Role of VATS in Ectopic Mediastinal Parathyroid Tumor
Manish Sahni1*, Vivek Agarwal1, Aarti Sahni2 and Deepak Khandelwal3
1Department of Endocrine Surgery, BLK Hospital, India 2Department of Endocrinology, Sir Ganga Ram Hospital, India 3Department of Endocrinology, Maharaja Agarsen Hospital, India
Submission: August 08, 2017;Published:September 18, 2017
*Corresponding author: Manish Sahni, Sir Ganga Ram Hospital, Old Rajinder Nagar, New Delhi-110060, India, Tel:+918130380962; Email: drmanish_sahni@yahoo.com
How to cite this article: Manish S, Vivek A, Aarti S, Deepak K. Role of VATS in Ectopic Mediastinal Parathyroid Tumor.J Endocrinol Thyroid Res. 2017; 2(5):555596. DOI: 10.19680/JETR.2017.02.555596.
Introduction
In 1849, Sir Richard Owen, provided the first accurate description of the normal parathyroid gland after autopsy examination of an Indian rhinoceros. However, Ivar Sandstrom suggested these glands being named Glandulae parathyroideae. The first successful parathyroidectomy was performed in 1925 by Felix Mandl. It was Edward Churchill who identified first time the ectopic parathyroid adenoma substernally on his one of the patients in 1926. Embryologically, the superior parathyroid glands are derived from the 4th branchial pouch while the inferior parathyroids are derived from 3rd branchial pouch [1]. However, true ectopic superior parathyroid glands are rare, but may be found in the middle or posterior mediastinum or in the aorto-pulmonary window [2].
Primary hyperparathyroidism is a common disorder affecting 100,000 individuals annually in US. It occurs in 0.1% to 0.3% of the general population and is more common in women (1:500) than in men (1:2000). It is characterized by increased parathyroid cell proliferation and PTH secretion that is independent of serum calcium levels. Though the exact etiology of PHPT is unknown, although exposure to low-dose therapeutic ionizing radiations, familial predisposition and genetic factors account for some cases.
We have done over 400 cases of parathyroid surgeries in last 10 years in our department but only 4 patients presented with ectopic parathyroid disease [3] cases were in anterior mediastinum and only 1 case in posterior mediastinum). We are showing the management of ectopic parathyroid tumor in posterior mediastinum and role of VATS, its benefits over standard open thoracotomy in managing ectopic parathyroid tumor.
Subjects and Methods
63 year old lady presented with generalized bony pains, history of recurrent renal stones. She got operated twice, one for right renal stones with PCNL in 2011 (outside) and another dynamic hip screw for neck of femur fracture in 2014. During evaluation, her vitas were stable with essentially normal systemic examination. On local examination of neck, no palpable neck swelling was evident. On further evaluation by biochemical studies, she was found to be hypercalcemic with serum calcium levels of 13mg/dl with decreased serum phosphate and elevated 24 hour urinary calcium concentrations her serum PTH levels were 320ng/ml (high).
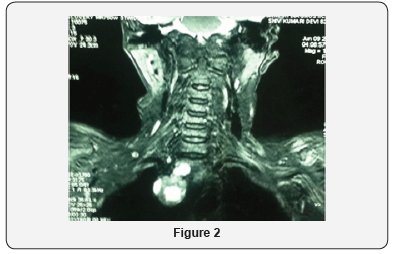
On radiological evaluation, her DEXA scan showed T score of -3.0 at the region of distal radius bone. Her ultrasound whole abdomen revealed non-obstructing 2mm stone right renal upper calyx. Ultrasound neck showed no abnormality. Sestimibitechnetium 99m scan revealed uptake over right mediastinal region (Figure 1). MRI neck and chest revealed 2.5cmx2.0cm oval shaped hyperintense lesion in the right paratracheal region in postero superior mediastinum (Figure 2). With the diagnosis of primary hyperparathyroidism with ectopic mediastinal parathyroid adenoma, she was optimized for surgery. She underwent Video- assisted thoracoscopic surgical approach.3 ports were made. 2 working ports of 5mm size were made on right anterior axillary and midclavicular line and one 10mm camera port was made midway between two 5mm ports. Her operative findings revealed an oval shaped 2.5cmx2cm hyper vascular lesion abutting right posterlateral wall of SVC. The tumor was excised using Harmonic scalpel energy device. Intraoperative IOPTH levels were sent during surgery and at 10 minutes after the excision of tumor with significant drop (>50%) in serum PTH post excision values. Hemostasis was achieved. Ports were closed with skin stapler after placing a intercostal drain from 10mm port site (Figure 3 & 4).
She developed hypocalcemia on post operative day 1 and was managed with i/v calcium for 2 days and stabilized later with oral calcium and vitamin D supplements in the follow up period. She was discharged on postoperative day 4.
Results
Histopathology report revealed parathyroid adenoma. During her first postoperative follow up after 2 weeks of surgery, her serum calcium levels were 8mg/dl and returned to normal activities within a week without pulmonary complications. At present she is on regular follow up and is doing fine.
Discussion
Primary hyperparathyroidism with ectopic parathyroid tumor being a rare entity. In the background of clinical symptoms and biochemical studies suggestive of hyperparathyroidism with no clinically palpable neck mass, high suspicion of ectopic parathyroid tumor should be kept in mind. Sestimibi-technetium 99m scan allows planar and SPECT imaging to identify ectopic parathyroid tumor. Also SPECT scan can indicate whether an adenoma is located in anterior or posterior mediastinum, thus enabling the surgeon to modify the operative approach accordingly. Though CT and MRI scans are less sensitive than sestimibi scans but are helpful in localizing large paraesophageal and mediastinal glands. The intraoperative PTH levels fall of >50% after 10mins. of gland excision is considered reliable test [3]. Thoracic surgical approaches have changed over recent years with advancements in minimally invasive surgery. As surgeon trained in advanced minimally invasive techniques can now perform pleural based, pulmonary and mediastinal procedures through multiple thoracoscopic ports without the need for a substantial, rib spreading incision. For ectopic mediastinal parathyroid tumor excision, either open sternotomy or VATS approach can be undertaken. Subjective measures of quality of life after VATS such as pain and perceived functional recovery, consistently and reproducibly favor VATS over thoracotomy [4]. Objective measures such as functional status as measured by 6min walk, return to work and daily activities also favor VATS over thoracotomy.
Finally recovery of respiratory function occur earlier in VATS patients [4]. When VATS is not possible, an open approach mostly posterlateral thoracotomy is used to gain access to the in trathoracic space for operations in the posterior mediastinum, pulmonary and oesophageal resections [5].
Conflict of interest
There is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
References
- Henry J (2003) Applied embryology of the thyroid and parathyroid gland. In Randolph G (Ed.), Surgery of the thyroid and parathyroid glands.
- Akerström G, Malmaeus J, Bergström R (1984) Surgical anatomy of human parathyroid glands. Surgery 95(1): 14-21.
- Sharma J, Milas M, Berber E, Mazzaglia P, Siperstein A, et al. (2008) Values of intraoperative parathyroid hormone monitoring. Ann surg Oncol 15(2): 493-498.
- Demmy TL, Nwogu C (2008) Is Video-assisted thoracic surgery better? Quality of life considerations. Ann Thorac Surg 85(22): S719-728.
- Swanson SJ, Herndon JE, Amico DTA, Demmy TL, McKenna RJ, et al. (2007) Video-assisted thoracic surgery lobectomy: report of CALGB 39802-aprospective, multi-institution feasibility study. J Clin Oncol 25(31): 4993-4997.






























