed 33 prolactinomacases. Endoscopic endonasal transsphenoidal (EET) surgery can be used as an effective method for microprolactinomastreatment to achieve rapid biochemical and clinical remission. In some macroprolactinomas (<24mm) EET surgery is effective (90% cases)
Keywords: Pituitary adenoma;Prolactinoma;Endoscopic endonasal transsphenoidal surgery;Biochemical remission
Introduction
Dopamine agonists (DA) are recognized as an effective medical treatmentsince the beginning 1970s[1,2]Normoprolactinemia was achievedin 59%when using bromocriptine[3].Normal PRL level can be achieved in 80-90%when using DA. Relevant systemic side effects, including vomiting, nausea, dizziness, headache have been reported in about one third of patients treated with DAs[ 4, 5]. DAs have a significant effect on other dopamine, serotonin androgenic receptors, which leads to severe neurological disorders such as postural hypotension or dyskinesia, psychosis, or mania, which provoke compulsive states[ 6,7]. In some cases these possible complications assume surgery over prolactinomas.
Materials and Methods
This study included 33 patients who underwent primary pituitary surgery over prolactinomas with no prior DA treatment (19 female, 14 male; age ranged, 20–67 years). Microprolactinomas10 cases, macroprolactinomas19 cases, giant prolactinoma 4 cases.endoscopic endonasal transsphenoidal (EET) surgery was performed by single neurosurgeon. Plasma PRL levels were obtained before surgery, and then on the 1st day, 1st week, 1st month, 3rd month and then every 6th months after surgery. Catamnesis1-5 yearsMRI check-up was performed before surgery and then on 3, 6 and 12month, then on yearly basis.
Results and Discussion
Median preop PRL serum level for all patients was530ng/mL (ranging, 65–1440ng/mL)Cavernous sinus invasion was ob served in 16 (48,5%) cases after surgery. Biochemical remission of PRL level back to normal wasin 10 cases withmicroprolactinomas (100%), in 10 (53%) cases of macroprolactinomas after surgery.No DA therapy after surgery in those with normal PRL serum level. Follow up lasted1-5 years. Postoperative complications such as CSF leak, meningitis, additional oculomotor disorder or visual impairment have not been established. No mortality. Biochemical and clinical remission was achieved after EET surgery with no DA therapy: microadenomas - 100% cases, macroprolactinomas– 53% (macroprolactinomas with size less then 24mm – 90% cases). Visual disturbances and visual field defects improved in all cases over macro and giant prolactinomas.
EET surgery overmicro and macroprolactinomas (tumor should be removed in capsule) achievesbiochemical and clinical remission within a short period of time. Though EET surgery over microprolactinomas gives 100% remission rate, in cases of macroprolactinomas EET surgery gives 53% remission rate. Macroadenomas give recurrence after surgery in6 months period. We noticed that the size starting from 24mm and more would likely to lead to recurrence. Meanwhile macroprolactinomas less then 24mmgive 90% remission. Cavernous sinus invasion is predicting factor over recurrence.
Foote Note
1Thorner MO, McNeilly AS, Hagan C & Besser GM. Long-term treatment of galactorrhoea and hypogonadism with bromocrip- tine. BMJ 1974 2 419–422.
2Werder K, Fahlbusch R, Landgraf R, Pickardt CR, Rjosk HK & Scriba PC. Treatment of patients with prolactinomas. Journal of Endocrinological Investigation 1978 1 47–58
3WebsterJ,PiscitelliG,PolliA,FerrariCl,IsmailI&ScanlonMF.For the Cabergoline Comparative Study Group. New England Journal of Medicine, 1994 904–909
4Molitch ME (1999) Medical treatment of prolactinomas. Endo- crinolMetab Clin North Am 28(1):143–169
5Diagnosis and treatment of hyperprolactinemia: An endocrine society clinical practice guideline, 2011
614.Noronha S, Stokes V, Karavitaki N & Grossman A. 2010. Treating prolactinomas with dopamine agonists: always worth the gamble?.Endocrine In press 10.1007/s12020-015-0727-2
716.Ali S, Klahr K &Freudenreich O. 2015. Management of psychosis associated with a prolactinoma: case and review of the literature. Psychosomatics 51 2010. 370–376. 10.1016/S0033-3182(10)70718-0.
Conclusion
Biochemical remission could be achieved surgically especially in microprolactinomas in 100% cases.
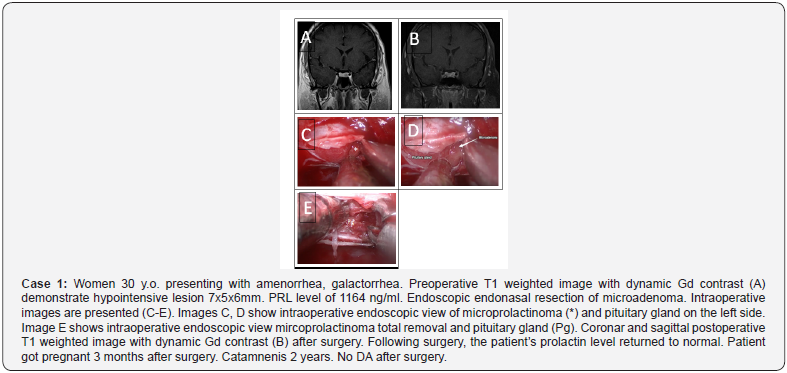
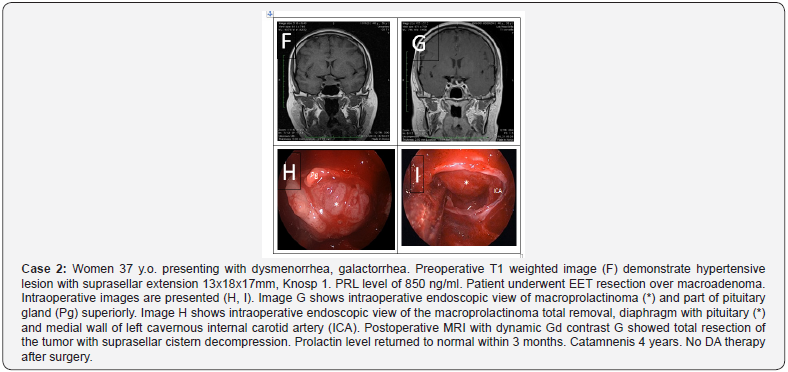
Biochemical remission might be achieved surgically in macroprolactinomas with size less then 24 mm (90% cases), cavernous sinus invasion (Knosp 0-2) is the prognostic factor.Ophthalmic symptoms regression is achieved in 100% patients and faster in cases macro and giant adenoma in comparison to DA therapy. Menses normalized in 100% cases of microprolactinomas and in 86% cases in macroadenomas with size less then 24mm.