Evaluation of Factors Associated with the COVID-19 Vaccine Acceptance in Nigeria
Francis Enenche Ejeh1*, Deborah Maigawu Buba2, Rine Christopher Reuben3, Saleh Mohammed Jajere4, Ballah A Denue5, Bashir Usman Malgwi4 and Sarah Adamma Abunike6
1Department of Veterinary Microbiology, University of Maiduguri, Nigeria
2Department of Veterinary Microbiology and Pathology, University of Jos, Nigeria
3German Centre for Integrative Biodiversity Research (iDiv), Germany
4Department of Veterinary Public Health and Preventive Medicine, University of Maiduguri, Nigeria
5Department of Medicine, College of Medical Sciences, University of Maiduguri, Nigeria
6Institute for Health and Equity, Medical College of Wisconsin, USA
Submission: January 02, 2024; Published: February 01, 2024
*Corresponding author: Francis Enenche Ejeh, Department of Veterinary Microbiology, University of Maiduguri, Nigeria
How to cite this article: Francis Enenche Ejeh*, Deborah Maigawu Buba, Rine Christopher Reuben, Saleh Mohammed Jajere, Ballah A Denue, Bashir Usman Malgwi and Sarah Adamma Abunike. Evaluation of Factors Associated with the COVID-19 Vaccine Acceptance in Nigeria. Int J Pul & Res Sci. 2023; 7(1): 555702. DOI: 10.19080/IJOPRS.2023.07.555702
Abstract
Achieving complete control over the COVID-19 pandemic hinges on two critical factors: widespread access to vaccines and public acceptance of their use. Understanding the nuances of vaccine acceptance within specific populations is crucial for designing effective vaccination campaigns. We conducted a comprehensive study to evaluate the determinants of COVID-19 vaccine acceptance among Nigerian adults from March 2021 till December 2021. Data collected were analyzed using descriptive statistics, Chi-square, and multivariable regression. We found a positive relationship between respondents’ COVID-19 knowledge and their willingness to accept COVID-19 vaccines. Overall, COVID-19 knowledge was good, with a mean score of 6.2±0.19 (range 0-8). The COVID-19 vaccine acceptance rate was 65.67%. Our comparisons of respondents’ age groups and marital status revealed higher odds of being willing to accept COVID-19 vaccines among respondents who were age 50 ≥ years old (aOR 7.35; 95% CI: 1.69-31.93; p = 0.008) and those who were singles (aOR 4.39; 95% CI: 1.86-10.33; p = 0.001), respectively. However, non-healthcare workers with high income and educational status were unwilling to accept COVID-19 vaccines. The intention to receive the COVID-19 vaccine varied across demographic characteristics, level of education, income, and employment status. We recommend continuous public health education on vaccination’s vital role in ending the COVID-19 pandemic.
Keywords: Infectious diseases; Coronavirus; Preventive medicine; Vaccine hesitancy; COVID-19 pandemic
Abbreviations: IPC: Infection Prevention and Control; WHO: World Health Organization; FCT: Federal Capital Territory; FDA: Food and Drug Administration; EMA: European Medicines Agency; MHRA: Medicines and Healthcare Regulatory Agency; Africa CDC: Africa Centers for Disease Control and Prevention; OR: Odds Ratio; CI: Confidence Interval; PhD: Doctor of Philosophy degree; SSCE: Senior Secondary School Certificate; NHWs: Non-Healthcare Workers; HCWs: Healthcare Workers; HCWs: Healthcare Workers; NPHCDA: Nigerian National Primary Healthcare Development Agency
Background
The coronavirus disease 2019 (COVID-19) pandemic has brought all nations on earth to their knees. The pandemic was so severe that humanity had taken measures contrary to the philosophy of the human fraternity and coexistence for the first time in history. Instead of fostering the “together, we stand” cliché globally upheld for decades, humanity would soon advocate for “separated we live,” which enabled social distancing and travel restriction among nations, regions, and territory. Just as it is often said, “hard times require desperate measures”, same with the approach scientists and political leaders adopted in combating the COVID-19 pandemic.
These include the prompt production and approval of different COVID-19 vaccines for emergency human use without the traditional rigorous testing and trials and the implementation of the Public Readiness and Emergency Preparedness Act with immunity from liability for the COVID-19 vaccines [1-4]. Other drastic measures that were taken to stop the spread of SAR-COV-2 included the initial lockdown of worship centers, markets, theatres, bars, clubs, the prohibition of crowd gathering, the enforcement of the use of facemask, hand washing and social distancing [5] Initially, the Nigerian masses complied with the infection prevention and control (IPC) measures enacted by the Federal Ministry of Health as well as other global health organizations including the World Health Organization (WHO). However, sustaining these measures for an extended period was no longer possible.
By and large, the successful administration of effective, safe and sustainable vaccines across the globe is widely believed to be crucial in mitigating and preventing the COVID-19 pandemic [6]. To this end, there has been an urgent need to rapidly design, develop and manufacture vaccines that be massively used as a practical tool to end the pandemic since no pharmaceutical interventions has been discovered yet. However, the production of vaccines against SARS-COV-2 was the fastest in the history of vaccinology [7]. Within one year of the emergence of COVID-19, COVID-19 vaccines were developed. Some had been approved by the relevant government regulatory agencies such as the Food and Drug Administration (FDA) of the United States, the European Medicines Agency (EMA), The United Kingdom’s Medicines and Healthcare Regulatory Agency (MHRA), and also the National Agency for Food and Drug Administration and Control of the Federal Republic of Nigeria [8].
The acceptability of COVID-19 vaccines by the public is crucial for eliminating this deadly pandemic. In separate studies conducted in Nigeria, Reuben et al. [9] and Adigwe [7] reported low COVID-19 acceptance of 29.0% and 22.7% among residents of northcentral Nigeria and the Federal Capital Territory (FCT), Abuja, respective. In the same vein, although 55.5% COVID-19 acceptance were among health care workers in the southwest and south-south geopolitical zones of Nigeria [10], a lower rate, 40.0%, was however reported among medical students in the Northwestern geopolitical zone in Nigeria [11].
The rapid assessment of information regarding COVID-19 vaccines acceptance among individuals across Nigeria amidst the current COVID-19 pandemic is necessary and crucial in aiding and speeding up vaccination appraisal, monitoring, re-planning, and implementation of behavior change programs/campaigns to increase vaccine acceptance and coverage, which are vital to mitigating COVID-19. The study aimed to evaluate the factors associated with COVID-19 vaccine acceptance among healthcare workers in Nigeria.
Materials and Methods
Study design and participants
We used a non-repeated cross-sectional design to evaluate the COVID-19 risk perception and factors associated with accepting the COVID-19 vaccine in Nigeria, West Africa. The study was from March 2021 to December 2021. The methods used in this study and the questionnaire have been previously published [12,13]. Participants were adults who were twenty years and above and were residents in Nigeria. Google form was used to communicate the questionnaire web link to the target participants. Social media platforms such as WhatsApp, Twitter, Facebook, and Instagram were used to reach participants. A brief description was included in the introduction. The submitted answered questionnaire was considered consent to participate in the study. As described in our previous study, the questionnaire was pre-evaluated for consistency and error [14]. The reliability coefficient was calculated using SPSS v.20. The value of Cronbach’s alpha was found to be 0.7. The data from the pilot study was not included in the final data analysis. We recruited four thousand target participants via social media. Four hundred and two (402) participants accepted and completed the questionnaires.
Ethical permit and consent note
The research ethics committee of the Borno State Hospital Services, Ministry of Health, Maiduguri, Nigeria, approved our study protocol (MHSEC/03/2020/00022). The submission of the online answer to the questionnaire was considered as consent to take part in the study. A consent note was not needed.
The Measures
The survey instrument used in this study was based on the tool designed by Municipal Public Health Service Rotterdam-Rijnmond (GGD) together with the National Institute for Public Health and the Environment (RIVM) in the Netherlands [12] with minimal modification. Previous studies consulted included [14], course material regarding coronavirus disease outbreaks, including the current COVID-19 pandemic by WHO [15], and guidelines issued by Africa Centers for Disease Control and Prevention (Africa CDC) [16]. The questionnaire consisted of four (4) parts:
Demographic characteristics of respondents.
Participants were asked to report their age, sex, state of residence, occupation, educational level, marital status, household size, income category, and employment status.
Knowledge of respondents on COVID-19.
This category included eight questions on the cause of COVID-19, transmission, prevention and control, myths, and symptoms. The knowledge questions consisted of dichotomous questions (correct, incorrect and unknown); a correct answer was scored 1 point while a wrong or unknown answer was scored 0 points. The total knowledge score ranged from zero to eight; the mean knowledge score of 0-4.99 was considered poor knowledge, and a mean score of 5-8 was deemed to be good knowledge of COVID-19.
Statistical analyses
We enter the data collected into Microsoft Excel and imported into SPSS version.20.0 for statistical analysis. Descriptive statistical methods were used to summarize data on socio-demographic characteristics and responses to questions regarding respondents’ knowledge on COVID-19, Perception of the seriousness, susceptibility to COVID-19 and perception of efficacy and self-efficacy to protect against the disease the intention to accept the COVID-19 vaccine in Nigeria. Data were summarized as categorical variables’ frequencies (n) and percentages (%). Furthermore, we presented the data in tables and graphs. Chi-square was used to figure out the level of difference among the categorical variables. A binary logistic regression analysis was applied and expressed as odds ratio (OR) and 95% confidence interval (CI) to figure out the predictors of COVID-19 vaccine acceptance. A p-value of less than 0.05 was considered significant in all tests.
Results
Demographic characteristics of study participants

The study included 402 participants from 47.2% (17/36) across all the states in Nigeria and the federal capital territory (Abuja). (Table 1) showed the demographic characteristics of the respondents, where the majority, 288 (71.6%) and 235 (58.5%), were males and married, respectively. Furthermore, 373 (67.9) and 249 (54.5%) were aged 20-39 and 5-10 person households. Although most of the respondents, 295 (73.38%) had either a bachelor, master or Doctor of Philosophy (PhD) degree, 107 (25.62%) had either senior secondary school certificate (SSCE) or Diploma/NCE certificates. Also, we had more 349 (86.8%) non-healthcare workers (NHWs) participation than the healthcare workers (HCWs) Respondents who earned less than 72.86USD (₦ 30,000) per month were 123 (30.6%) while those who made more than 947.18USD (₦390,000) were 33 (8.2%). The majority, 127 (31.6%) of the participants, were employees of the federal government of Nigeria.
Knowledge of participants towards COVID-19 and acceptance of COVID-19 vaccine
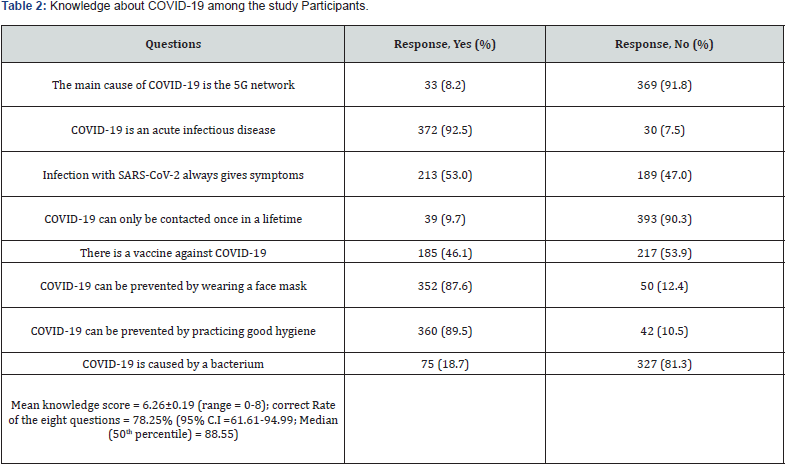
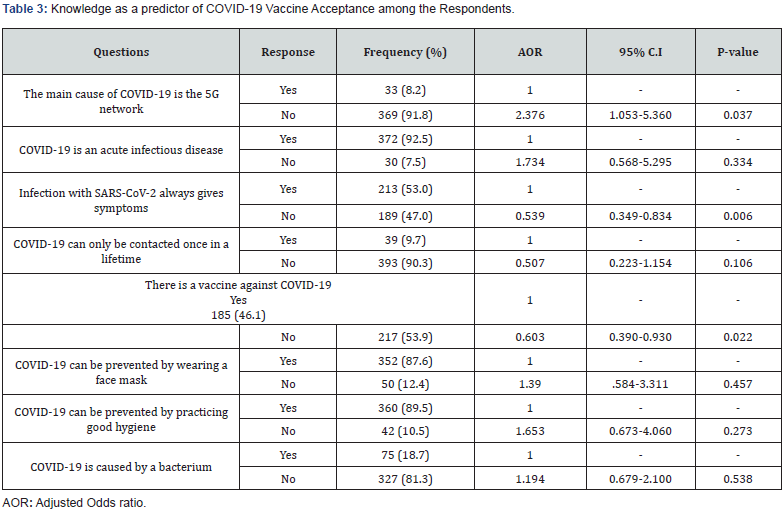
All the respondents agreed to have heard about COVID-19. The correct rate of the eight questions on the knowledge about COVID-19 was 78.25%±0.19 (95% CI =61.61-94.99), with the participants median or percentile rate of learning about COVID-19been 88.55%. The overall mean knowledge score of the participant was 6.26±0.19 (range = 0-8) (Table 2). Multivariate regression analysis of the respondent data revealed that respondents who believed that the 5G network is not the main cause of the COVID-19 were about two times more likely to accept the COVID-19 vaccines than those who believed that the 5G network was the cause of COVID-19 (OR = 2.376; 95%C.I = 1.053-5.360; P = 0.037). Respondents who opined the non-existence of COVID-19 vaccines were less likely to accept being vaccinated with the available COVID-19 vaccines (OR = 0.603; 95% C.I = 0.390-0.930; P = 0.022). However, respondents who believed COVID-19 is often asymptomatic were less likely to accept the COVID-19 vaccine than those who believed COVID-19 often shows symptoms (OR = 0.539; 95% C.I = 0.349-0.834; P = 0.006) (Table 3).
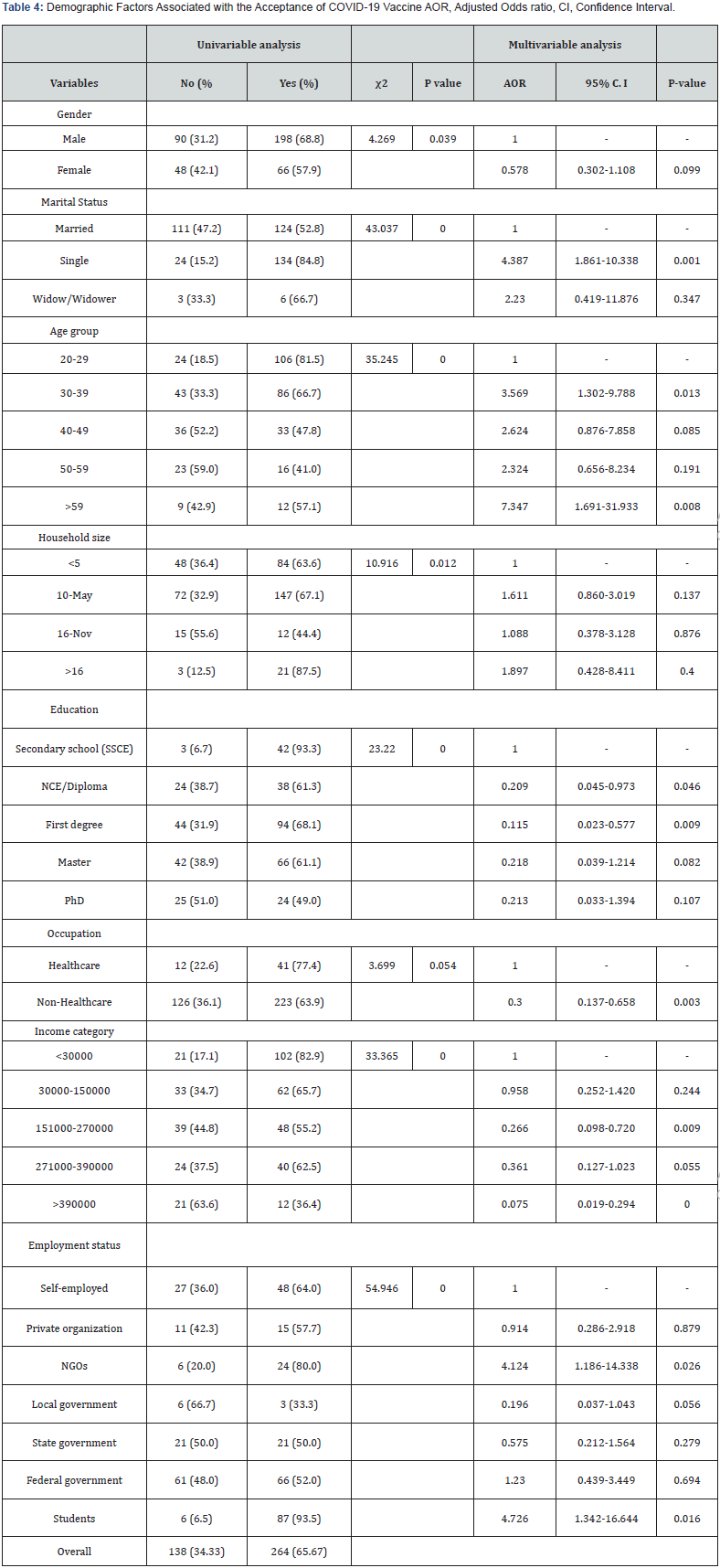
Demographic factors associated with the acceptance of COVID-19 Vaccine in Nigeria
Regarding demographic factors associated with the COVID-19 vaccine acceptance, 198 (68.8%) of the male had vaccine acceptance while females had 66 (57.9%). The difference between vaccine acceptance and gender was statistically significant (χ2 = 4.269; P = 0.039). Based on marital status, single and never married respondents had the highest (138 (84.8%)) COVID-19 vaccine acceptance rate. The difference in the acceptance of the COVID-19 vaccine with regards to marital status was statistically significant (χ2 = 43.047; p < 0.001). Also, respondents that were never married (singles) were more likely to accept the COVID-19 vaccine compared to the married (OR = 4.387; 95% C.I = 1.861-10.338; P = 0.001).
The acceptance of the COVID-19 vaccine was significantly (χ2 = 35.245; p < 0.001) different among the age groups. The age group 20-39 years had the highest percentage 106 (81.5%) of COVID-19 vaccine and were about four times likely to accept COVID-19 vaccine. Also, the age group fifty-nine years and above were about seven times likely (OR = 7.347; 95% C.I = 1.691-31.933; P = 0.008) compared with the age group 20-39 years. The acceptance of COVID-19 vaccine varies significantly (χ2 = 10.916; p = 0.012) among household size. Households with a family size of more than sixteen (16) had the highest percentage, 21 (87.5%) of COVID-19 vaccine acceptance, while household size less 11-16 had the least 12 (44.4%) acceptance.
The acceptance of COVID-19 vaccine differs significantly (χ2 = 23.220; p < 0.001) among the educational qualification. Respondents with secondary (high) school certificates had the highest percentage, 43 (93,.3%) COVID-19 vaccine acceptance, while respondents with the Doctor of Philosophy (PhD) had the lowest percentage, 24 (49.0%) COVID-19 vaccine acceptance. Respondents with the national certificate of education/diploma, Bachelor, Master, and PhD were less likely to accept the COVID-19 vaccine than respondents with secondary (high) school certificates (Table 4). Regarding occupation, healthcare workers (HCWs) had a higher percentage 41 (77.4%) COVID-19 acceptance, than non-healthcare workers (NHCWs) 223 (63.9%). Although, the differences were not statistically significant (χ2 = 3.699; p = 0.053), NHCWs were less likely to accept the COVID-19 vaccine (OR = 0.300; 95% C.I = 0.137-0.658; P = 0.003).
Regarding income categories, lower-income earners ($72.89USD (₦30000) per month) had the highest percentage 102 (82.9%) acceptance of COVID-19 vaccine, while the highest income earners (≥ $947.00USD (≥₦390000) per month) had the lowest percentage 12 (36.4%) acceptance of COVID-19 vaccine. The differences in COVID-19 vaccine acceptance among the income categories was statistically significant (χ2 = 35.365; p < 0.001). And respondent who earned the highest income were less likely to accept the COVID-19 vaccine (OR = 0.075; 95% C.I = 0.019-0.294; P ≥ 0.001). Concerning employment status, students had the highest percentage, 87 (93.5%), followed by the non-governmental organization (NGOs) 24 (80.0) while local government workers had the lowest percentage, 3 (33.3%) of COVID-19 vaccine acceptance. Students and NGOs workers were about four times and five times more likely to accept the corvid-19 vaccine than the self-employed (Table 4).
Discussion
COVID-19 Vaccine Acceptability among the Study Participants
The sustainable production of safe and viable vaccines is considered the foremost critical countermeasure to fight the COVID-19 and pivotal to lessening and mitigating the devastating health and socioeconomic impacts of the COVID-19 pandemic the world over [6]. However, the willingness of the population to accept the approved and available COVID-19 vaccines would significantly alter the epidemiological dynamics and the transmission of SARS-CoV-2 among the population.
Overall, our study recorded 65.67% (264/402) COVID-19 vaccine acceptance among the study participants. However, about one-third of the participants were hesitant or unwilling to accept COVID-19 vaccines. A substantial percentage of the Nigerian population needs to be vaccinated against COVID-19 to achieve herd immunity against COVID-19 disease. Being the most populous African country (with > 200 million people), the Nigerian National Primary Healthcare Development Agency (NPHCDA) has so far vaccinated only about 6 million people as at the time the article was developed and since COVID-19 vaccines became available [17]. The reasons for the low acceptance rate recorded in this study may be because of belief systems, misinformation and poor COVID-19 education [14,18]. In a similar multinational study assessing country-specific COVID-19 vaccines acceptance rate, Hawlader et al. [19] reported 74.0, 71.5, 65.7 and 65.0% COVI-19 vaccines acceptance rates in Nepal, Pakistan, India and Bangladesh, respectively. When comparing with our findings. Higher COVID-19 vaccine acceptance was reported in studies in Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%), China (91.3%) and Brazil (85.4%) [20-23]. Lower rates of 23.6%, 5.7%, 41.7% and 63.0%, were reported from Kuwait, Italy, Russia and the United Kingdom [24-27].
Globally, vaccine acceptance has been found to be a complex and multi-dynamic phenomenon, which often varies depending on the type of disease, place (country and region), time, community demographics, settings, and behavioral proclivities [19,25-27]. Furthermore, it is noteworthy that vaccine hesitancy in Nigeria is not exclusive to the current COVID-19 pandemic. An earlier vaccine coverage report in Nigeria showed only 53.3, 34.0, 41.8 and 39.0% vaccine coverage for tuberculosis, polio, measles and yellow fever, respectively [28]. Also, in an epidemiological survey during the initial national lockdown to curtail the spread of COVID-19 in April 2020, only 29.0% of the study population indicated their willingness to accept COVID-19 vaccines when available [24].
Knowledge about COVID-19 and Acceptance of the COVID-19 Vaccine
The level of COVID-19 knowledge is a major factor that is affecting the acceptability of the COVID-19 vaccine in Nigeria and globally. Our findings revealed that the mean knowledge score was high among the study population (mean 6.26±0.9; range = 0-8). The mean knowledge score obtained in this study was consistent with a previous study in Vietnam in which a 7.11 (0-9) mean knowledge score was reported among high-risk group [29]. Also, the values reported in this study were lower than in a previous study among healthcare workers in Nigeria [14]. The differences seen in this study may be because of the difference in the study population. By their level of knowledge regarding COVID-19, healthcare workers are more likely to be better informed about COVID-19 than the public.
Knowledge plays an essential role in the understanding of the COVID-19 pandemic threat. The study participants’ knowledge about the availability of the COVID-19 vaccine was poor. Only one hundred and eighty-five (46.1%) were aware of the availability of the COVID-19 vaccine at the time of collecting the data. Therefore, the general public should be continually educated through popular media such as social media and television [14] and other sources of information about COVID-19 [9,29,30].
This study revealed that the acceptance of the COVID-19 vaccine was affected by misinformation and poor knowledge. Participants that believed that the 5G network was the cause of the COVID-19 pandemic were less likely to accept the COVID-19 vaccine. Also, respondents who said that the COVID-19 always give symptoms and respondents who said there was no vaccine against COVID-19 were less likely to accept the vaccine. The emergence of COVID-19 was associated with immense misinformation, misgivings and mistrust regarding its epidemiology and transmission, pathogenesis and clinical manifestations, and control and prevention measures among the Nigerian population [9].
These undoubtedly contributed to increased information gaps, negative beliefs and mistrust in approved and available COVID-19 vaccines, generally expected in developing countries, including Nigeria. Although the Federal government has criminalized fake news and misinformation [31], there is a need better to counter misinformation regarding the COVID-19 vaccine and future pandemics. Criminalizing false information was regarded as suppressing freedom of expression. For example, Zambia, Zimbabwe, Uganda, Canada held that prohibiting fake news was unconstitutional violates the right to freedom of expression (Centre for Law and Democracy, 2021) [32]. However, in recent times, because of the COVID-19 pandemic, nations have passed amendments to their laws criminalizing fake news and misinformation (Centre for Law and Democracy, 2021). Pomeranz and Schwid [33] addressed the issues of COVID-19 misinformation by stating that “the goal of addressing COVID-19 misinformation is best served by protecting expression, disseminating factual information, ensuring strong protection for whistleblowers, and supporting independent media environment”.
Demographic Factors Associated with the Acceptance of COVID-19 Vaccine
Our study also explored the relationships between demographic factors with COVID-19 vaccine acceptance among the Nigerian population. We found an association between gender and vaccine acceptance. Unwillingness to take COVID-19 vaccines among females was higher than male participants. Our study identified the male gender as a positive predictor for COVID-19 vaccine acceptance, which agrees with many other studies globally [34-36]. In most Nigerian states, traditional patriarchal norms are the primary factor in creating a disparity in vaccine acceptance and coverage in Nigeria. Additionally, scientific evidence suggests higher risks for COVID-19 infection, complications and death among males [37-40]. This gender-based disparity in COVID-19 morbidity and mortality may have contributed to increased vaccine acceptance among males in Nigeria.
Our study also revealed marital status as a predictor for COVID-19 vaccine acceptance. Participants who were never married (single) or widow/widower were more likely to be vaccinated against COVID-19 than those married. Attitudes and perceived risks for a disease or health condition often differ with the status of relationships, which determines subsequent decisions for vaccine acceptance [41]. Although two separate studies found an association between COVID-19 vaccine acceptance and marital status, however, contrariwise, both studies found that married individuals were more interested in being vaccinated [42, 43].
Interestingly, individuals within the age group 20-39 years old were four times more likely to accept COVID-19 vaccines than other age groups. This corroborated a similar report showing negative attitudes toward COVID-19 vaccination among the ageing Bangladeshi population [42]. Although the ageing population is at considerable risk of COVID-19 complications, most of them are conservatives (often resorting to traditional treatment) whose perceptions of the COVID-19 pandemic and vaccine acceptability cannot be easily influenced. This may be a significant public health concern in developing countries since the ageing population is most vulnerable to COVID-19. Conversely, the older people in Hong Kong, Saudi Arabia and the USA showed a higher willingness for COVID-19 vaccine acceptance [23,43,44].
Our findings revealed that respondents from large household sizes were more willing to accept the COVID-19 vaccine than smaller households’ size. The reason may be because their fear of infecting other family members outweighs the perceived fear of the adverse effect that may result from the novel COVID-19 vaccine. This finding is consistent with an earlier study in which healthcare workers were concerned about infecting their family members [13]. Surprisingly, we found that participants with only higher educational qualifications (NCE/Diploma, first degree, master’s, and PhD) were less likely to be willing to be vaccinated against COVID-19 than those with only secondary school education. We supposed that due to the media overhype of the COVID-19 pandemic and associated misinformation, individuals with higher education could have been overly cautious of emerging concerns attributed to vaccines safety and post-vaccination adverse reactions related to COVID-19 vaccines [6,9].
Similar trends were previously reported in India and Pakistan [19]. In sharp contrast with our finding, several studies worldwide showed associations between higher educational qualification and COVID-19 vaccine acceptance [35,45-47]. This association is often supported by the argument that individuals with higher academic qualifications better understand COVID-19 and vaccinations than individuals with lower education [45]. Howbeit, our study disproved this famous claim despite population and region-specific studies are expected to yield divergent and community-specific outcomes. Therefore, there is a need to re-educate the educated elite in the study population about the COVID-19 pandemic and COVID-19 vaccine.
Compared with the general population (in this case, NHCWs), HCWs had more willingness to be vaccinated against COVID-19, as recorded in our study. Similar trends were reported in a regional survey involving six Asia-Pacific countries, including Bhutan, China, India, Indonesia, Singapore and Vietnam [48], as well as other separate studies in India [19], Canada [49], Hong Kong [50], France [51,52], and the USA [53]. The most important and independent factors often associated with COVID-19 vaccine hesitancy among HCWs include concerns regarding risks and safety [52]. Still and all, with increased clinical studies and the availability of additional public health information about COVID-19 vaccines risks and safety, vaccine acceptance over time may vary [49].
Furthermore, we found that participants with higher income were more likely to be unwilling to be vaccinated when compared with participants with lower income. In Nigeria, low-income earners are at an increased risk of contracting infectious diseases, including COVID-19 due to crowded living conditions and slums, poor personal and community hygiene, reliance on crowded public utilities including transport, their inability to access better healthcare services, and their increased tendency to continue regular work and business outside their homes [38,54]. Regarding employment status, students and NGOs workers were more likely to be willing to be vaccinated when compared with participants with other employment statuses. Since most students are young adults, this finding supports our earlier established relationship between youthful age and COVID-19 vaccine acceptance stated above [55-58].
Conclusion
Our results showed that the study participants had sound knowledge about COVID-19. However, the acceptance of the COVID-19 vaccine was poor. Several factors, including demographic characteristics such as old age, low income, single and student and NGO workers, were positive predictors of COVID-19 vaccine acceptance. In contrast, high income, high academic qualification, married, youthful age and poor knowledge of COVID-19 were associated with unwillingness to accept the COVID-19 vaccine. Continuous public health education and re-education of the target population sets with a low COVID-19 vaccine acceptance rate are needed to change their belief about COVID-19 and COVID-19 vaccine, improve vaccine acceptance and bring an end to the pandemic [59-61].
Ongoing public health enlightenment campaigns among the Nigerian population are necessary to improve their knowledge of COVID-19, assuage their fears and negative beliefs towards COVID-19, and boost their confidence and willingness to accept available COVID-19 vaccines. Increased COVID-19 vaccine acceptance within the population would significantly reduce transmission and severity of the disease hence, mitigating the pandemic.
Acknowledgements
The authors wish to acknowledge the support of Saidu Adamu for helping us with the dissemination of the online questionnaire.
References
- Sidebari L (2021) CRS Legal Sidebar Prepared for Members and Committees of Congress The PREP Act and COVID-19: Limiting Liability for Medical Countermeasures.
- The World Bank (2021) Development Committee, Joint Ministerial Committee of the Boards of Governors of the Bank and the Fund on the Transfer of Real Resources to Developing Countries.
- Halabi SF (2022) Solving the Pandemic Vaccine Product Liability Problem. UC Irvine Law Rev 12(1): 11.
- Mustapha K (2022) COVID-19 and medical liability in Nigeria: Where lies health workers’ immunity? | TheCable.
- Ejeh FE, Owoicho S, Saleh AS, Madukaji L, Okon KO (2021) Factors associated with preventive behaviors, anxiety among healthcare workers and response preparedness against COVID-19 outbreak: A one health approach. Clin Epidemiol Glob Heal 10: 100671.
- Reuben RC, Adogo LY (2021) SARS-CoV-2 vaccines–induced thrombotic thrombocytopenia: should we consider immuno-hypersensitivity? Rev Saude Publica 55: 70.
- Adigwe OP (2021) COVID-19 vaccine hesitancy and willingness to pay: Emergent factors from a cross-sectional study in Nigeria. Vaccine X 9: 100112.
- NAFDAC (2022) Covid-19 Vaccine Update - NAFDAC. 2021.
- Reuben RC, Danladi MMA, Saleh DA, Ejembi P (2020) Knowledge, Attitudes and Practices Towards COVID-19: An Epidemiological Survey in North-Central Nigeria. J Community Health 46(3): 457-470.
- Adejumo OA, Ogundele OA, Madubuko CR, Oluwafemi RO, Okoye OC, et al. (2021) Perceptions of the COVID-19 vaccine and willingness to receive vaccination among health workers in Nigeria. Osong Public Heal Res Perspect 12(4): 236-243.
- Mustapha M, Lawal BK, Sha’aban A, Jatau AI, Wada AS, et al. (2021) Factors associated with acceptance of COVID-19 vaccine among University health sciences students in Northwest Nigeria. PLoS One 16(11): e0260672.
- ECOM-EM (2015) Standard questionnaire on risk perception of an infectious disease outbreak This tool contains example questions for public surveys on risk perception of (an outbreak of) an infectious disease.
- Ejeh FE, Owoicho S, Saleh AS, Madukaji L, Okon KO (2021) Factors associated with preventive behaviors, anxiety among healthcare workers and response preparedness against COVID-19 outbreak: A one health approach. Clin Epidemiol Glob Heal 10: 100671.
- Ejeh FE, Saidu AS, Owoicho S, Maurice NA, Jauro S, et al. (2020) Knowledge, attitude, and practice among healthcare workers towards COVID-19 outbreak in Nigeria. Heliyon 6(11): e05557.
- World Health Organization (2020) World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. Geneva, Switzerland.
- AfrCDC (2020) Africa CDC Guidance for Assessment, Monitoring, and Movement Restrictions of People at Risk for COVID-19 in Africa.
- Linus Oota (2021) COVID-19: Six million Nigerians vaccinated, says NPHCDA.
- Reuben RC, Danladi MMA, Saleh DA, Ejembi PE (2021) Knowledge, Attitudes and Practices Towards COVID-19: An Epidemiological Survey in North-Central Nigeria. J Community Health 46: 457-70.
- Hawlader MDH, Rahman ML, Nazir A, Ara T, Haque MMA, et al. (2022) COVID-19 vaccine acceptance in South Asia: a multi-country study. Int J Infect Dis 114: 1-10.
- Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, et al. (2020) Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front Public Heal 8: 381.
- Sarasty O, Carpio CE, Hudson D, Guerrero-Ochoa PA, Borja I (2020) The demand for a COVID-19 vaccine in Ecuador. Vaccine 38(51): 8090-8098.
- Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. (2020) Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 8(3): 482.
- Xiao X, Wong RM (2020) Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 38: 5131-5138.
- La Vecchia C, Negri E, Alicandro G, Scarpino V (2020) Attitudes towards influenza vaccine and a potential COVID-19 vaccine in Italy and differences across occupational groups, September. Med Lav 111(6): 445-448.
- Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, et al. (2021) COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccines Immunother 17: 1612-1621.
- Tran VD, Pak TV, Gribkova EI, Galkina GA, Loskutova EE, et al. (2021) Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia. Pharm Pract (Granada) 19(1): 2276.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, et al. (2021) Predictors of COVID-19 Vaccine Acceptance, Intention, and Hesitancy: A Scoping Review. Front Public Heal 9: 698111.
- Dong TQ, Rhoda DA, Mercer LD (2020) Impact of state weights on national vaccination coverage estimates from household surveys in Nigeria. Vaccine 38: 5060-5070.
- Huynh G, Nguyen T Van, Nguyen DD, Lam QM, Pham TN, et al. (2021) Knowledge About COVID-19, Beliefs and Vaccination Acceptance Against COVID-19 Among High-Risk People in Ho Chi Minh City, Vietnam. Infect Drug Resist 14: 1773-1780.
- Pauline MCN, Azubuike CMC, Mbachu II, Ndukwu CI, Ezeuko AYA, et al. (2020) COVID-19 infection: Knowledge, attitude, practices, and impact among healthcare workers in a South-Eastern Nigerian state. J Infect Dev Ctries 14(9): 943-952.
- Danielle Paquette (2019) New Nigeria fake news law raises censorship fears - The Washington Post.
- Centre for Law and Democray (2021) UN Special Rapporteur for Freedom of Expression Submission on an Annual Thematic Report on Disinformation Centre for Law and Democracy info@law-democracy.org +1 902 431-3688 www.law-democracy.org Submission to UN Special Rapporteur for Freedom of Expressi.
- Pomeranz JL, Schwid AR (2021) Governmental actions to address COVID-19 misinformation. J Public Health Policy 42: 201-210.
- Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, et al. (2020) Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol 35: 775-779.
- Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, et al. (2021) Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS One 16: e0250495.
- Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, et al. (2021) COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health 46: 270-277.
- Laura Ungar (2021) The Gender Vaccine Gap: More Women Than Men Are Getting Covid Shots | Kaiser Health News.
- Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, et al. (2021) Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines 9: 515.
- Tian S, Hu N, Lou J, Chen K, Kang X, et al. (2020) Characteristics of COVID-19 infection in Beijing. J Infect 80(4): 401-406.
- Alqudeimat Y, Alenezi D, Alhajri B, Alfouzan H, Almokhaizeem Z, et al. (2021) Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract 30: 262-271.
- Thomson A, Robinson K, Vallée-Tourangeau G (2016) The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 34: 1018-1024.
- Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, et al. (2021) Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS One 16(4): e0250495.
- Al-Mohaithef M, Padhi BK (2020) Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey</p>. J Multidiscip Healthc 13: 1657-1663.
- Malik AA, McFadden SM, Elharake J, Omer SB (2020) Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 26: 100495.
- Gan L, Chen Y, Hu P, Wu D, Zhu Y, et al. (2021) Willingness to Receive SARS-CoV-2 Vaccination and Associated Factors among Chinese Adults: A Cross Sectional Survey. Int J Environ Res Public Health 18(4): 1993.
- Kelly BJ, Southwell BG, McCormack LA, Bann CM, MacDonald PDM, et al. (2021) Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect Dis 21(1): 338.
- Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, et al. (2021) Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun 12(1): 29.
- Chew NWS, Cheong C, Kong G, Phua K, Ngiam JN, et al. (2021) An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int J Infect Dis 106: 52-60.
- Dzieciolowska S, Hamel D, Gadio S, Dionne M, Gagnon D, et al. (2021) Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am J Infect Control 49(9): 1152-1157.
- Kwok KO, Li K-K, Wei WI, Tsoi MTF, Tang A, et al. (2022) Likelihood of COVID-19 vaccination among primary school students in Hong Kong. Clin Microbiol Infect 28: 142-144.
- Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, et al. (2021) Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect 108: 168-173.
- Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, et al. (2021) Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill 26(3): 2002047.
- Schrading WA, Trent SA, Paxton JH, Rodriguez RM, Swanson MB, et al. (2021) Vaccination rates and acceptance of SARS-CoV-2 vaccination among U.S. emergency department health care personnel. Acad Emerg Med 28(4): 455-458.
- Nnaji ND, Onyeaka H, Reuben RC, Uwishema O, Olovo CV, et al. (2021) The deuce-ace of Lassa Fever, Ebola virus disease and COVID-19 simultaneous infections and epidemics in West Africa: clinical and public health implications. Trop Med Health 49: 102.
- El-Mohandes A, White TM, Wyka K, Rauh L, Rabin K, et al. (2021) COVID-19 vaccine acceptance among adults in four major US metropolitan areas and nationwide. Sci Reports 11(1): 2184 .
- Shitu K, Wolde M, Handebo S, Kassie A (2021) Acceptance and willingness to pay for COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. Trop Med Health 49: 1-12.
- Mahmud S, Mohsin M, Khan IA, Mian AU, Zaman MA (2021) Knowledge, beliefs, attitudes and perceived risk about COVID-19 vaccine and determinants of COVID-19 vaccine acceptance in Bangladesh. PLoS One 16(9): e0257096.
- Domnich A, Cambiaggi M, Vasco A, Maraniello L, Ansaldi F, et al. (2020) Attitudes and beliefs on influenza vaccination during the covid-19 pandemic: Results from a representative italian survey. Vaccines 8: 1-20.
- Wang J, Jing R, Lai X, Zhang H, Lyu Y, et al. (2020) Acceptance of covid-19 vaccination during the covid-19 pandemic in china. Vaccines 8(3): 482.
- Anjorin AAA, Odetokun IA, Abioye AI, Elnadi H, Umoren MV, et al. (2021) Will Africans take COVID-19 vaccination? PLoS One 16(12): e0260575.
- Wong MCS, Wong ELY, Huang J, Cheung AWL, Law K, et al. (2021) Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 39(7): 1148-1156.






























