Endocrine Dysregulation in Case of Chronic Obstructive Pulmonary Disease (COPD) – A Systemic Review
Avishek Das1*, Avisek Banerjee1, Tapas Kumar Chaudhuri2 and Pokhraj Guha3
1Department of Zoology, Ramkrishna Mission Vidyamandira, India
2Department of Zoology, University of North Bengal, India
3Department of Zoology, Garhbeta College, India
Submission: February 22, 2024; Published: April 02, 2024
*Corresponding author: Avishek Das, Assistant Professor, Department of Zoology, Ramkrishna Mission Vidyamandira, Belur Math, Howrah, West Bengal, 711202, India
How to cite this article: Avishek Das*, Avisek Banerjee, Tapas Kumar Chaudhuri and Pokhraj Guha. Endocrine Dysregulation in Case of Chronic Obstructive Pulmonary Disease (COPD) – A Systemic Review. Int J Pul & Res Sci. 2024; 7(2): 555707. DOI: 10.19080/IJOPRS.2024.07.555707
Abstract
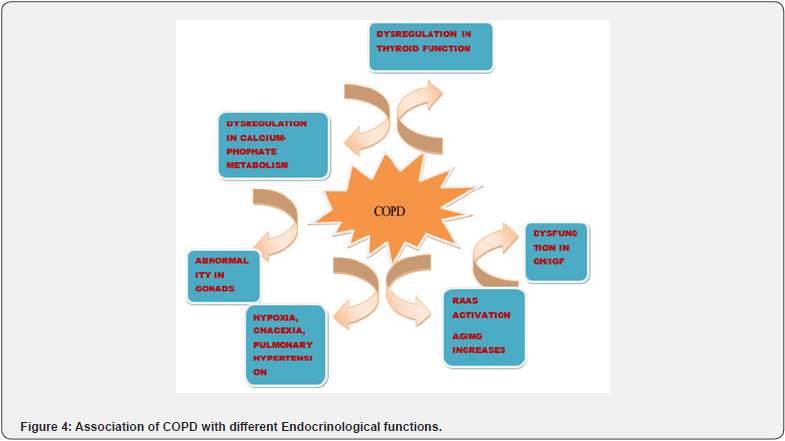
In this comprehensive overview, we delve into the limited understanding of endocrinological disturbances in Chronic Obstructive Pulmonary Disease (COPD), highlighting an elevated risk of specific endocrinopathies within the hypothalamic-pituitary-gonadal axis. Beyond its conventional characterization as a pulmonary inflammatory condition, COPD intricately involves multiple endocrine glands, including the thyroid, adrenal, pancreas, gonads, and pituitary. The secretion of endocrine hormones from these diverse tissues not only mirrors specific responses but also manifests nonspecific reactions associated with COPD diagnosis. A noteworthy observation is the dynamic modulation of growth hormone levels throughout the course of COPD. While some instances reveal a decrement in growth hormone concentration, others exhibit a nonspecific response marked by elevated levels. Altered thyroid hormone levels, coupled with weight loss and cachexia, emerge as characteristic features of COPD. Furthermore, the decline in testosterone and estrogen during hypoxemia is a common occurrence, leading to prevalent hypogonadism in both male and female COPD patients. The intricate interplay of Vitamin D and parathyroid hormones is also disrupted in COPD, consequently impacting calcium and phosphate homeostasis. Notably, the renin-angiotensin-aldosterone system undergoes significant upregulation in the course of COPD, contributing to secondary erythrocytosis and maintaining fluidic balance. The level of angiotensin-converting enzyme, a key player in pulmonary hypertension, is implicated in the COPD pathophysiology. Despite these insights, a critical gap remains in the identification of targeted medications for COPD management. This review underscores the imperative for further investigations to unravel the intricate correlations between various endocrine factors and their associations with COPD. Such endeavors hold the potential to pave the way for precision medication strategies tailored to address the multifaceted endocrine disturbances in COPD patients, thereby advancing therapeutic interventions in this complex respiratory condition.
Keywords: Chronic obstructive pulmonary disease; Cachexia; Hypogonadism; Renin- angiotensin-aldosterone system; Pulmonary hypertension
Abbreviations: COPD): Chronic Obstructive Pulmonary Disease; FVC: Forced Vital Capacity; FGF23: Fibroblast Growth Factor 23; IGF-1: Insulin Like Growth Factors; RAAS: Renin-Angiotensin- Aldosterone system; ACE: Angiotensin Converting Enzyme; GH: Growth Hormone; TSH: Thyroid-Stimulating Hormone; BMR: Basal Metabolic Rate; PTH: Parathyroid Hormone
Introduction
Chronic obstructive pulmonary disease (COPD) is a poorly reversible, slowly progressing with long asymptomatic lung disease characterized by airflow obstruction and it is a leading cause of morbidity as well as mortality throughout the world [1,2]. The major determinant of COPD susceptibility is cigarette smoking in urban areas [3]. Different genetic variants have been associated with the susceptibility of COPD [4]. The global population-based study indicates that the prevalence of COPD in the population less than 40 years of age is 10% and will remain a major public health problem. The major diagnosis procedure of COPD is made by measuring volume of air forcibly expired from total lung capacity (FEV1) by the forced vital capacity (FVC). Ratio of FEV1/FVC when it is <70% then COPD is said to be present in the patient and assigned to mild (Global initiative for COPD 1), moderate (GOLD2), severe (GOLD3) and very severe (GOLD4) (www.goldcopd.org) [5,6]. According to the American thoracic society COPD can be define as chronic bronchitis and emphysema where chronic bronchitis is characterized by excessive cough and sputum production and emphysema means chronic dyspnea, enlarged air spaces and destruction of lung tissue [7].
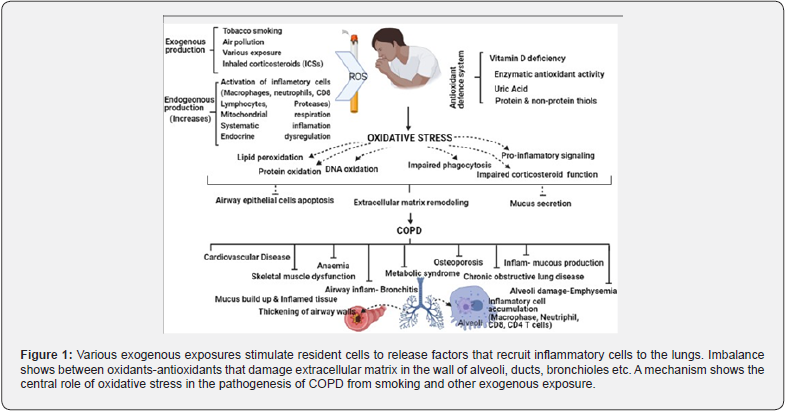
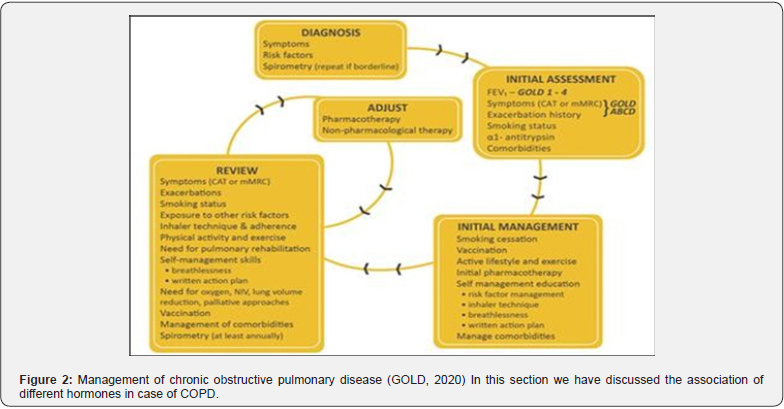
The persistent inhalation of different toxic particles by tobacco smoking, polluted air, exhaust gases from engine and others are the major risk factors for COPD. The airborne particles <0.5μm in diameter are 1000 times larger than oxygen molecules (Figure 1). These particles are likely to deposit in the transitional region of airways because they are unable to diffuse deeper into the alveolar air spaces. So terminal bronchioles are destroyed first rather than respiratory bronchioles because they receive higher dose of particulates [8]. In this study we have focused the endocrine dysregulation in case COPD. Different endocrine hormones play a vital role in the diagnosis. Patients with COPD are commonly hypoxemic and hypercapnic and also receive a high dose of glucocorticoids which may alter the endocrine function. The abnormal endocrine function including loss of control of breathing, decrease in muscle mass impaired cardiac function and fluidic balance in the body (Figure 2) [9]. In this section we have discussed the association of different hormones in the case of COPD.
Growth Hormone and COPD
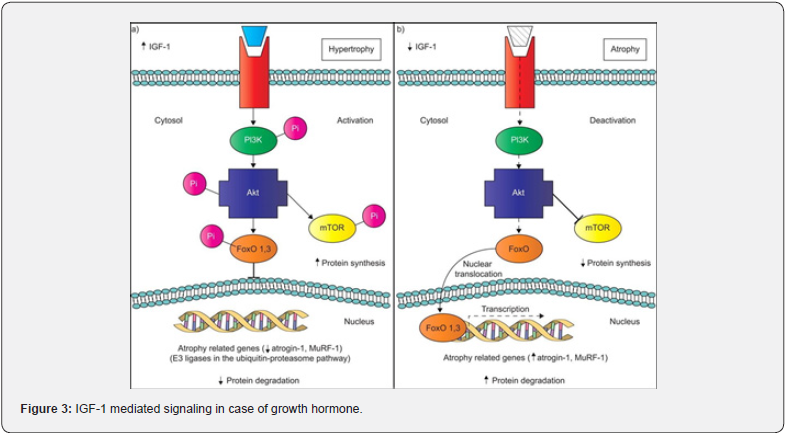
Growth hormones are responsible for muscle growth and its development. It is also increasing the level of insulin like growth factors (IGF-1). In case of COPD constant use of systemic corticosteroid is known to down-regulate the growth hormone synthesis [10]. During the course of chronic obstructive pulmonary disease, the levels of growth hormone and IGF-1 tend to be low in the patient. Some studies also reflected the increase of GH concentration in the blood which may be due to the nonspecific response of the body (Figure 2) [11]. Administration of GH in COPD patient increases muscle mass and function [12]. According to Karametos et al. [13] COPD is associated with the aging process. It accelerates the aging process in the patients suffering from COPD and the level of GH becomes very much low. The concentration difference of GH between COPD and control subjects was 0.42ng/ml as documented by Karametos et al. [13] It indicates that the biological age of the COPD patients was 13.1 on an average older of the same age when compared with the control subjects [13]. So, COPD influences the premature aging of patients (Figure 3).
Thyroid Hormone and COPD
Thyroid hormones mainly regulate the metabolism and thermogenesis in our body. Impairment of the thyroid hormone potentially influences the energy balance in the body. Hypermetabolism is commonly associated with COPD in case of resting position also. Insufficient diet and COPD cause a negative energy balance and weight loss in the patients [14,15]. It has been found that there is a strong correlation between T3/T4 ratio and arterial oxygen tension in the case of COPD patients [16]. The dysfunctions of thyroid gland in case of COPD leads to poor quality of life, cardiac dysfunction and also increase the frequency of exacerbation and mortality among the patients [17].
In general population, the prevalence of hypothyroidism ranges from 4.8% in female and 0.9% in male and the frequency of hypothyroidism increase with age [18,19]. It has been found that patients with hypothyroidism have low blood oxygen pressure and high carbon dioxide pressure in the blood [20]. Some of the frequent characteristics have been described in COPD patients due to hypothyroidism like shortening of the length of sarcomere and increase in number of mitochondria [21]. It has been documented that not only hypothyroidism but also hyperthyroidism play a critical role among the patients suffering from COPD. Dyspnea and hyperventilation are common symptoms during hyperthyroidism. It also increases the hypoxic drive and hypercapnic drive in the patients [22].
Gonadal Hormone and COPD
Male testosterone hormone production is stimulated by luteinizing and follicle stimulating hormone produced in the pituitary gland. Testosterone is recognized as an anabolic product signaling through androgen binding receptors in the cells. This hormone is responsible for the synthesis of actin and myosin molecules for muscle formation. Most of the testosterone present as the bound state in the body. The declining concentration of testosterone and oestrogen are associated with the aging process due to the changes in hypothalamic pituitary-gonadal axis both in case of male and female. It has been found that in case of female, testosterone level falls before menopause and declines further in post menopause session [23]. Hypogonadism, mainly associated with hypoxaemia, is also related to COPD. Many patients with hypoxaemia are related with decrease concentration of testosterone in their body [24]. In another study it has been found that patients with COPD who were given corticoids have decreased level of testosterone [25].
Calcium- Phosphate Regulatory Hormones and COPD
Fibroblast growth factor 23 (FGF23) is responsible for regulating the phosphate concentration in the body and lowering the 1.25-dihydroxy vitamin D. In case of the patients with chronic COPD may alter the phosphate metabolism. Phosphate dysregulation in the body also alters the concentration of parathyroid hormone [26]. Vitamin D may be considered as a possible biomarker for COPD as evident. The lower concentration of vitamin D is associated with faster fev1 decline rate and higher risk of COPD development [27]. The elevated level of parathyroid hormone is independently associated with COPD in the patients [28].
Renin-Angiotensin- Aldosterone System (RAAS) and COPD
According to Zeng et al. [29] the level of plasma renin activity, angiotensin I and II and aldosterone levels are higher in case of COPD patients when compared with healthy subjects. The activation of RAAS increases significantly in COPD patients [29]. According to Vlahakos et al. [30] activation of RAAS pathway is associated with high level of secondary erythrocytosis in patients suffering from COPD [30]. The development of pulmonary hypertension in COPD patients is caused due to the activation of angiotensin converting enzyme (ACE) pathway. The serum level of ACE is significantly higher in COPD patients when compared to the normal healthy population [31]. In one of the meta-analysis, it is evident that ACE gene insertion/deletion polymorphism is not associated with the risk of developing COPD [32].
Discussion
Chronic obstructive pulmonary disease (COPD) stands as a significant global health challenge, characterized by inflammatory lung pathology and escalating mortality rates worldwide [33]. Despite advancements in medical understanding and treatment modalities, COPD continues to burgeon, particularly in developed nations as documented by the Global Initiative for Chronic Obstructive Lung Disease (GOLD, www.goldcopd.org). Notably, smoking cessation remains the primary preventive measure against COPD, although occupational exposures to chemicals and pollutants also contribute significantly to its pathogenesis [34]. The insidious nature of COPD often results in a protracted asymptomatic phase, with patients often seeking medical attention only in the advanced stages of the disease. The inflammatory cascade within the bronchial tree and pulmonary parenchyma leads to progressive tissue destruction, culminating in the loss of lung elasticity characteristic of emphysema. Consequently, air trapping occurs within the lungs, exacerbating dyspnea and ultimately precipitating hypoxemia in advanced stages of the disease.
Pulmonary hyperventilation, as previously discussed [2], emerges as a hallmark characteristic of COPD, contributing to the ventilatory impairment observed in affected individuals. This multifaceted interplay of inflammatory processes, structural alterations, and ventilatory dysfunction underscores the complex pathophysiology of COPD and highlights the critical need for comprehensive management strategies targeting both its symptomatic and disease-modifying aspects. The intricate network of endocrine glands plays a pivotal role in orchestrating various physiological functions, encompassing metabolism, muscle development, calcium-phosphate regulation, gonadal development, and electrolytic balance within the human body. Growth hormone (GH), emanating from the pituitary gland, is integral to muscle growth and overall bodily movement. Intriguingly, early-onset Chronic Obstructive Pulmonary Disease (COPD) has been associated with diminished GH concentrations, precipitating weight loss, muscle protein depletion, and impaired mobility. Moreover, a noteworthy correlation emerges between GH levels and age, necessitating targeted supplementation to ameliorate muscle function in affected individuals.
The thyroid hormones, encompassing T3/T4 and thyroid-stimulating hormone (TSH), wield influence over metabolism, basal metabolic rate (BMR), and the metabolism of carbohydrates, fats, and proteins. In COPD, thyroid dysfunction becomes a chronic manifestation, contributing to weight loss and insufficient thyroid hormone levels. The concomitant development of hypoxemia and hypercapnia further exacerbates the condition, demanding precise medication to restore thyroid function. Hypoxemia, a hallmark of COPD onset, instigates a decline in testosterone and estrogen levels, fostering hypogonadism in both male and female patients. This, coupled with the administration of corticoids during COPD treatment, accelerates the aging process and leads to reduced sex hormone levels. The intricate interplay of these factors underscores the need for vigilant hormonal management in COPD patients.
Vitamin D and parathyroid hormone (PTH) jointly regulate calcium/phosphate balance in bodily fluids. Lower vitamin D levels have been associated with increased COPD prevalence, while elevated PTH levels in COPD patients contribute to heightened blood calcium levels and subsequent bone disruption in later life. The Renin-Angiotensin-Aldosterone System (RAAS), crucial for fluid balance, undergoes heightened activation in COPD patients. The elevated angiotensin-converting enzyme (ACE) levels in these patients not only serve as potential markers for COPD detection but also contribute to secondary erythrocytosis, modulating red blood cell count to regulate oxygen concentration during hypoxemia (Figure 4). This multifaceted interplay underscores the significance of understanding endocrine disruptions in COPD for developing targeted therapeutic interventions [35,36].
Conclusion
It is complicated and still unclear about the proper medication for the treatment of COPD. Lack of awareness is also a major factor for the development of the disease. Not only smoking but also pollution, especially in the urban areas, drastically affects the advancement of the disease by modifying our physiology. The endocrine function associated with COPD is needed to be focused and to be studied thoroughly to understand their role in case COPD. Inter relation of these hormones may relate with each other and proper correlation between them is very important for the study of COPD.
References
- Busch R, Brian DH, Jin Z, Peter JC, MJ McGeachie, et al. (2017) Genetic association and risk scores in a chronic obstructive pulmonary disease meta-analysis of 16707 subjects. Am J Respir Cell Mol Biol 57(1): 35-46.
- Devine JF (2008) Chronic obstructive pulmonary disease: an overview. Am Health Drug Benefits 1(7): 34-42.
- Ingebrigsten T, Simon FT, Jørgen V, Sophie VS, Kirsten OK, et al. (2010) Genetic influences on chronic obstructive pulmonary disease- a twin study. Respir Med 104(12): 1890-1895.
- Welter D, J MacArthur, Joannella M, Tony B, Peggy H, et al. (2014) The NHGRI GWAS catalog, a curated resource of SNP- trait associations. Nucleic Acid Res 42(Database issue): D1001-D1006.
- Global initiative for chronic obstructive lung disease (GOLD) (2009) Global strategy for the diagnosis, management, and prevention of Chronic obstructive pulmonary disease.
- Global initiative for chronic obstructive lung disease (GOLD) (2020) Global strategy for the diagnosis, management, and prevention of Chronic obstructive pulmonary disease.
- (1995) Standards for the diagnosis and care of patients with Chronic obstructive pulmonary disease. American Thoracic society. Am J Resp Crit Care Med 152(5 Pt 2): S77-S121.
- Hogg L, Amy G, Rachel G, Helen F (2012) People with COPD perceive ongoing, structured and socially supportive exercise opportunities to be important for maintaining an active lifestyle following pulmonary rehabilitation: a qualitative study. J Physiother 58(3): 189-195.
- Laghi F, N Adiguzel, MJ Tobin (2009) Endochrinological derangements in COPD. Eur Respir J 34(4): 975-996.
- Gayan-Ramirez G, F Vanderhoydonc, G Verhoeven, M Decramer (1999) Acute treatment with corticosteroids decreases IGF-1 and IGF-2 expression in the rat diaphragm and gastrocnemius. Am J Respir Crit care Med 159(1): 283-289.
- Mador MJ, E Bozkanat (2001) Skeletal muscle dysfunction in chronic obstructive pulmonary disease. Respir Res 2(4): 216-224.
- Creutzberg EC, Casaburi R (2003) Endocrinological disturbance in chronic obstructive pulmonary disease. Eur Respir J Suppl 46: 76s- 80s.
- Karametos I, Paraskevi T, Ilias T, Chrisi H, Grigorios G, et al. (2019) Chronic obstructive pulmonary disease as a main factor of premature aging. Int J Environ Res Public Health 16(4): 540.
- Creutzberg EC, AM Schols, FC Bothmer-Quaedvlieg, EF Wouters (1998) Prevalence of an elevated resting energy expenditure in patients with chronic obstructive pulmonary disease in relation to body composition and lung function. Eur J Clin Nutr 52(6): 396-401.
- Schols AMWJ, PB Soeters, R Mostert, WH Saris, EF Wouters (1991) Energy balance in chronic obstructive pulmonary disease. Am Rev Respir Dis 143(6): 1248-1252.
- Dimopoulou I, I Ilias, G Mastorakos, E Mantzos, C Roussos, et al. (2001) Effects of severity of chronic obstructive pulmonary disease on thyroid function. Metabolism 50(12): 1397-1401.
- Chaudhary SC, Tauhid A, Kauser U, Kamal KS, Kamlesh KG, et al. (2018) Prevalence of thyroid dysfunction in chronic obstructive pulmonary disease patients in a tertiary care center in North India. J Family Med and Prim care 7(3): 584-588.
- Bjoro T, J Holmen, O Krüger, K Midthjell, K Hunstad, et al. (2000) Prevalence of thyroid disease, thyroid dysfunction and thyroid peroxidase antibodies in a large, unselected population. The health study of North – Tron- delag (HUNT). Eur J Endochrinol 143(5): 639-647.
- Morganti S, GP Ceda, M Saccani, B Milli, D Ugolotti, et al. (2005) Thyroid disease in the elderly: sex- related differences in clinical expression. J Endochrinol Invest 28(11 Suppl Proceedings): 101-104.
- Terzano C, S Romani, G Paone, V Conti, F Oriolo (2014) COPD and thyroid dysfunction. Lung 192: 103-109.
- Orozco-Levi M, J Gea, JL Lloreta, M Félez, J Minguella, et al. (1999) Subcellular adaptation of the human diaphragm in chronic obstructive pulmonary disease. Eur Respir J 13(2): 371-378.
- Dymanowska JM, AJ Białas, Paulina L, Paweł G, Wojciech JP (2017) Thyroid gland in chronic obstructive pulmonary disease. Adv Respir Med 85(1): 28-34.
- Booij A, CM Biewenga-Booji, O Huber-Bruning, C Cornelis, JW Jacobs, et al. (1996) Androgens as adjuvant treatment in postmenopausal female patients with rheumatoid arthritis. Ann Rheum Dis 55(11): 811-815.
- Semple PD, GH Beastall, WS Watson, R Hume (1980) Serum testosterone depression associated with hypoxia in respiratory failure. Clin Sci 58(1): 105-106.
- Kamischke A, DE Kemper, MA Castel, M Lüthke, C Rolf, et al. (1998) Testosterone in men with chronic obstructive pulmonary disease with or without glucocorticoids therapy. Eur Respire J 11(1): 41-45.
- Stroda A, Vincent B, Ayham D, Christian C, Claudia G, et al. (2018) Serum phosphate and phosphate regulatory hormones in COPD patients. Respir Res 19(1): 183.
- Afzal S, Peter L, Stig EB, Jacob JF, Børge GN (2014) Plasma 25- hydroxyvitamin D, lung function and risk of chronic obstructive pulmonary disease. Thorax 69(1): 24-31.
- Park JH, Hye KP, Hoon J, Sung-Soon L, Hyeon-Kyoung K, et al. (2015) Parathyroid hormone as a novel biomarker for chronic obstructive pulmonary disease: Korean national Health and Nutrition examination survey. Plos One 10(9): e0138482.
- Zeng GB (1989) The renin- angiotensin- aldosterone system changes in chronic obstructive pulmonary disease. Article in Chinese 12(5): 265-267.
- Vlahakos DV, EN Kosmas, I Dimopoulou, E Ikonomou, G Jullien, et al. (1999) Association between activation of the renin- angiotensin system and secondary erythrocytosis in patients with chronic obstructive pulmonary disease. Am J Med 106(2): 158-164.
- Toru U, Ceylan A, Osman G, Server S, Özlem A, et al. (2015) Circulating levels of IGF-1 and IGFBP-3 in patients with COPD. Eur Respir J 46: PA4810.
- Xu G, Guohui F, Yingtong S, Lili Y, Sinan W, et al. (2018) Association of angiotensin- converting enzyme gene I/D polymorphism with chronic obstructive pulmonary disease. JRAAS 19(2): 1470320318770546.
- Murrey CJ, Lopez AD (1997) Global mortality, disability, and the contribution of risk factors: Global burden of disease study. Lancet 349(9063): 1463-1442.
- National heart (2006) lung and blood institute. National institute of health. COPD essentials for health professionals.
- Skabby T, Lise LNH, Betina HT, Charlotta P, Torben J, et al. (2014) Vitamin D status and chronic obstructive pulmonary disease: A prospective general population study. Plos One 9(3): e90654.
- JM Sacheck, Akira O, SC McLary, Alfred LG (2004) IGF-1 stimulates muscle growth by suppressing protein breakdown and expression of atrophy- related ubiquitin ligases, atrogin-1 and MuRF1. Am J Physiol Endocrinol Metab 287(4): E591-E601.






























