Thermal Ablation for Benign Thyroid Nodules: Radiofrequency
Cesareo R1, Gaspa G 2*, Di Mauro A3, Casini A1, Pasqualini V4 and Cianni R4
1Thyroid Diseases Center, SM Goretti Hospital, Italy
2Department of Medicine, Campus Bio-Medico University of Rome, Italy
3Department of Medicine, Campus Bio-Medico University of Rome, Italy
4Department of Radiology, SM Goretti Hospital, Italy
Submission: March 08, 2017; Published: April 06, 2017
*Corresponding author: Gaspa G, Department of Medicine, Food Science and Nutrition Unit, Campus Bio-Medico University of Rome, Italy, Email: gainluigi.gaspa@virgilio.it
How to cite this article: Cesareo R, Gaspa G , Di M A, Casini A, Pasqualini V , Cianni R. Thermal Ablation for Benign Thyroid Nodules: Radiofrequency. J Endocrinol Thyroid Res. 2017; 1(4): 555566. DOI:10.19080/JETR.2017.01.555566
Introduction
Nodular thyroid disease is common in adult population. Although most thyroid nodules are benign and treatment is often not necessary, some patients require treatment due to pressure symptoms or cosmetic complaints [1]. Unfortunately, levothyroxine therapy presents a significant reduction of the initial size only in a limited group, while a number of nodules continue to grow progressively. Whilst these studies refer to the treatment of uninodular goiter, clinical data regarding the efficacy of levothyroxine therapy on multi-nodular goiter are less specific. Moreover, only one randomized study seems to confirm a certain efficacy, although without no long-term data. Further long-term levothyroxine suppression treatment in elderly patients is associated with adverse effects on bones and on the cardiovascular system. In addition, radioiodine therapy may be ineffective in large non-hyperfunctioning nodules [2,3].
Numerous case report and prospective randomized controlled trials with different treatment algorithms have confirmed the clinical effectiveness and safety of thermal ablation therapies, in particular laser therapy (LT) and radio frequency thyroid ablation (RTA) for the management of benign thyroid lesions.In particular, LA investigated primarily that the treatment of solid nodules is successful in reducing the volume of treated thyroid nodules by 40% to 80%. In patients followed for more than 5 years, LA results in a satisfactorily mid to long-term clinical response in the majority of cases [4-6]. RTA, introduced in 2006, has been reported to be a safe, effective treatment for benign thyroid nodules [7]. In this short review, we aim to describe the advantage of using RTA for the treatment of thyroid nodules.
Technique
At the beginning, thyroid nodules should be confirmed as benign on at least two separate ultrasound (US)-guided fine needle aspirations and/or core needle biopsies. We do not advise the treatment of follicular neoplasm (classified as Ty3 according to the British and Italian reporting system for thyroid cytopathology that corresponds to Bethesda Categories III and IV nodules) since there is a high risk of malignancy. Caution should be taken in performing RTA on benign nodules with ultrasound characteristics of malignancy. RTA offers the opportunity of using cooled needles of different thicknesses and lengths. In particular, the most common electrodes used in Italy are 14 gauge, 10cm long, with 4 to 9 hooks, expandable to 3.5-4.0cm, and a 17 gauge electrode, 15cm long, with a 1cm active point. The latest version is a thinner 18 gauge electrode with various sized active points, ranging from 0.5 to 1.5cm. Regarding the hook-umbrella technique where hooked needles are fixed inside the thyroid nodule, both the 17 and 18 gauge needles are used with the “moving shot” technique,described by Beak [8]. The thyroid nodule is generally subdivided in many small units and the therapist performs thermal ablation of each unit by moving the radiofrequency electrode. It is initially positioned in the deepest part of the nodule and issubsequentially shifted laterally and across the isthmus. The treatment usually starts with 30W and, as soon as a hyperechogenic area appears (i.e., proving necrosis), the needle is removed to ablate the next area. If the hyperechogenic area does not appear after 5 to 10 seconds of treatment, the power is increased by 10W until a maximum of 100-110W is reached. The treatment is considered completed when all the subunits of the nodule have been treated and show the classic post-ablation hyperechogenic tissue.
Discussion
US-guided minimally invasive procedures represent an alternative to surgery for the treatment of thyroid nodules, which grow and become symptomatic due to compressive symptoms.RTA has been used since 2006 to treat compressive thyroid nodules, mostly in Korea and in Italy [7,9-11]. We are currently leading multiple studies aiming to demonstrate clear efficacy of RTA on volume reduction of thyroid nodules. A significant reduction of thyroid nodule volume has been described by several studies-from 50 to 80% from baseline volume, depending on the study [11-13].
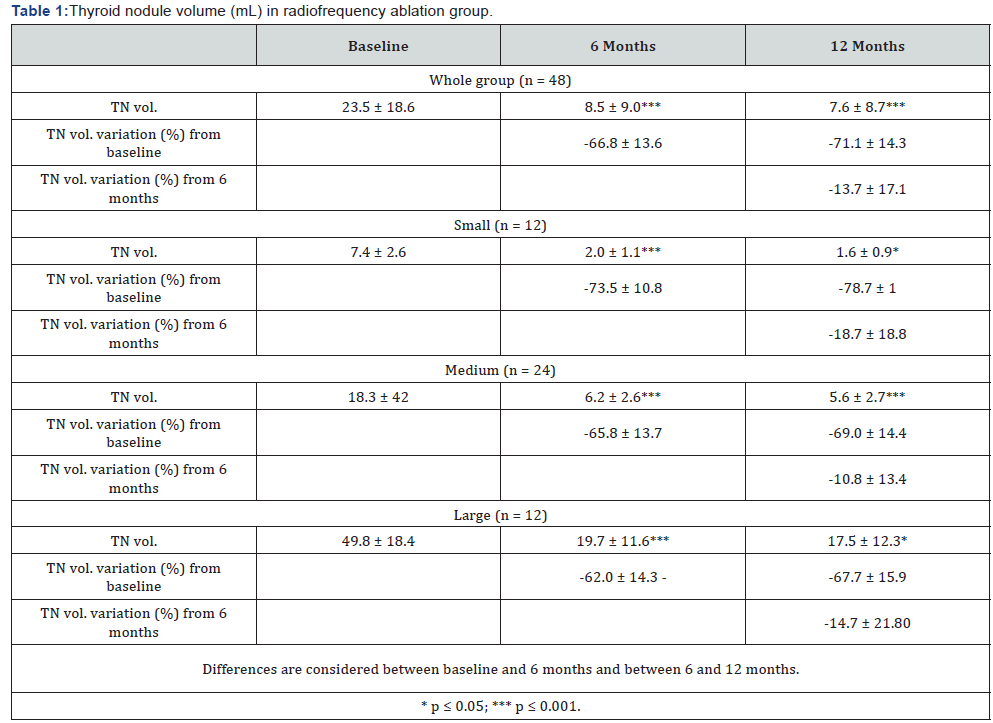
Our recent data regarding the efficacy of RTA at six months and at one year on thyroid nodules demonstrated that a single RTA treatment is effective in reducing benign, non-functional thyroid nodule volume, especially those small and medium sized [14,15] (Table 1). According to our research, RTA is effective in reducing the thyroid nodule volume, but, as the best reduction rate was seen in small thyroid nodules, such efficacy may be size-dependent. Therefore, more treatment is expected to treat larger nodules. Furthermore, several studies showed that larger nodules are often subjected to more treatments [10,16]. This may occur because a part of them showed a trend of recurrence. In very large thyroid nodules, RTA efficacy could be even less as the treatment is not uniformly distributed to the entire lesion [9,17]. At the moment, we do not have a common consensus on the definition of a small, medium or large nodule. Yet, we believe nodules with volume≤10ml should be considered small, whilst those bigger than 30ml should be considered large. Most clinical studies on RTA have been performed on benign thyroid cold nodules. We have less data about RTA efficacy on hot thyroid nodules. Recently, a multicentre study validated the efficacy of RTA in the latter, but it was necessary more than one single treatment in every nodule treated [17]. We believe radioiodine therapy remains the gold standard for the treatment of these nodules, RTA is effective only in the treatment of small-medium hot nodules. Moreover, when performed in experienced centres, RTA is a rapid, inexpensive, and safe method for inducing a clinically significant nodule volume reduction.
Conclusion
RTA represents a valid approach in patients with nodular goiter who are not eligible or failed conventional treatments, or have refused to be cure.RTAcan be considered a safe and effective therapeutic option in combination with laser ablation. In our opinion, RTA is most suitable for small and medium thyroid nodules; we need more data (particularly large and prospective studies) to evaluate the effectiveness of this procedure for the treatment of larger thyroid nodules.
References
- Papini E, Rago T, Gambelunghe G, Valcavi R, Bizzarri G, et al. (2014) Long-term efficacy of ultrasound-guided laser ablation for benign solid thyroid nodules. Results of a three-year multicenter prospective randomized trial. J Clin Endocrinol Metab 99(10): 3653-3659.
- Cesareo R, Iozzino M, Isgrò MA, Annunziata F, Di Stasio E (2010) Short term effects of levothyroxine treatment in thyroid multinodular disease. J Endocr 57(9): 803-809
- Valcavi R, Riganti F, Bertani A, Formisano D, Pacella CM (2010) Percutaneous laser ablation of cold benign thyroid nodules: a 3-year follow-up study in 122 patients. Thyroid 20(11): 1253-1261.
- Dossing H, Bennedbaek FN, Hegedus L (2011) Long-term outcome following interstitial laser photocoagulation of benign cold thyroid nodules. Eur J Endocrinol 65(1): 123-128.
- Pacella CM, Mauri G, Achille G, Barbaro D, Bizzarri G, et al. (2015) Outcomes and Risk Factors for Complications of Laser Ablation for Thyroid Nodules: A Multicenter Study on 1531 Patients. J Clin Endocrinol Metab 100(10): 3903-3910.
- Kim YS, Rhim H, Tae K, Park DW, Kim ST (2006) Radiofrequency ablation of benign cold thyroid nodules: initial clinical experience. Thyroid 16(4): 361-367.
- Na DG1, Lee JH, Jung SL, Kim JH, Sung JY (2012) Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol 13(2): 117-125.
- Baek JH, Kim YS, Lee D, Huh JY, Lee JH (2010) Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol 194(4): 1137-1142.
- Spiezia S, Garberoglio R, Di Somma C, Deandrea M, Basso E, et al. (2007)Efficacy and safety of radiofrequency thermal ablation in the treatment of thyroid nodules with pressure symptoms in elderly patients. J Am Geriatr Soc 55(9): 1478–1489.
- Deandrea M, Limone P, Basso E, Mormile A, Ragazzoni F, et al. (2008) US-guided percutaneous radiofrequency thermal ablation for the treatment of solid benign hyperfunctioning or compressive thyroid nodules. Ultrasound Med Biol 34(5): 784-791.
- Spiezia S, Garberoglio R, Milone F, Ramundo V, Caiazzo C, et al. (2009) Thyroid nodules and related symptoms are stably controlled two years after radiofrequency thermal ablation. Thyroid 19: 219-225.
- Faggiano A, Ramundo V, Assanti AP, Fonderico F, Macchia PE, et al. (2012) Thyroid nodules treated with percutaneous radiofrequency thermal ablation: a comparative study. J Clin Endocrinol Metab 97: 4439-4445.
- Deandrea M, J Yong Sung J, Limone P, Mormile A, Garino F, et al. (2015) Efficacy and Safety of Radiofrequency Ablation versus Observation for Non functioning Benign Thyroid Nodules: A Randomized Controlled International Collaborative Trial. Thyroid 25: 890-896.
- Cesareo R, Pasqualini V, Simeoni C, Sacchi M, Saralli E, et al. (2015) Prospective study of effectiveness of ultrasound-guided radiofrequency ablation versus control group in patients affected by benign thyroid nodules. J Clin Endocrinol Metab 100(2): 460-466.
- Cesareo R, Palermo A, Pasqualini V, Simeoni C, Casini A, et al. (2017) Efficacy and safety of a single radiofrequency ablation of solid benign non-functioning thyroid nodules. Arch Endocrinol Metab doi: 10.1590/2359-3997000000246.
- Sung JY, Baek JH, Jung SL, Kim JH, Kim KS, et al. (2015) Radiofrequency Ablation for Autonomously Functioning Thyroid Nodules: a multicenter study. A Multicenter Study. Thyroid 25: 112-117.
- Lim HK, Lee JH, HA EJ, Sung JY, Kim JK, et al. (2013) Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol 23(4): 1044-1049.






























