Spontaneous Pneumothorax: Diagnosis, Treatment and Recurrence in a Third Level Hospital
Silvia Denise Ponce-Campos1, Felipe de Jesus Contreras-Rodriguez2, Daniel Hernandez-Gordillo3, Eduardo Hernandez-Cuellar4, Luz Audina Mendoza-Topete5, Bertha Nachelly Orozco-Gonzalez3, Fernando Morett-Vera5, Jonathan Alvarez-Pinto5, Aníbal Guerrero-Rodriguez2, Nidia Rodriguez-Plascencia3, Jesus Elvis Cabrera-Luviano6, and Juan Manuel Diaz7*
1Institute of Security and Social Services for State Workers, Pneumology Service, Mexico
2Mexican Institute of Social Security, Pulmonology Department, Mexico
3Mexican Institute of Social Security, Pulmonary Physiology Department, Mexico
4Autonomous University of Aguascalientes, Department of Morphology, Mexico
5Saint Javier Hospital, Mexico
6Institute of Security and Social Services for State Workers, Internal Medicine Department, Mexico
7Autonomous University of Aguascalientes, Medical Didactic Unit, Mexico
Submission: March 01, 2023; Published: March 20, 2023
*Corresponding author: Juan Manuel Diaz, Autonomous University of Aguascalientes, Medical Didactic Unit - Postal Code: 20100, Mexico
How to cite this article: Silvia Denise Ponce-Campos, Felipe de Jesus Contreras-Rodriguez, Daniel Hernandez Gordillo, Eduardo Hernandez-Cuellar, Luz Audina Mendoza-Topete, et al. Spontaneous Pneumothorax: Diagnosis, Treatment and Recurrence in a Third Level Hospital. Int J Pul & Res Sci. 2023; 6(3): 555689. DOI: 10.19080/IJOPRS.2023.06.555689
Abstract
Introduction: Pneumothorax is defined as the presence of air in the pleural cavity. It is classified as spontaneous, traumatic, and iatrogenic. Spontaneous pneumothorax is divided into Primary Spontaneous Pneumothorax (PSP) or Secondary Spontaneous Pneumothorax (SSP) depending on the existence of an underlying respiratory disease. This study investigated the factors that influence the onset and recurrence of PSP and SSP such as physical and demographical characteristics, exposure habits, and clinical signs.
Methods: It was carried out a cross-sectional study with 43 patients diagnosed with spontaneous pneumothorax, in this study were observed and analyzed the clinical data from medical evaluation, thorax radiography, and computed tomography.
Results: From 43 patients, 25 (58%) and 18 (42%) were diagnosed with PSP and SSP, respectively. Spontaneous pneumothorax was most common in men (67.4%), and exposure to tabaco and inorganic dust were main factors associated with this. The age was higher in patients with SSP than in PSP. Interestingly, the pneumothorax occurred mainly in the right lung (69.8%) and during spring (41.9%). Hospitalization and resolution time was similar for patients with PSP and SSP, as well as the recurrence rate. The decision of surgical intervention was higher for patients that had recurred. In case of PSP, recurrence was associated with non-surgical treatment.
Conclusions: We did not find differences in the appearance and recurrence of patients with PSP and SSP in terms of physical and demographical characteristics, or exposure habits. We suggest that surgery must be indicated to avoid recurrence, especially for PSP.
Keywords: Spontaneous pneumothorax; Primary spontaneous pneumothorax; Secondary spontaneous pneumothorax; Recurrence; Imagenological
Abbreviations: SP: Spontaneous Pneumothorax; PSP: Primary Spontaneous Pneumothorax; SSP: Secondary Spontaneous Pneumothorax; IP: Iatrogenic Pneumothorax; TP: Traumatic Pneumothorax; COPD: Chronic Obstructive Pulmonary Disease
Introduction
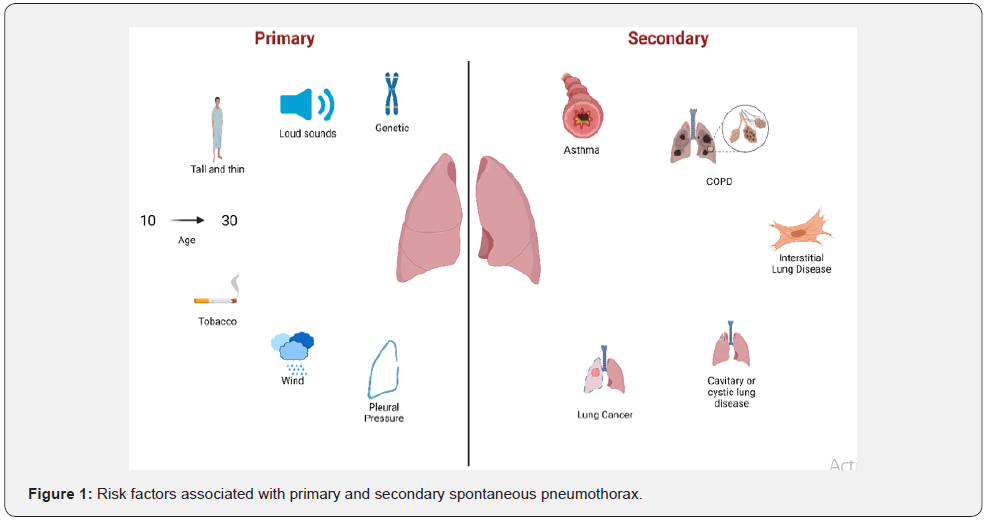
Pneumothorax is clinically defined as the presence of air in the pleural space due to an abnormal communication between the alveolar space and the pleura, or a direct or indirect communication between the atmospheric pressure and the pleural space. It is classified as spontaneous, traumatic, or iatrogenic [1]. The spontaneous pneumothorax (SP) is divided into primary spontaneous pneumothorax (PSP) without an underlying pulmonary disease, and secondary spontaneous pneumothorax (SSP) with an underlying pulmonary disease. The iatrogenic pneumothorax (IP) results from a complication of a medical intervention, and the traumatic pneumothorax (TP) is a perforation from the thoracic wall to the visceral pleura as a result of trauma [2]. The primary spontaneous pneumothorax (PSP) has an incidence of 7.4-18 cases per 100,000 men, and 1.2-6 cases per 100,000 women [3]. This condition occurs typically in tall and slim individuals with an average age of 10-30 years.
Among the risk factors are tobacco smoking, changes in the atmospheric pressure, and exposure to loud music. However, some other factors may include inflammation of the distal airways, genetic predisposition, anatomic alterations, low body mass index, caloric restriction, connective tissue disorders, and ectomorphic somatotype which produces a negative intrapleural pressure [3-6]. The annual incidence of the SSP is 6.3 cases per 100,000 men, 2 cases per 100,000 women, and 26 cases per 100,000 patients with COPD. The highest peak occurs from 60-65 years [1,2]. SSP is characterized by a previous pulmonary condition such as chronic obstructive pulmonary disease (COPD), the most frequent condition (FEV1 <1L and FEV1/FVC ratio <40%) associated with emphysema. Other conditions can be cystic fibrosis, tuberculosis, lung cancer, Pneumocystis carinii pneumonia, lymphangioleiomyomatosis, and histiocytosis X (Figure 1). Another cause is catamenial pneumothorax that occurs in women around 30-40 years with history of endometriosis; it generally affects the right lung and appears during the first 72 h after the onset of the menstrual cycle [7,8].
Clinically, the patients with SP refer a unilateral thoracic pain that disappear spontaneously within 24h. Dyspnea can be presented with minimal to moderate efforts. In some cases, the physical examination can be normal if the size of the pneumothorax is small. On the contrary, in large pneumothorax, thrill and respiratory sounds may be absent, as well as tympanism to the percussion. If this condition progresses, patients may present hypotension, tachypnea, cyanosis, and tachycardia (the most frequent sign). Even though a pneumothorax could be small, it is possible for a patient to present acute respiratory insufficiency as well as severe hypoxemia, hypotension, and hypoventilation [1,2].
Diagnosis for SP can be determined by image methods such as thorax radiography and tomography, in which it is characterized by a displacement of the visceral pleural line from the chest wall. In M-mode sonography, lung sliding is absent with presence of bar code and lung point signs. It is still unclear the causes of appearance and recurrence for SP. Furthermore, most of the studies focused on SP without analyzing separately the patients with PSP or SSP. The aim of this study is to analyze the physical, demographic, and exposure characteristics of patients in the appearance and recurrence of PSP and SSP. Furthermore, the efficacy of conventional management or surgery was analyzed in terms of recurrence for patients with PSP and SSP [1,2,9-11].
Materials and Methods
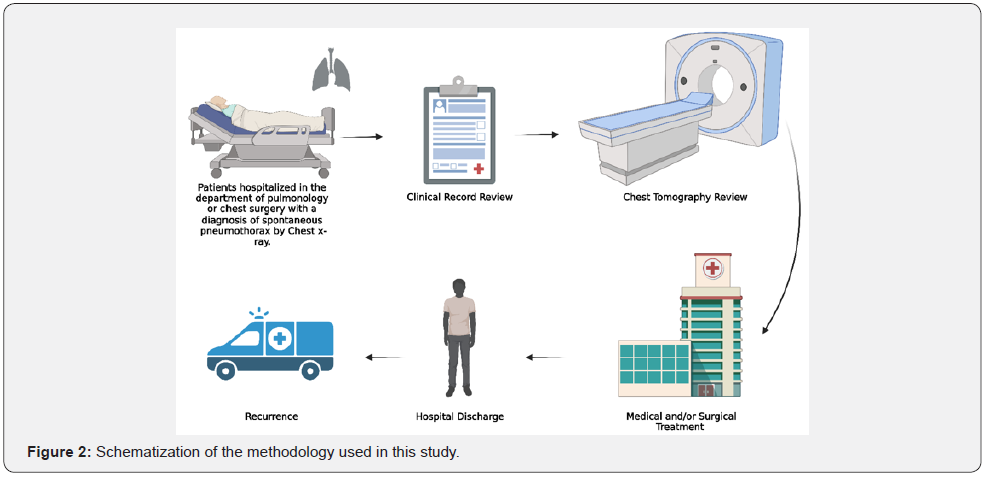
An analytical cross-sectional study was carried out with hospitalized patients diagnosed with spontaneous pneumothorax (SP) during March 2017 to February 2019 at the Department of Pneumology and Thoracic Surgery of the Mexican Institute of Social Security (Mexico, Jalisco). This study was approved by Mexican institute of social security ethics committee (R-2019-1301-030). An informed consent with the information and uses of the data was signed by all the patients enrolled in this study. The inclusion criteria used were as follow: hospitalized patients diagnosed with spontaneous pneumothorax by medical evaluation, thorax radiography and computed tomography, also patients ranged in age from 18 years to 99 years, without gender selection were selected. Otherwise, the exclusion criteria used were patients with iatrogenic or traumatic pneumothorax, pregnancy or lactation, or an ongoing infection during the study.
Patients in this study were grouped into primary spontaneous pneumothorax (disease considered that occurs without an apparent cause and in the absence of significant lung disease) and secondary spontaneous pneumothorax (occurs in the presence of existing lung pathology) in order to observe, analyze, and compare the clinical data obtained from each one [7]. Clinical data obtained from this study were related to sociodemographic and environmental predisposition factors, as well as clinical information derived from medical interview, medical evaluation, and imagenological results in order to analyze and compare this information. Imagenological studies from each patient were used to value the anatomical and pulmonary parenchyma condition, also the radiolucent associated to the presence of air into the thorax (Figure 2). Data obtained in this study were processed and analyzed using GraphPad 8.0 software. Means, frequency, and percentages, as well as standard deviation were obtained and analyzed. Clinic and demographic data were compared using nonparametric unpaired t-test. A statistically significant difference was considered when p<0.05.
Result
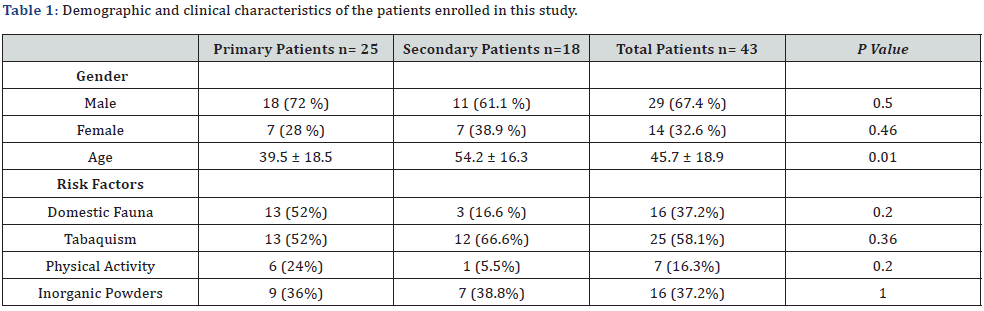
In this study, were diagnosed 43 cases of spontaneous pneumothorax, 25 (58%) of them were identified as PSP and 18 (42%) as SSP. Gender distribution in the PSP group showed the presence of 72% male patients and 28% of female, also the SSP group had a distribution of 61.1% to male and 38.9% for female. Otherwise, age distribution of the patient with PSP showed an average of 39.5 years old (range 18-71) and for SSP 54.2 years old (range 26-72). Some risk factors to which patients are exposed were evaluated, tabaquism was the most frequent factors present in PSP and SSS with a 52% and 66.6% respectively in the groups, also fauna and the exposition to inorganic powder were frequent factors (Table 1). There were no significative differences between the demographic data present in this study.
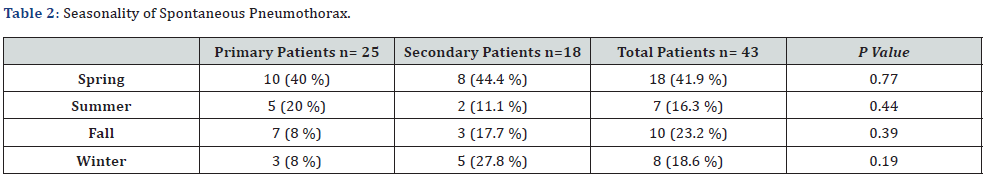
Other consideration evaluated in this study, was the presence of this disease related to the seasonality (Table 2). Most of the patients presented SP in spring (69.8%), followed by 23.2% in autumn, 18.6% in winter, and 16.3% in summer. In terms of casualties, there were 2(8%) for patients with PSP compared with 2(11.1%) for those with SSP, resulting in a non-significant difference. (Table 3) shows clinical characteristics of the patients in this study. Interestingly, from the total of cases, the SP was found mainly in the right lung in a 69.8% of patients and followed by 16.3% in the left lung, only 13.9% cases were bilateral. Open thoracotomy for pneumothorax was performed for patients that do not improve their condition with conservative treatment and those with bronchoalveolar fistula. Regarding the treatment, there was not a significant difference in the number of patients surgically intervened for PSP (24%) and SSP (16.6%).
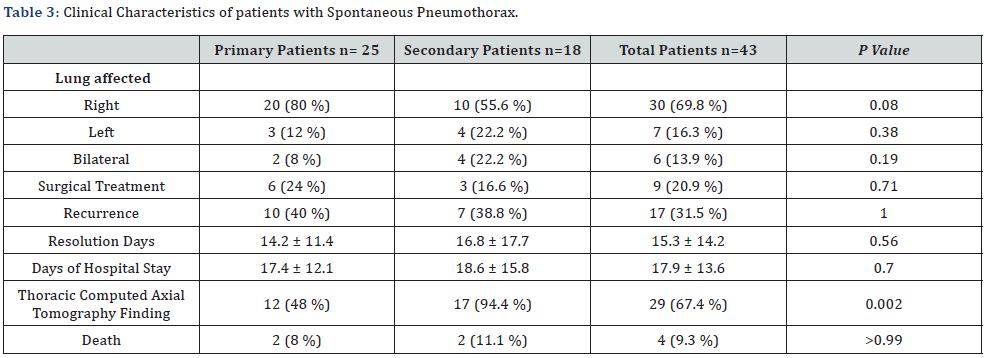
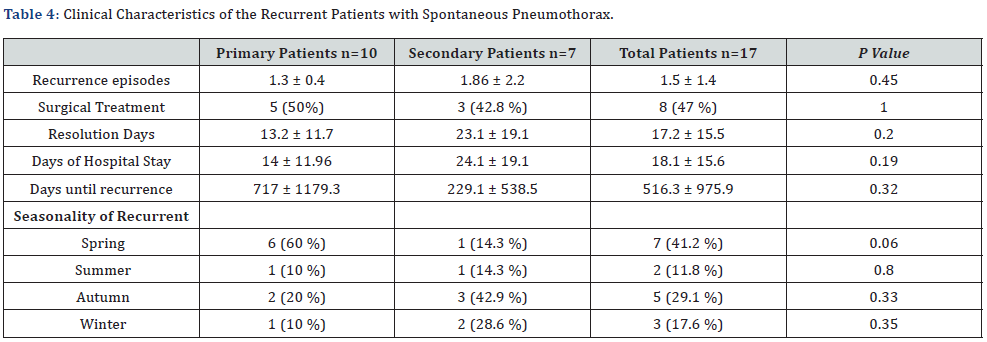
Recurrence of this pathology was observed in 17 patients (39.5%), of whom 10 (59%) from PSP and 7 (41%) from SSP. In both groups, time of hospitalization and recovery were similar and do not show a significative difference. After the analysis of thorax computed tomography, more clinical findings were observed (cysts, bullae, bronchiectasis, cavitations) in patients with PSP compared with those with SSP, 48 % and 94.4 %, respectively. Finally, 9.3% of the patients die along the study derived from this pathology. (Table 4) shows the characteristics of patients with recurrent SP. There was no significant difference between patients with PSP or SSP in terms of number of recurring events, if they were surgically intervened in the first event, resolution time, hospitalization time, and recurrence time. Similarly, regarding the season of the year in which patients had a recurrent episode to SP, it was observed the highest occurrence in spring (41.2%), followed by 29.1% in autumn, 17.6% in winter, and 11.8% in summer; however, for SPS most of patients had a recurrent event in autumn (42.9%) followed by winter (28.6%).
It is worth mentioning that from the 43 patients with SP, 9 (20.9%) were surgically treated, and only 1 showed recurrence; however, from the 34 (79%) that were not surgically treated, 16 showed recurrence. It is worth noting that there was no significant difference in the time of resolution of patients that had recurred to SP (12.18 ± 12.0 days vs 17.38 ± 15.4 days, p= 0.2). Also, there was no difference in the hospital stay (13.71 ± 9.7 days vs 20.6 ± 15.2 days, p=0.1). From the recurrent patients to SP, only (47%) were surgically treated. The time of resolution and hospital stay for patients that had recurred was not different for those treated or not with surgery (23.8 ± 17.29 days vs 11.4 ± 11.7 days, p=0.1; 24.8 ± 17.2 days vs 12.2 ± 11.9 days, p=0.09, respectively). Furthermore, the hospital stay was not significant different for patients with the initial or recurrent SP (13.7 ±9.7 days vs 18.1 ± 15.6 days, p=0.2).
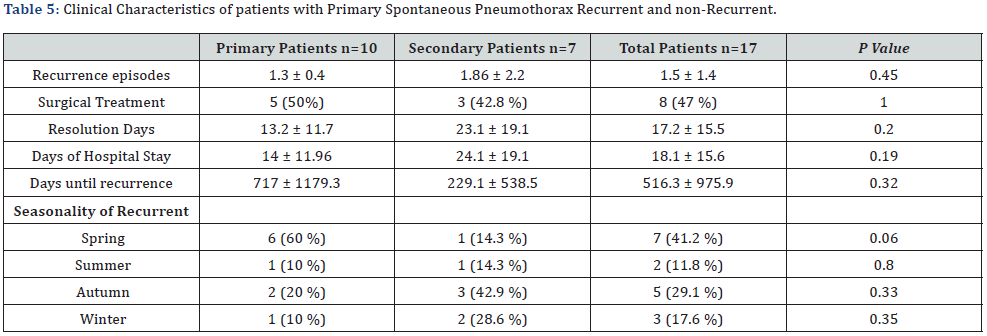
(Table 4) shows the comparative analysis between the recurrent and non-recurrent patients to PSP. Interestingly, from the patients that had recurred, none of them were surgically treated in the initial event, and for those that did not show recurrence, 9 (60%) were surgically treated (p=0.05). It was not found significant difference for the rest of variables. For 10 patients with recurrent PSP, 5 (50%) were surgically treated and 5 (50%) were treated with conservative management. Finally, there was no difference neither in the resolution time (9.3 ± 8.9 vs 13.2 ± 11.7, p=0.1) nor in the hospital stay (12.3 ± 9.3 days vs 14 ± 11.9 days, p=0.1) for patients with PSP comparing the initial and recurrent event. Finally, (Table 5) show the clinical characteristics from primary spontaneous pneumothorax patients with recurrent and non-recurrent.
Discussion
Pneumothorax is a multifactorial disease associated to anatomical alterations (congenital or acquired), exposure to environmental risk factors, as well as acute trauma events, these factors may lead to an alveolar-pleural communication condition and resulting in the presence of air in the pleural space. This respiratory disease has serious implications quality of life and in some cases cause the death of the patient. Worldwide, several research groups had been working into obtain, describe, and develop information relate to evaluate risk factors, optimize the diagnosis methods, and develop efficient treatments for this pathology. Moreover, is essential the obtention of more information from different geographical in order to provide more data for the knowledge of this condition.
In this study, there were not found differences between patients with PSP and SSP in terms of the factors involved in the presentation of the respiratory disease such as demographic, environmental, or anthropometric variables. It was only found a difference in the age at which the condition was initially presented, being younger the patients with PSP compared to those with SSP who often present chronic respiratory diseases. This is in agreement with previous studies reported in the literature [1,12-14]. On the other hand, we found by computer-assisted tomography of the chest, a significant difference in the clinical signs of patients with SSP in comparison with those with PSP. It was as expected as patients with SSP already have a pulmonary disease. Furthermore, it was observed that in most cases the right lung was affected. Different to this finding, it was shown in a previous work similar rates of the pneumothorax in the right and left lungs of patients with SP, PSP, and SSP [12]. Although there are clear anatomical differences in the right and left lung, there are not many studies so far analyzing the laterality of the SP in lungs of patients with this condition.
Similar to previous studies, the recurrence rate was similar for patients with PSP and SSP. Time of resolution and hospital stay in patients with SP was similar for both groups. This could be due to the conservative management provided in our institution for SP independently of being PSP or SSP. Regarding the season at which the SP was presented, it was observed that most of the patients presented SP in spring. There have been some studies analyzing the role of meteorological factors in the onset of SP, such as atmospheric pressure, outdoor temperature, relative humidity, and wind speed. However, the results have been contrasting showing a correlation in some studies while the meteorological factors were dispensable in other studies [15-19]. In case of recurrence, most of patients with PSP showed recurrence in spring followed by autumn while most of patients with SSP showed recurrence in autumn followed by winter. We consider that there is still not clear the influence of the altitude and meteorological conditions in the onset and recurrence of SP [13,20].
It was observed a tendency of having a recurrent event in patients that were not surgically treated. We suggest that surgery must be considered since the initial event, especially for PSP as we found that recurrence was higher for non-surgically treated patients. We did not observe a significant difference related to the time of resolution and hospital stay in patients with SP. In other studies surgery has been associated with a decrease in the time of resolution, hospital stay, and recurrence [8,10,21]. However, in our institution surgery is not the first option but the conventional management. Furthermore, the period between the initial and recurrent event was lower for patients with SSP in comparison with those with PSP. We suggest that this was due to the underlying pulmonary disease in patients with SSP.
Recently, the European Respiratory Society published a Meta-analysis study related to the recurrence of PSP. They showed that recurrence was higher in women, and they suggested that this finding may be due to certain physio pathological conditions including cystic pulmonary diseases, mainly lymphangioleiomyomatosis or catamenial pneumothorax. However, these conditions must be ruled out to classify a patient with PSP [12,13]. Finally, according to the clinical criteria, data available and results, surgical treatment could be prioritized from the first event in primary spontaneous pneumothorax; however, it is a single-center study and in a third-level hospital. We consider that is fundamental to carry out multicentric studies related to the subject, which can study factors associated with recurrence, in order to establish a treatment that prevents recurrences in the majority of patients.
Acknowledgments
We thank the Mexican Institute of Social Security for allowing and encouraging the conduction of research devoted to improving the patient care and quality of medical services. We are grateful with all the medical staff and researchers that participated in the conduction of this research. All the figures presented in this study were created with BioRender.com.
References
- Noppen M (2010) Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev 19(117): 217-219.
- Luh SP (2010) Diagnosis and treatment of primary spontaneous pneumothorax. J Zhejiang Univ Sci B 11(10): 735-744.
- Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A (2002) Manual Aspiration versus Chest Tube Drainage in First Episodes of Primary Spontaneous Pneumothorax. Am J Respir Crit Care Med 165(9): 1240-1244.
- Hatz R, Kaps M, Meimarakis G, Loehe F, Muller C, et al. (2000) Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg 70(1): 253-257.
- Loubani M, Lynch V (2000) Video assisted thoracoscopic bullectomy and acromycin pleurodesis: an effective treatment for spontaneous pneumothorax. Respir Med 94(9): 888-890.
- De Smedt A, Vanderlinden E, Demanet C, De Waele M, Goossens A, et al. (2004) Characterisation of pleural inflammation occurring after primary spontaneous pneumothorax. Eur Respir J 23(6): 896-900.
- Terzi, E, Zarogoulidis, K, Kougioumtzi, I, Dryllis, G, Kioumis, I, et al. (2014) Human immunodeficiency virus infection and pneumothorax. J Thorac Dis 6(Suppl 4): 377-382.
- Aragaki-Nakahodo A (2022) Management of pneumothorax: an update. Curr Opin Pulm Med 28(1): 62-67.
- Bradley M, Williams C, Walshaw M (1991) The value of routine expiratory chest films in the diagnosis of pneumothorax. Arch Emerg Med 8(2): 115-116.
- MacDuff A, Arnold A, Harvey J (2010) Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 65(Suppl 2): ii18-ii31.
- Tsakok M, Hallifax R (2021) Updates in Pleural Imaging. Clin Chest Med 42(4): 577-590.
- Onuki T, Ueda S, Yamaoka M, Sekiya Y, Yamada H, et al. (2017) Primary and Secondary Spontaneous Pneumothorax: Prevalence, Clinical Features, and In-Hospital Mortality. Can Respir J 2017: 6014967.
- Walker S, Bibby A, Halford P, Stadon L, White P, et al. (2018) Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J 52(3): 1800864.
- Hallifax R, Goldacre R, Landray M, Rahman N, Goldacre M (2018) Trends in the Incidence and Recurrence of Inpatient-Treated Spontaneous Pneumothorax, 1968-2016. JAMA 320(14): 1471-1480.
- Zhang G, Gao R, Fu J, Jin X, Zhang Y, et al. (2012) Climatic Conditions and the Onset of Primary Spontaneous Pneumothorax: An Investigation of the Influence of Solar Terms. Med Princ Pract 21(4): 345-349.
- Motono N, Maeda S, Honda R, Tanaka M, Machida Y, et al. (2016) Atmospheric temperature and pressure influence the onset of spontaneous pneumothorax. Clin Respir J 12(2): 557-562.
- Daş M, Alar T, Delice O, Gedik I, Bardakci O, et al. (2020) The effect of meteorological variables on spontaneous pneumothorax in two regions with different altitudes. Int J Biometeorol 65(4): 503-511.
- Ogata H, Matsumoto K, Nakatomi K, Nakashima N, Shoji F, et al. (2018) Seasonal and meteorological impacts on primary spontaneous pneumothorax. J Thorac Dis 10(7): 3957-3964.
- Tuluce K, Sevilgen G (2022) Effect of meteorological factors on first episode and recurrence of primary spontaneous pneumothorax. Rev Assoc Med Bras 68(2): 165-169.
- Sadikot R, Cowen M, Arnold A (1997) Spontaneous pneumothorax in a patient with an azygos lobe. Thorax 52(6): 579-580.
- Thelle A, Gjerdevik M, Grydeland T, Skorge T, Wentzel-Larsen T, et al. (2015) Pneumothorax size measurements on digital chest radiographs: Intra- and inter- rater reliability. Eur J Radiol 84(10): 2038-2043.






























