Impulse Oscillometry in The Monitoring of Pediatric Asthma
Alberto Vidal Grell*
Departament of Pediatric Pulmonology, Clínica MEDS, Chile
Submission: May 10, 2024; Published: May 22, 2024
*Corresponding author: Alberto Vidal Grell, MD, Avenida José Alcalde Délano 10581, Lo Barnechea, Santiago Chile
How to cite this article: Alberto Vidal Grell*. Impulse Oscillometry in The Monitoring of Pediatric Asthma. Int J Pul & Res Sci. 2024; 7(3): 555711. DOI: 10.19080/IJOPRS.2024.07.555711
Abstract
Impulse oscillometry (IOS) is a lung function study that uses pulse waves to measure respiratory impedance. It requires little effort, which makes it easily reproducible and useful when monitoring children with asthma. The accuracy of its interpretation depends on the reference predictive values. The most recent evidence positions it as a good method to predict loss of control, future risk of exacerbations, and persistent alterations of lung function in pediatric asthma.
Keywords: Asthma; Children; Lung function; Impulse oscillometry; Monitoring
Mini Review
IOS uses square-type sound waves at least 5 times per second in constant pulses to transmit airway pressure. Through these pressure pulses delivered to the respiratory system, a flow reaction is generated with its oscillations at certain frequencies. Higher frequency sound waves (>20 Hertz) move a shorter distance, so they will reflect the characteristics of larger airways. Lower frequency sound waves (<15 Hertz) travel deeper into the airways, allowing small airway parameters to be measured. By obtaining measurements at high and low frequencies, IOS can reflect proximal and distal airway function simultaneously, which is extremely useful in bronchial asthma [1]. Furthermore, the IOS is a test that requires minimal effort on the part of the patient, who only must breathe at tidal volume, which allows for measuring the lung function of many asthmatic children who are not able to perform spirometry.
Impulse oscillometry measures lung impedance (Zrs) which is composed of lung resistance (Rrs) and lung reactance (Xrs). The Rrs is the energy required to propagate the pressure wave through the airways and inflate the lung, reflecting the caliber of the airway. Narrower airways will have greater resistance due to greater frictional pressure loss as air flows through them. The Rrs at low frequencies such as 5 Hertz (R5) represents the resistance of the total airway (proximal and distal), while the resistance at higher frequencies, such as 20 Hertz (R20), represents only the resistance of the proximal airways. The Rrs of the peripheral airways can be determined by subtracting the resistance of the proximal airways (R20) from the total Rrs of the respiratory system (R5), and this value is commonly known as the R5-R20. Xrs is another IOS parameter used in asthma, which is frequency-dependent and measures the elastic retraction of lung tissue.
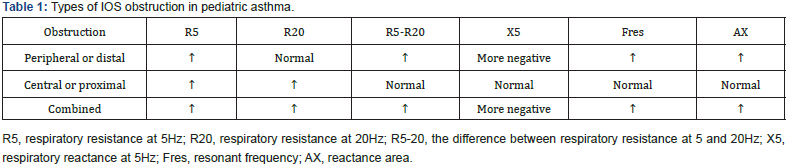
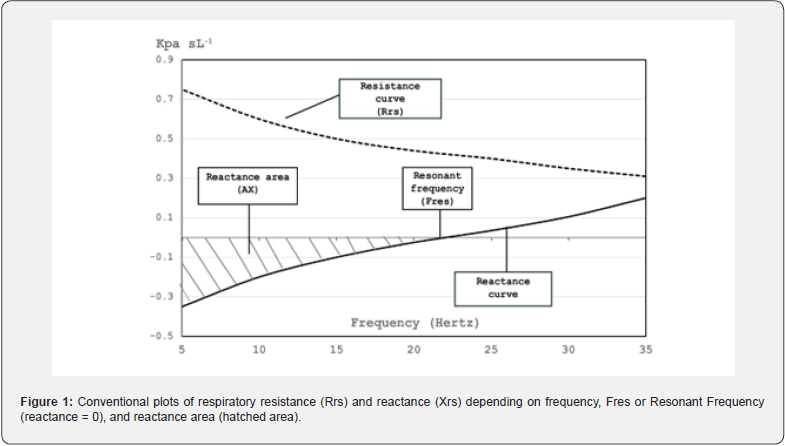
At low frequencies, the most negative values will predominate, while at higher frequencies the most positive values will predominate. In asthma, the most used parameter is the reactance at 5 Hertz (X5), which will be more negative as there is greater obstruction of the small airway. There is a point at which the reactance is equal to zero, it is known as the Resonant Frequency (Fres), and the area delimited by the horizontal axis, the Xrs curve below zero and vertex is in Fres, is called the reactance area (AX) or Goldman triangle [2,3]. (Figure 1) plots the curves of Rrs, Xrs, the reactance area, and Fres. In pediatric asthma, all or some of the IOS parameters can be altered and determine types of obstructive alterations. The most common is peripheral or distal airway obstruction followed by combined airway obstruction (distal and proximal) and very less frequent central or proximal airway obstruction [4]. (Table 1) shows the different parameters altered in each type of obstruction.
For the interpretation of IOS in asthma, it is important to have reference predictive values in healthy children. These predictive values vary with patient size, but also by age, gender, weight, and ethnicity. Currently, there are at least 15 countries on different continents that have reported predictive values for IOS in healthy children. When the predictive values between Hispanics and Caucasians have been compared, a good degree of agreement has been demonstrated for most of the IOS parameters, indicating that there would not be many geographic or ethnic differences [5]. Recently, Gochicoa, et al. [6] published continuous predictive values for life, which allows monitoring the patient with asthma from the preschool stage to adolescence without having to change the predictive values as the child grows, thereby eliminating the discordance that can be produced by mixing the different equations [6].
In recent years, evidence has increased regarding the role of IOS in the monitoring of pediatric asthma. Ling et al. [7] published a meta-analysis of 6 studies with 615 children and adolescents with asthma and showed that R5, X5, AX, and Fres are good IOS parameters to predict asthma exacerbations or loss of control [7]. In a prospective observational cohort of 560 asthmatic children between 6 and 12 years (average 9 years) it was shown that the parameters R5, R5-R20, X5, and AX can predict lower scores in asthma control measured by the childhood asthma control test (C-ACT). Furthermore, in this study, the parameter R5-R20, which reflects the alteration of the small airway, is the strongest risk factor for uncontrolled asthmatic children in multiple regression analysis [8]. A 3-year follow-up study with 66 asthmatic preschoolers showed that AX, R5-R20, and R5 had the best LR+ (50, 10, and 7.1, respectively) to increase the probability of abnormal spirometry at school age [9]. Similar findings were later found in a cohort of 220 preschool children followed from the age of 4 years with IOS in which it was demonstrated that the increase in preschool R5 was associated with active asthma and impaired lung function at age 8 years [10].
Conclusion
IOS in pediatric asthma used from preschool age can predict loss of control, exacerbations, and deterioration of lung function in the short and medium term.
References
- McDowell KM (2019) Recent Diagnosis Techniques in Pediatric Asthma: Impulse Oscillometry in Preschool Asthma and Use of Exhaled Nitric Oxide. Immunol Allergy Clin North Am 39(2): 205-219.
- King GG, Bates J, Berger KI, Calverley P, de Melo PL, et al. (2020) Technical standards for respiratory oscillometry. Eur Respir J 55(2): 1900753
- Kaminsky DA, Simpson SJ, Berger KI, Calverley P, de Melo PL, et al. (2022) Clinical significance and applications of oscillometry. Eur Respir Rev 31(163): 210208.
- Gupta N, Sachdev A, Gupta D, Gupta S (2020) Oscillometry - The future of estimating pulmonary functions. Karnataka Paediatr J 35(2): 79-87.
- Galant SP, Fregeau W, Pabelonio N, Morphew T, Tirakitsoontorn P (2020) Standardized IOS Reference Values Define Peripheral Airway Impairment-Associated Uncontrolled Asthma Risk Across Ethnicity in Children. J Allergy Clin Immunol Pract 8(8): 2698-2706.
- Gochicoa-Rangel L, Martínez-Briseño D, Guerrero-Zúñiga S, Contreras-Morales J, Arias-Jiménez D, et al. (2023) Reference equations using segmented regressions for impulse oscillometry in healthy subjects aged 2.7-90. ERJ Open Res 9(6): 00503-2023.
- Ling Y, Si M, Niu Y, Han Y, Xu Y (2021) The predictive value of impulse oscillometry for asthma exacerbations in childhood: A systematic review and meta-analyses. Pediatr Pulmonol 56(7): 1850-1856.
- Lin LM, Chang YJ, Yang KD, Lin CH, Chien JW, et al. (2022) Small Airway Dysfunction Measured by Impulse Oscillometry and Fractional Exhaled Nitric Oxide Is Associated with Asthma Control in Children. Front Pediatr 10: 877681.
- Grell AV, Vera RG, Yarur AM, Castro-Rodriguez JA, Montenegro MAP, et al. (2023) Impulse oscillometry in preschool children with persistent asthma can predict spirometry at school age. Pediatr Pulmonol 58(5): 1411-1416.
- Knihtilä HM, Stubbs BJ, Carey VJ, Laranjo N, Zeiger RS, et al. (2024) Preschool impulse oscillometry predicts active asthma and impaired lung function at school age. J Allergy Clin Immunol 18: S0091-6749(24)00034-4.






























