Correlation of Clinical and Radiological Profile of Sputum Positive Pulmonary Tuberculosis with Radiographic Sequalae After Treatment
Shamrendra Narayan1*, Hemant Kumar2, Dipti Agarwal3, Arvind Kumar4, Neha Singh1, Anurag Pathak4 and Manoj Pandey2
1Department of Radiodiagnosis, Ram Manohar Lohia Institute of Medical sciences, India
2Department of Pulmonary Medicine, Ram Manohar Lohia Institute of Medical sciences, India
3Department of Pediatrics, Ram Manohar Lohia Institute of Medical sciences, India
4Department of Social and Preventive Medicine, Ram Manohar Lohia Institute of Medical sciences, India
Submission: February 19, 2023; Published: March 06, 2023
*Corresponding author: Dr. Shamrendra Narayan, MD, Professor (Jr Grade), Department of Radiodiagnosis, Dr Ram Manohar Lohia Institute of Medical sciences, Lucknow, India
How to cite this article: Shamrendra Narayan*, Hemant Kumar, Dipti Agarwal, Arvind Kumar, Neha Singh, Anurag Pathak and Manoj Pandey. Correlation of Clinical and Radiological Profile of Sputum Positive Pulmonary Tuberculosis with Radiographic Sequalae After Treatment. Int J Pul & Res Sci. 2023; 6(3): 555688. DOI: 10.19080/IJOPRS.2023.06.555688
Abstract
Introduction: Pulmonary tuberculosis (PTB) is the most common type and it constitutes more than 80% of the total cases of tuberculosis with significant morbidity and mortality. About 40 % of treated cases of PTB have residual radiological opacity.
Aim: The present study had been undertaken to correlate the clinical and radiological profile of sputum positive pulmonary tuberculosis with radiographic sequalae after treatment.
Materials and Methods: In this prospective observational study demographic profile, bacterial load, duration of symptoms of sputum smear positive pulmonary tuberculosis cases were recorded. Clinicodemographic parameters, Chest x-ray abnormalities, TIMIKA score and additional scores using area of involvement and cavity status were recorded in a structured template at the beginning and end of treatment. Treatment failures or those lost to follow up were excluded from the residual analysis of the study. The analysis was done using the BlueSky Statistics software (Open version) and R software. The Chi-square test and Fisher exact test to measure of association between attributes. The relationships were examined by regression analysis, after establishing the significance of individual variables using univariate test.
Results: Of 132 subjects 99 were evaluated for residual radiographic lesions. The average duration of symptoms was 6 weeks. Reticulonodular opacity and or consolidation predominantly upper lobes was most common initial presentation that showed complete resolution in more than 90% cases. There was overall significant reduction in area scores. Residual fibrosis was seen in 62 % cases. Multivariate analysis showed high odds ratio for some of the attributes.
Conclusion: High area score, age more than 40, high AFB score, and longer duration of symptoms are more likely to end up with residual radiographic lesion after successful completion of therapy.
Keywords: Chest x-ray, Pulmonary tuberculosis; Residual radiographic lesion; Reticulonodular opacity; Sputum
Abbreviations: TB: Tuberculosis; PTB: Pulmonary Tuberculosis; RCTs: Randomized Controlled Trials; CXR: Chest X-ray; DSTB: Drug-Sensitive Tuberculosis; AFB: Acid-Fast Bacilli
Introduction
Tuberculosis (TB) is a communicable disease that is a major cause of ill health, one of the top 10 causes of death worldwide and the leading cause of death from a single infectious agent (ranking above HIV/AIDS). The TB incidence rate at national level varies from less than 5 to more than 500 new and relapse cases per 100 000 population per year. Globally, 7.1 million people with TB were reported to have been newly diagnosed and notified in 2019 [1]. Pulmonary TB is the most common type and it constitutes more than 80% of the total cases. Mycobacterium tuberculosis spreads via inhalation route. Once in alveoli, bacilli are either ingested by macrophages and eradicated or it multiply to produce local damage and spread to regional lymph node [2]. Chest radiograph is a useful tool when applied as part of a systemic approach in the evaluation of Pulmonary tuberculosis.
The chest x-ray presentation (extent of involvement) at diagnosis of pulmonary tuberculosis patient is varied. The chest X-ray (CXR) findings in drug-sensitive tuberculosis (DSTB) may be categorized broadly into parenchymal disease (consolidation, cavitation, nodular and military patterns); pleural disease (thickening, calcification, effusion); and lymph node disease. These CXR abnormality might heal with complete resolution of pleural/ parenchymal/ mediastinal lesions or with residual fibro-bronchiectatic changes/ cavitation/ calcification for parenchymal lesion; pleural thickening and calcification for pleural disease and residual nodes or calcification for mediastinal and hilar nodes [3]. Thus, in addition to their role in diagnosis, serial radiographs are preferred by many physicians in monitoring treatment response. However, this tool can be misleading for assessing the progress and outcome of treatment because of the wide spectrum of radiographic responses among TB patients under treatment. About 40 % of treated cases have residual radiological opacity [4]. Pulmonary parenchymal lesions show more residual lesions (67%) than pleural (23%) and mediastinal lesions (9%).
Moreover, patients with residual disease have increased chances of getting repeat treatment for tuberculosis if presented even with some non-tubercular respiratory illness in future. The factors that determines the possibility of residual lesions has not been studied. Several methods were devised for predicting the radiological outcome in various TB treatment trials, such as those described by the Madras TB Chemotherapy Centre in 1960, Simon in 1966 and the National TB and Respiratory Disease Association of the USA in 1969 [5-7]. Despite this, no system has been validated in predicting outcome. Further studies are needed to explore factors that make an individual susceptible to residual lesions as compared to another. This might pave way for research/ intervention in future research to prevent it. Disease severity at the onset of treatment might be one such factor. However, this needs standardization for assessment of severity for the purpose.
Randomized controlled trials (RCTs) and observational studies in adults with TB illustrate lack of standardization in the grading of radiological severity, with each of these studies utilizing different non-validated investigator generated systems to grade CXR severity [8-10]. Anna P Ralph et al. [11] devised a simple, validated method for grading CXR severity in adults with smear-positive pulmonary TB (Timika CXR score) that correlates with baseline clinical and microbiological severity and response to treatment, and is suitable for use in clinical trials [11]. This Timika CXR score proposal has been recently studied in south Indian population by Chakraborti et al. [12] and found to be useful [12]. Present study proposes to evaluate the clinical and radiological profile of sputum positive pulmonary tuberculosis (PTB) cases and its association with the residual CXR abnormality in treatment cured patients.
Methods
Setting and design
This prospective observational study was carried out in Department of Radio-diagnosis, Department of Tuberculosis and Respiratory diseases of a tertiary care hospital. The study was approved by institutional review board and institutional ethics committee (20/18).
Sample size
Extensive literature search was done to find out research articles relating X-ray findings at onset of treatment to findings at completion of treatment. All treatment naïve patient’s sputum positive pulmonary tuberculosis during a study period of 12 months, reporting at outpatient department of this institute, fulfilling the criteria and giving consent for study were included in the study.
Study population
Treatment naïve pulmonary tuberculosis sputum smear positive cases registered under Category I of Revised National Tuberculosis Control Program guidelines. Known case of long standing diabetes, chronic obstructive airway disease, Malignancy, Pneumoconiosis, any other chronic respiratory illness, previous history of antitubercular treatment and HIV reactive patients were excluded from the study. Detailed clinical history and investigations were recorded. Density of acid-fast bacilli (AFB) in the sputum was graded as 1, 2 or 3+ (AFB Score) according to standard protocols. Chest x-ray PA view was evaluated at the time of TB diagnosis and at the end of treatment.
X-Ray Evaluation
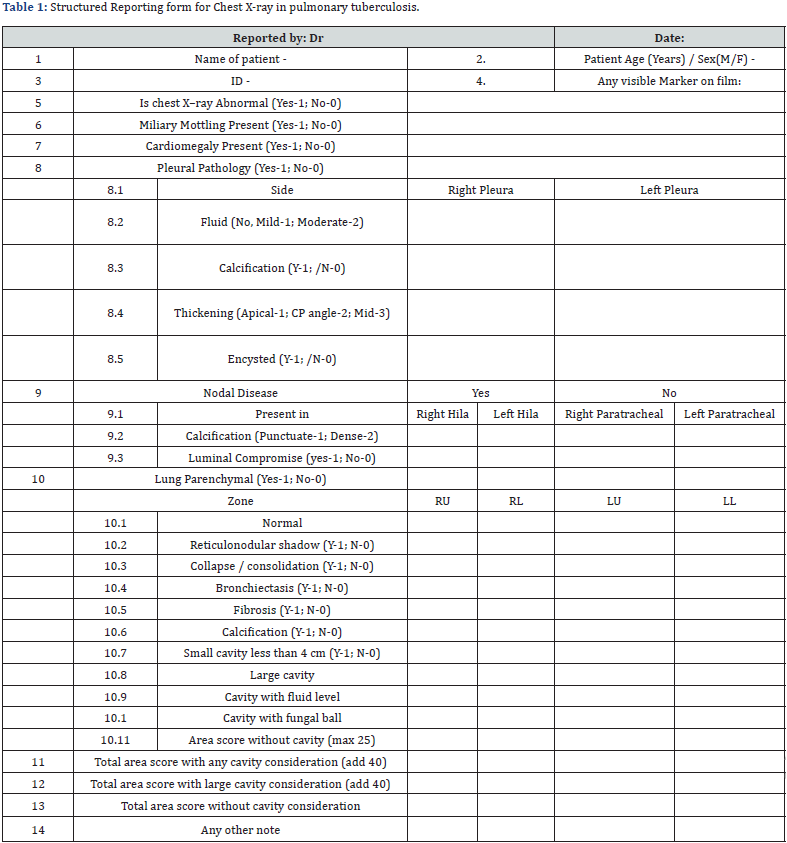
Structured reporting template was prepared (Table 1) using the predefined nomenclature.
Glossary of terms used
a) Lung zones were divided into upper and lower zone by the ipsilateral hilar level. Area percentage shall be stated in comparison to total area of zone by eyeballing: RU/ LU/ RL/LL with a maximum score of 25 for each segment. To calculate percentage of affected lung, visual estimation of the extent of opacification, cavitation or other pathology as a percentage of visible lung was made; dense opacification of a zone was graded as score of 25, while the patchy opacification within a zone attracting scores <25 depending on opacification extent.
b) Cavity: at least 50% of wall is visible and size > 1cm, size will be taken as maximum diameter rounded to nearest 0.5cm. Size less than 4cms in maximum diameter are categorised as small cavity. In case of multiple cavities in one zone cavity then largest cavity should be measured. Cavity: cavity if overlapping in two zones then it should be counted in zone where more than 50% but for measurement of lung area involvement calculation it should be considered on its appearance in each lobe separately.
c) Consolidation: lobar/ segmental uniform homogenous opacity with or without air bronchogram.
d) Bronchiectasis: cysts/ tram line/ honeycomb appearance
e) Miliary: uniform sized <3mm shadow seen in multiple zones
f) Nodules: shadow > 3mm up to 3cm with well-defined margin
g) Reticulonodular infiltrates: Patchy merging nodules/ clusters with some reticular pattern.
h) Volume loss: collapsing anatomical outlines
i) Fibrosis: streaky shadows with some architectural distortion
j) Lymphadenopathy: lobular soft density, focal narrowing of airway is seen to be noted. Both hila should be equal size and density with v point on left at 1 cm above right or at least at the same level. Enlargement should be bumpy/ nodular/lobular, and vessels should not continue.
k) Calcification: extremely dense opacity
l) Pleural effusion: encysted: loss of normal crescent / bulging fluid outline.
m) No effusion; Mild: (<500ml) Horizontal limb of crescent has not reached the level of highest point of dome of diaphragm; Moderate: anything more than mild (>500ml).
Observations were coded numerically (binomial/ ordinal). The format was tested with 20 tester chest radiographs by 5 observers (1st,2nd and 3rd year radiology resident, one senior resident in radiology and one senior resident in pulmonary medicine). The result showed significant for level of agreement for all attributes (0.6-1) and the template was used for recording CXR findings in subjects. Area CXR score (TIMIKA Score) was calculated as proportion of total lung affected (%) + 40 if large cavitation (>= 4cms) present was calculated for each subject [11]. Additional scores without cavity consideration based on area percentage only; as well as score with any cavity consideration where mere presence of cavity irrespective of size were assigned a value of 40 that was added in area score were also calculated. Chest x-ray PA view was evaluated at the time of TB diagnosis and at the end of treatment. X-ray abnormalities were recorded as per schedule by radiologists of experience over 10 years who were blinded to bacteriological and clinical parameters and treatment outcome.
Variables
Following variables were considered as the possible predictors for residual lesions on CXR in our study: Age, Sex, Duration of symptoms before start of treatment, AFB Score, Pleural disease, Nodal disease, Parenchymal disease, area score and cavity status.
Outcome measure
The primary outcome measures at the end of therapy was treatment cured patient with no residual radiographic positivity at the end of therapy. Residual lesions were recorded as parenchymal Fibrosis, calcification, cavitation, pleural thickening, and mediastinal/ hilar residual adenopathy. Cases which were defined as treatment failure as per RNTCP guidelines after intensive phase of therapy, or those lost to follow up were excluded from the study.
Statistical analysis
The X-ray findings were objectivized as numerical scores for individual variates (continuous, ordinal, or binomial scale as applicable). These numerical values were entered into Microsoft Excel sheets and for subsequent analysis using the BlueSky Statistics software (Open version) and R software. All statistics were two-sided with p-values less than 0.05 indicating statistical significance. The quantitative data were recorded as mean ± SD or median with IQR. Shapiro Wilk test is used for normality checking, then we will apply parametric test or non-parametric test, as applicable.
In the parametric test, we will use t-test for testing of mean difference, and the F test for ANOVA, also in the non-parametric test, we will use Wilcoxon rank-sum test, and the Kruskal-Wallis test, as applicable. Qualitative data were recorded in frequencies and proportions. For the analysis, used the Chi-square test and Fisher exact test to measure of association between attributes. The relationships between sputum findings, clinical findings, and radiological scores would be examined by regression analysis, after establishing the significance of individual variables using univariate test.
Results
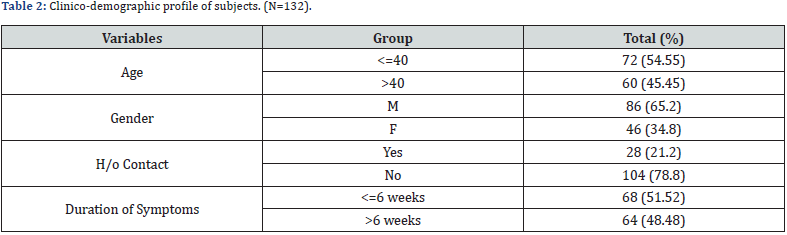
132 subjects qualified the inclusion criteria and recruited in the study of which 99 were evaluated for residual radiographic lesions at the end of completion of therapy as per the criteria laid down. The flow chart of the study population is given in (Figure 1). The clinicodemographic profile of the subjects are summarized in (Table 2). 86 (65% of subject) were male as compared to 46 (35 %) females. Majority of cases did not give history of contact. However, the duration of symptoms before reaching the facility for treatment are evenly distributed around the mean duration of 6 weeks. The radiographic spectrum of sputum positive pulmonary tuberculosis cases has been presented in (Table 3). Majority of cases showed abnormal chest radiograph as compared to only two cases that were normal. There were no miliary cases in our subjects. Only 5 (3.7%) cases presented with nodal involvement.
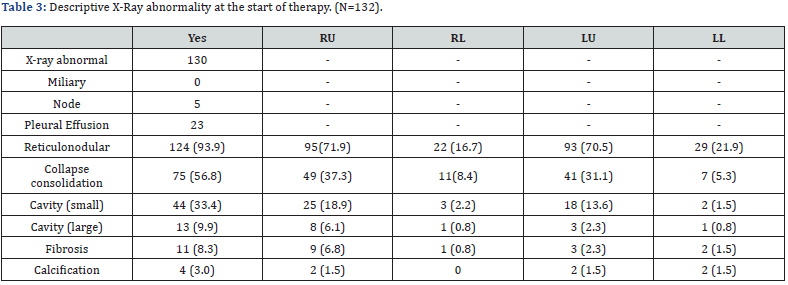
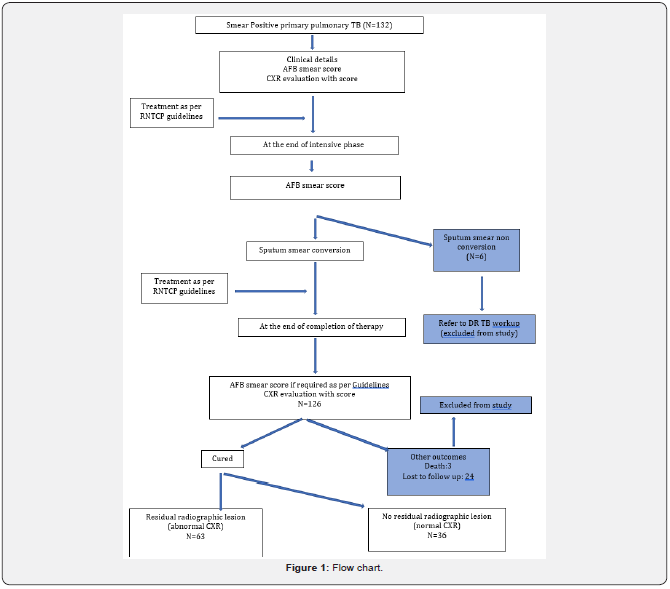
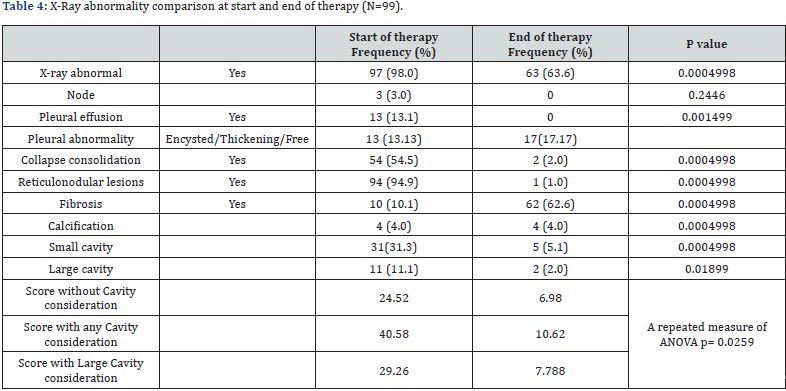
Reticulonodular lesions and consolidation was present in 93.9 % cases with 71.9% cases there was involvement of upper lobes. The details of frequency of abnormality in radiographs of subjects who completed the treatment are given in (Table 4). There was complete resolution of lymphadenopathy and pleural effusion. Reticulonodular lesions and collapse consolidation showed complete resolution in approximately 98 % and 96% cases respectively. However, residual fibrosis was seen in 62 % cases. Of 31 subjects with small cavities on initial radiograph residual cavity was seen in 5 whereas of 11 subjects having large cavities at initial radiograph, residual cavity lesion was seen in 2 cases. There was overall significant reduction in area score measured with different criteria.
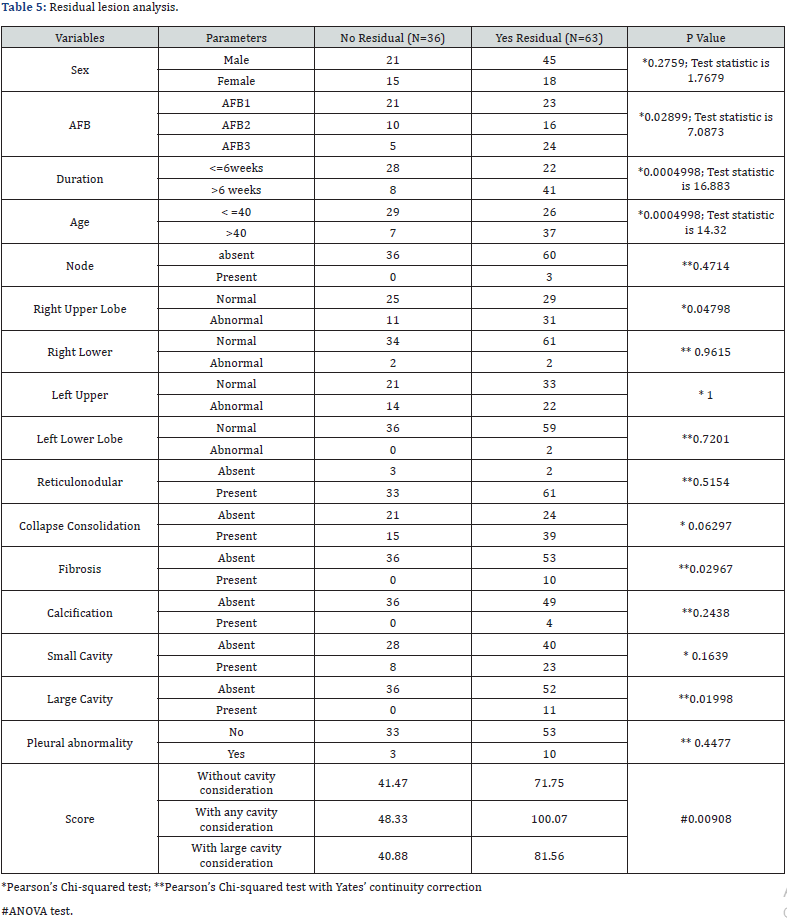
A univariate analysis of all the attributes were done for presence and absence of residual lesion and summarized in (Table 5). Pearson Chi square test with yates’ continuity correction was used for all except the area score. With p value less than 0.05 as significant difference, it was observed that AFB score, duration of illness before start of therapy, age, upper lobar involvement, fibrosis, large cavity, and area score showed significant difference in the population with residual lesion vs no residual lesion. For area score ANOVA test was used as there was no significant difference between residual present and residual absent on the different scores. While testing the mean area score with Tukey multiple comparisons of means it was observed mean area score for cases without residual lesion was 40.9. Also, absolute score with small cavity consideration had the highest mean score at the start of therapy in cases with residual lesions.
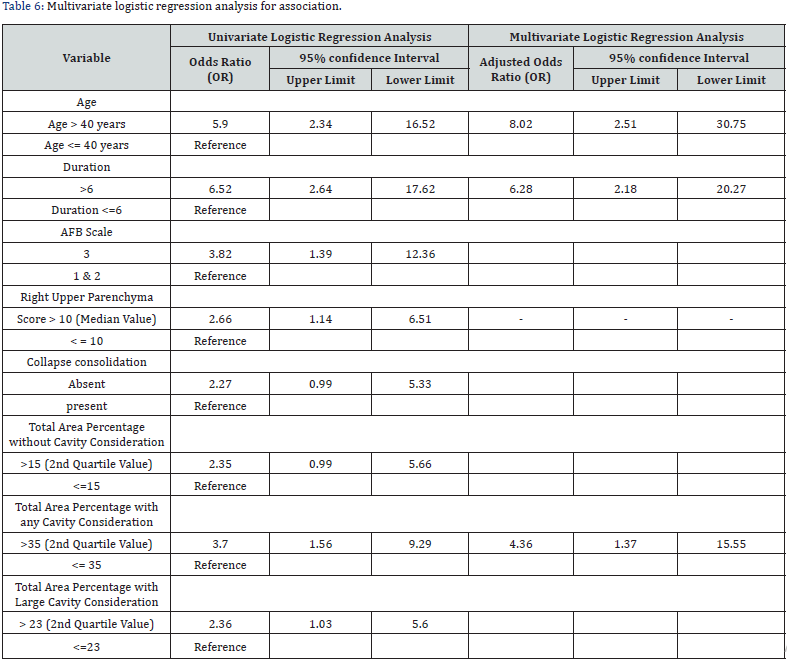
A multivariate regression analysis for association using parameters with significant association with residuals in univariate analysis are shown in (Table 6). Their 95% confidence interval with lower limit and upper limit are also calculated. It was observed that age more than 40, duration of illness more than 6 weeks before start of therapy and area score with any cavity (more than 1cm) consideration more than 35 showed significant association with residual lesion on radiograph after treatment completion with odds ratio of 5.9, 6.5, 3.8 and 3.7 respectively.
Discussion
The study was conducted to analyze the clinical and radiological predictors of residual radiographic lesion in sputum positive pulmonary tuberculosis cases after complete treatment. As the clinical and radiological parameters at presentation are important variables and related data at the presentation has also been analyzed. In era of digital health and AI, both for medical records and communication, reporting template was developed and tested for validity. The participants of the testing tool had different level of acumen and exposure in x-ray reporting. However, well defined nomenclature and objectivity helped in achieving a high level of agreement. Similar observation has been made in other study for picking up abnormality however the agreement was less for some specific changes. This limitation has been overcome with structuring the report template with well accepted definition of the terminology used in our study [13,14]. Thus, this tool can be used for routine reporting at a peripheral health facility with standard medical qualification.
Pulmonary tuberculosis remains a concern for the society in terms of high morbidity and mortality. The analysis of clinic-demographic pattern in the study subject reflect high prevalence in male population could be due to the socioeconomic behavior of outdoor activity leading the higher chances of exposure. Moreover, the education and cultural factors may be a reason where the male/ earning members are more motivated to report to higher centers for better treatment. Significant low history of contact may be due to higher outdoor exposure in public places where people are not aware of the status of other people. However, this is a matter of concern as there may be high prevalence of undiagnosed cases mimicking other respiratory illness.
The analysis of radiographic changes at the presentation shows significant high abnormal radiograph in our study that may be attributed to the inclusion criteria of sputum positivity, making lung parenchymal/ airway involvement more likely. This is consistent with other studies where the sputum positivity shows high incidence of chest x ray abnormality [15-17]. In the two cases that were normal, lesion could be in the hidden areas and that remains the limitation of the modality. There is absence of miliary cases in our group could be attributed to the fact that miliary disease is due to hematogenous spread and a paucibacillary load in the sputum. Though a significant high no of sputum positivity has been reported in miliary cases, this can be attributed to heterogenous group/ observation by chance [18,19].
Incidence of mediastinal adenopathy is maximum in childhood and decreases with age [20]. This may be a reason low prevalence of lymphadenopathy in our observation as majority of patients were adult. Similarly, low prevalence of nodal diseases could be attributed to the fact that primary nodal disease suggests good host immunity and a paucibacillary status. Consistent with the literature that reticulonodular opacity/ consolidation are most common. As well as upper lobar involvement. Lower lobe consolidation was noted in 11% on right side and 7% on left side. Similar observation was made by Shi Chuan Chang where they reported in 5.1% cases [21]. Primary involvement of lower lobes is more common in atypical TB. Presence of calcification in 4 cases may be attributed to previous tubercular infection sequalae.
A very high proportion of patients with sputum positive PTB are left with residual radiographic lesions despite adequate/ complete treatment. Fibrosis was the most common residual lesions seen in almost 99% cases. In a study by Balakrishnan et al. [22] they reported a residual lesion in 40.36% cases unlike ours of 63%, however they had included not only the parenchymal disease but also primary mediastinal and pleural cases. Moreover, on further analysis of residual lesion in sputum positive cases they observed residual in 70 % cases slightly higher than our observation. Fibrosis remains the most common sequalae that present with atelectasis predominantly upper lobe, tractional bronchiectasis, hilar and mediastinal shift [23,24]. Balakrishnan et al. [25] reported occurrence of fibrosis in 57% cases that is much lower than our observation. This difference could be attributed to the fact that in considering other outcome like residual cavity, calcification, bronchiectasis they have not counted fibrosis in them.
Tubercular pleuritis usually resolves however in some cases pleural residual lesion may be seen as thickening, calcification and fibrothorax [25,26]. Known JS et al. [26] reported a residual pleural opacity in 68.3% cases, whereas Balakrishnan et al. [27] reported residual pleural opacity in 23.6% cases [27]. In our study though pleural effusion has resolved in all cases, the cases with pleural abnormality have increased. This paradox can be attributed to the apical pleural thickening in treated cases which was not seen in initial radiograph. Interestingly there is no new case of calcification in the residual analysis at the end of therapy. This can be explained by the fact that calcification is a dystrophic calcification process, and it takes longer time to set up and not dense enough at the end of treatment to show up in radiograph.
In univariate analysis it was observed that AFB score, duration of illness before start of therapy, age, upper lobar involvement, fibrosis, large cavity, and area score showed significant difference in the population with residual lesion vs no residual lesion. However, in multivariate analysis, Age more than 40, duration of illness more than 6 weeks before start of therapy and area score with any cavity (more than 1cm) consideration more than 35 showed significant association with residual lesion on radiograph after treatment completion with odds ratio of 5.9, 6.5, 3.8 and 3.7 respectively. Similar observations have been reported by Al-Hajjaj et al. [28] and teale et al. [29]. Moreover, in a study by Maria et al. [30] there was no difference in radiographic abnormality at presentation between young and elderly, here we have found significant difference in the residual radiographic lesions in young vs old population [30].
Association with higher AFB score may be because high bacterial load means advanced disease and thus greater damage and residual lesions. Similarly, a longer time from onset of symptoms to treatment initiation might contribute to more lung damage and residual lesion [31]. The association of residual radiographic lesion positivity with chest area score is significant especially with small cavity consideration. This can be an independent predictor for residual lesion. Though large cavity has been attributed to presence of residual cavity in radiograph, this was not significantly associated with residual positivity in our study [32]. This association of radiographic severity score with residual lesion has not been studied in literature. Small sample size and significant high no of lost to follow up are major limitations for this study. Significant lost to follow up could be due to covid pandemic leading to difficulty in transportation, limited services at routine outpatient departments, and conversion of hospitals as dedicated level III covid facility leading to migration to nearer health care setup.
Conclusion
There are significant high chances of residual radiographic lesions after successful completion of therapy in PTB cases. Among the radiographic parameters Area score with small cavity consideration more than 35 has 3.7 times more chances of having residual lesion. Other clinical parameters like age more than 40 years and duration of symptom more than 6 weeks before start of therapy has 5.9 and 6.52 times more chances of having residual lesions on radiograph. AFB score 3 usually present with more severe residual radiographic abnormality as compared to lower scores. Early diagnosis and treatment will remain the key factor in preventing residual radiographic abnormalities. Moreover, the so much advancement in research for antifibrotic drugs, use of these drugs in the target population with high probability of residual lesions may be a future area of research in the preventing the residual lesions. Also, the structured reporting tool for chest X-Ray can be used universally for uniform reporting, artificial intelligence, record keeping and thus playing more effective role in end TB strategy.
Acknowledgement
SN shall be guarantor for this study. HK, DA, AK, NS, AP, SN were involved in conceptualization of the study, data collection, analysis, manuscript writing. All authors approved the final version of manuscript.
References
- (2019) Global Tuberculosis Report 2019. World Health Organization.
- Leung AN (1999) Pulmonary tuberculosis: The essentials. Radiology 210(2): 307-322.
- Kim HY, Song KS, Goo JM, Lee JS, Lee KS, et al. (2001) Thoracic sequelae and complications of tuberculosis. Radiographics 21(4): 839-858.
- Menon B, Nima G, Dogra V, Jha S (2015) Evaluation of the radiological sequelae after treatment completion in new cases of pulmonary, pleural, and mediastinal tuberculosis. Lung India 32(3): 241-245.
- Centre TC (1960) A concurrent comparison of isoniazid plus PAS with three regimens of isoniazid alone in the domiciliary treatment of pulmonary tuberculosis in South India. Bull World Health Organ 23(4-5): 535-585.
- Simon G (1966) Radiology in Epidemiological Studies and some Therapeutic Trials. Br Med J 2(5512): 491-494.
- FALK A (1969) Classification of pulmonary tuberculosis. Diagnostic Standards and Classification of Tuberculosis. Pp: 68-76.
- Heo EY, Chun EJ, Lee CH, Kim YW, Han SK, et al. (2009) Radiographic improvement and its predictors in patients with pulmonary tuberculosis. Int J Infect Dis 13(6): e371-e376.
- Thorson A, Long NH, Larsson LO (2007) Chest X-ray findings in relation to gender and symptoms: A study of patients with smear positive tuberculosis in Vietnam. Scand J Infect Dis 39(1): 33-37.
- den Boon S, Bateman ED, Enarson DA, Borgdorff MW, Verver S, et al. (2005) Development and evaluation of a new chest radiograph reading and recording system for epidemiological surveys of tuberculosis and lung disease. Int J Tuberc Lung Dis 9(10): 1088-1096.
- Ralph AP, Ardian M, Wiguna A, Maguire GP, Becker NG, et al. (2010) A simple, valid, numerical score for grading chest x-ray severity in adult smear-positive pulmonary tuberculosis. Thorax 65(10): 863-869.
- Chakraborthy A, Shivananjaiah AJ, Ramaswamy S, Chikkavenkatappa N (2018) Chest X ray score (Timika score): An useful adjunct to predict treatment outcome in tuberculosis. Adv Respir Med 86(5): 205-210.
- Abubakar I, Story A, Lipman M, Bothamley G, van Hest R, et al. (2010) Diagnostic accuracy of digital chest radiography for pulmonary tuberculosis in a UK urban population. Eur Respir J 35(3): 689-692.
- Rastoder E, Shaker SB, Naqibullah M, Wille MMW, Lund M, et al. (2019) Chest x-ray findings in tuberculosis patients identified by passive and active case finding: A retrospective study. J Clin Tuberc Other Mycobact Dis 14: 26-30.
- Agarwal D, Narayan S, Agarwal HK, Singh AK, Pandey M (2022) Pulmonary tuberculosis: An observational study to compare radiographic abnormalities with reference to smear microscopy status. Panacea Journal of Medical Sciences 12(2): 350-354.
- Rai D, Kirti R, Kumar S, Karmakar S, Thakur S (2019) Radiological difference between new sputum-positive and sputum-negative pulmonary tuberculosis. J Family Med Prim Care 8(9): 2810-2813.
- Ebrahimzadeh A, Mohammadifard M, Naseh G (2014) Comparison of chest x-ray findings of smear positive and smear negative patients with pulmonary tuberculosis. Iran J Radiol 11(4): e13575.
- Toure NO, Cisse MF, Dia Kane Y, Diatta A, Bouker BB, et al. (2011) [Miliary tuberculosis: a report of 49 cases]. Rev Mal Respir 28(3): 312-316.
- Gomes M, Saad R, Stirbulov R (2003) Pulmonary tuberculosis: relationship between sputum bacilloscopy and radiological lesions. Rev Inst Med Trop Sao Paulo 45(5): 275-281.
- Geoffrey AA, Richard IM, Sandra SK (1993) Pulmonary tuberculosis in children. Semin Roentgenol 28(2): 158-172.
- Chang SC, Lee PY, Perng RP (1987) Lower Lung Field Tuberculosis. Chest 91(2): 230-232.
- Menon B, Nima G, Dogra V, Jha S (2015) Evaluation of the radiological sequelae after treatment completion in new cases of pulmonary, pleural, and mediastinal tuberculosis. Lung India 32(3): 241-245.
- Jamshed BB, Narainder G, Parveen G, Chandan JD (2003) Imaging of pulmonary tuberculosis. Eur Radiol 13(8): 1771-1785.
- PE Palmer (1979) Pulmonary tuberculosis--usual and unusual radiographic presentations. Semin Roentgenol 14(3): 204-243.
- JA Choi, KT Hong, YW Oh, MH Chung, HY Seol, et al. (2001) CT manifestations of late sequelae in patients with tuberculous pleuritis. AJR Am J Roentgenol 176(2): 441-445.
- Stern EJ (2000) Fraser and Pare’s Diagnosis of Diseases of the Chest, (In: 4th edn), 174(3): 788-788.
- Kwon JS, Cha SI, Jeon KN, Kim YJ, Kim EJ, et al. (2008) Factors Influencing Residual Pleural Opacity in Tuberculous Pleural Effusion. J Korean Med Sci 23(4): 616-620.
- Al-Hajjaj MS, Joharjy IA (2000) Predictors of radiological sequelae of pulmonary tuberculosis. Acta Radiol 41(6): 533-537.
- Teale C, Goldman JM, Pearson SB (1993) The association of age with the presentation and outcome of tuberculosis: a five-year survey. Age Ageing 22(4): 289-293.
- Korzeniewska-Kosela M, Krysl J, Muller N, Black W, Allen E, et al. (1994) Tuberculosis in Young Adults and the Elderly: A Prospective Comparison Study. Chest 106(1): 28-32.
- R Long, B Maycher, A Dhar, J Manfreda, E Hershfield, et al. (1998) Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest 113(4): 933-943.
- Kumar Rai D, Kumar R (2020) Identification of risk factors for radiological sequelae in patients treated for pulmonary tuberculosis: Prospective observational cohort study. Indian J Tuberc 67(4): 534-538.






























