- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
A New Phenomenon: Post-Acute COVID-19 Syndrome
Bharti Sharma*
Consultant Scientist and Epidemiologist, Head of Research Department, Duallinks International, India
Submission: November 10, 2022; Published: November 21, 2022
*Corresponding author: Bharti Sharma, Consultant Scientist and Epidemiologist, Head of Research Department, Duallinks International. 24, I. P. Extension, New Delhi-110092, India, Email: duallinks_3@yahoo.com
How to cite this article: Bharti S. A New Phenomenon: Post-Acute COVID-19 Syndrome. Int J Pul & Res Sci. 2022; 6(2): 555682. DOI: 10.19080/IJOPRS.2022.06.555682
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Abstract
During the last two and half years, the world continues to face public health challenges created by the wave upon wave of COVID-19 (coronavirus disease 2019) infections in the currently ongoing pandemic (being started with the emergence of new, mutated and more transmissible strains of the COVID-19 virus). In the aftermath of the successive waves of the COVID-19 pandemic, many COVID-19 survivors have presented with what has been termed “post-acute COVID-19 syndrome” or “long-term COVID-19.” There is an urgent requirement of both a universal framework for recognizing at risk patients for post-acute COVID-19 syndrome and the provision of multidisciplinary care in targeted COVID-19 outpatient facilities.
Keywords: Post-acute Covid-19 syndrome; Persistent hypoxia; Myocardial fibrosis; Myalgia; Dyspnea
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Introduction
What is post-acute COVID-19 syndrome?
After undergoing wave upon wave of the global pandemic of COVID-19 infection since 2020 till the present year 2022, the healthcare systems of all countries have borne a tremendous level of drain on the available resources. In addition, they have documented an overall scenario of health status crisis in the populations that have suffered from the COVID-19 infection in any form (mild, moderate or severe) [1-3]. Since the numbers of recovering COVID-19 continue to grow with each new wave (brought about by the increasing transmissibility capability of each new variant strain of the COVID-19 virus), there have been an increasing number of published studies that have documented a number of multi-organ sequelae of health issues associated to post-COVID-19 infections [1-6].
It is now an evidence-based fact that the COVID-19 viral infection is one which involves malfunctions of many organ systems of the human body which present in the patients as a wide range of symptoms and lasting health status issues even after the disease has been cured. There has been a high degree of documentation of persisting and long-term effects of the COVID-19 viral disease amongst survivors [2]. This has now allowed the validation of what is loosely known as “post-acute COVID-19 syndrome” or “long-term COVID-19” [1,2,6]. Post-acute COVID-19 syndrome presents with persistent symptoms like continuous fatigue, presence of dyspnea, anosmia, sleep cycle disturbances, poor mental health status as well as a number of observed organ system-specific sequelae [2,3,6-8].
These persistent symptoms are experienced in the long-term period after recovery from the COVID-19 infection bout and have been implicated in the impairment of the patient’s physical status, cognitive functioning. This in turn leads to a poor health status and impaired quality of life as the affected individual is unable to have optimal participation in their work life and society as a whole. Since post-acute COVID-19 syndrome has a serious impact on multiple organ systems of the body, there is urgent need to institute treatment protocols that make use of a multidisciplinary approach in health care provision of COVID-19 survivors that are suffering from this syndrome. There is an urgent requirement of both a universal framework for recognizing at risk patients for post-acute COVID-19 syndrome and provision of multidisciplinary care in targeted COVID-19 outpatient facilities [2,8,9].
At present, the generally accepted norm is that patients suffering from any form of COVID-19 infection show full recovery in 15-21 days (depending on the severity of the infection) provided they have taken correct treatment, but after the two and half years long global COVID-19 pandemic, it is clear that this doesn’t always happen. There has been clear documentation of the long-term as well as serious impacts of the COVID-19 infection (though these are not fully clear at present). The surprising fact is that this long-term sequelae of persistent symptoms have been observed even in individuals who suffered only a mild COVID-19 infection without any need for hospitalization [8,9]. At present, there is no universally accepted definition, but this health issue is being termed as the “post-acute COVID-19 syndrome” or the “long COVID-19.” This review provides a brief descriptive and qualitative summary of the presently researched, studied and health issues of post-acute COVID-19 syndrome which is usually a disease seen in people that recovered from a bout of COVID-19 infection but continue to have health issues [10-18].
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Literature Review Search Methodology and Analysis
Search strategy and selection of relevant research studies
This review research study was done making use of the Preferred Reporting Items for Systematic Reviews (PRISMA) checklist requirements for systematic reviews and meta-analyses [19]. I searched selected databases using the following keywords: Post-acute Covid-19 syndrome, persistent hypoxia, long-term COVID-19, myocardial fibrosis, myalgia, dyspnea, pronounced cognitive impairment, brain fog for studies associated with the long-term impacts of post-acute Covid-19 syndrome (published between 2021 to 2022). For this qualitative as well as descriptive literature review, a number of validated scientific and medical databases were selected and searched for relevant published studies. The searched databases included: Scopus, OVID, PubMed, MEDLINE, Cochrane, ProQuest Central, The Web of Science Index, and Google Scholar.
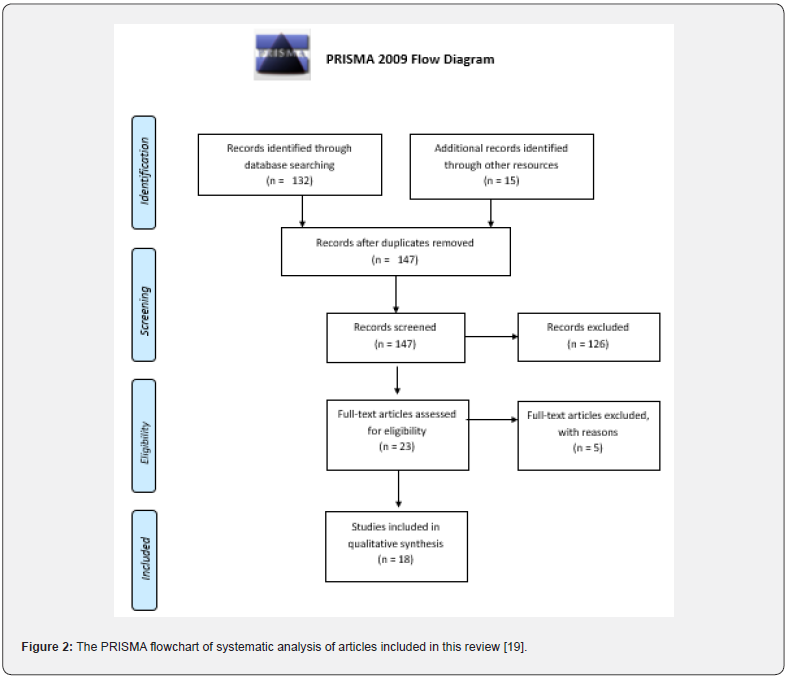
The studies as well as abstracts found in the initial search and investigation were then studied in detail so as to ensure that only relevant studies were short-listed. After this step, the studies were examined in detail so as to identify research studies that had assessed the long-term impacts of post-acute Covid-19 syndrome. In the next step, only the research studies that met inclusion criteria and exclusion criteria for this review were selected while the rest were discarded. Furthermore, any duplicate studies were also removed and the remaining studies were reviewed in detail for the purposes of this study. The final step of data collection was the collating as well summarizing the results, findings and data from all the articles that were included in this review. The included articles were subjected to rigorous qualitative and descriptive analysis so as to identify the long-term impacts of post-acute Covid-19 syndrome with the different kinds of clinical presentations shown by survivors of a Covid-19 infection (Figure 1). (Figure 1) below outlines the multiple-phase iterative methodology utilized for data collection and analysis in this review research study.
Inclusion and exclusion criteria
Since the COVID-19 infection long-term side-effects were studies only since last year, only articles published from 2021 to 2022 were of relevance. Also, articles published a non-English language with no English version available were excluded from this review study.
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Results
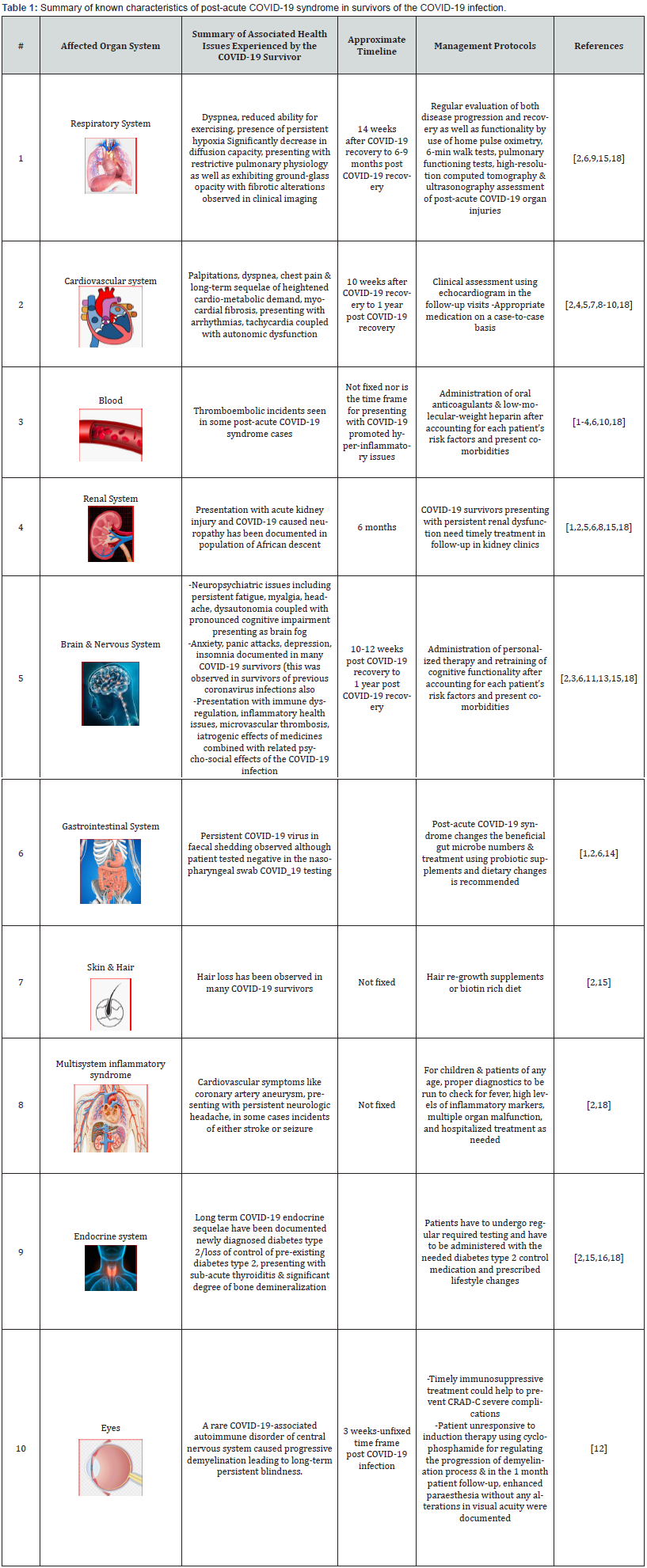
A total of 147 studies were found in the primary search and after removal of duplicates and irrelevant articles, 21 articles were reviewed at the abstract level. Five articles were further excluded for not meeting the inclusion and exclusion criteria (Figure 2). Thus, 18 full-text articles that met the study inclusion were reviewed and contributed to the findings of this systematic review. The 18 studies were characterized and summarized results and finding were summarized (Table 1).
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
After a review of the most comprehensive research studies that have documented the currently known characteristics of post-acute COVID-19 syndrome in survivors of the COVID-19 infection, a brief synopsis of the key issues experienced are present in (Table 1).
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
The presentation of multi-organ sequelae associated with post-acute COVID-19 syndrome in survivors of the COVID-19 infection (in the long-term post recovery from the COVID-19 infection) have started to become an urgent public health issue as more studies continue to present data of sequelae experienced in the time frame needed for presentation of post-acute COVID-19 syndrome or long-term COVID-19 symptoms. This review of published and relevant literature has demonstrated that the chronic symptoms linked to post-acute COVID-19 syndrome have a severe effect on both the patient’s physical as well as cognitive functionality. These in turn causes health-associated detrimental impacts on the patient’s quality of life and prevent them from functioning or participating in all society activities as well as work activities (this causes loss of earnings). There is need for detailed future research that can clearly outline the associations between COVID-19 infection and post-acute COVID-19 syndrome presentations, underlying mechanisms and therapeutic options available.
Moreover, it is clear that care for patients with COVID-19 does not conclude at the time of hospital discharge, and interdisciplinary cooperation is needed for comprehensive care of these patients in the outpatient setting. As such, it is crucial for healthcare systems and hospitals to recognize the need to establish dedicated COVID-19 clinics, where specialists from multiple disciplines are able to provide integrated care. Prioritization of follow-up care may be considered for those at high risk for post-acute COVID-19, including those who had severe illness during acute COVID-19 and/or required care in an ICU, those most susceptible to complications (for example, the elderly, those with multiple organ comorbidities, those post-transplant and those with an active cancer history) and those with the highest burden of persistent symptoms.

It is recommended that in the future, there is an urgent need for ongoing research which would focus on the timely identification as well as characterizing of the main clinical symptoms, serology features and the appropriate use of both imaging and epidemiologic factors of long term COVID-19 (in all stages of the infection including acute, moderate and chronic presentation of this disease) as this will be useful in providing improved understanding of the post-acute COVID-19 syndrome’s pathophysiology and multiple organ involvement in it. In future research studies on the post-acute COVID-19 syndrome, it is necessary to include prospective test groups and also conduct clinical trials, together with regular reviewing of the data collected so as to find key emerging, evidence-based themes by researchers, larger work organizations as well as health care bodies dedicated to the development of a more comprehensive knowledge database which can be used by all the staff involved in clinical practice devoted to COVID-19 recovery and follow up care.
At present, health care staff that provides care for the COVID-19 survivors that present with long term COVID-19 symptoms have to play a very important part in the timely recognition, accurate recording of data, examination as well as appropriate management of presented symptoms. In addition, there is need to provide follow up treatment/management of multiple organ-specific issues that have been observed due to the COVID-19 infection in patients. The health care staff providing post-acute COVID-19 syndrome patients with health care has to simultaneously carry out research studies and clinical studies and also recommend the use of other beneficial recovery resources like existing patient support groups or communities. Given the global scale of this pandemic, it is apparent that the health care needs for patients with sequelae of COVID-19 will continue to increase for the foreseeable future. Rising to this challenge will require harnessing of existing outpatient infrastructure, the development of scalable healthcare models and integration across disciplines for improved mental and physical health of survivors of COVID-19 in the long term.
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
Acknowledgment
I thank Mr. Bharat Sharma for his extended support in data collection and authentication of the validity of the sources during this study.
- Review Article
- Abstract
- Introduction
- Literature Review Search Methodology and Analysis
- Results
- Brief Summary and Main Emerging Themes from The Presently Documented Symptoms of Post-Acute COVID-19 Syndrome
- Future Recommendations for The Management of Post-Acute COVID-19 Syndrome
- Acknowledgment
- References
References
- Montani D, Savale L, Noel N, Meyrignac O, Colle R, et al. (2022) Post-acute COVID-19 syndrome. Eur Resp Rev 31(163): 210185.
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, et al. (2021) Post-acute COVID-19 syndrome. Nat Med 27(4): 601-615.
- Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, et al. (2022) Post‐acute COVID‐19 syndrome (PCS) and health‐related quality of life (HRQoL)—A systematic review and meta‐analysis. J Med Virol 94(1), 253-262.
- Al-Jahdhami I, Al-Naamani K, Al-Mawali A, (2021) The post-acute COVID-19 syndrome (long COVID). Oman Med J 36(1): e220.
- Alkodaymi MS, Omrani OA, Fawzy NA, Abou SB, Almamlouk R, et al. (2022) Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin Microbiol Infect. 28(5): 657-666.
- Tabacof L, Tosto-Mancuso J, Wood J, Cortes M, Kontorovich A, et al. (2022) Post-acute COVID-19 syndrome negatively impacts physical function, cognitive function, health-related quality of life, and participation. Am J Phys Med Rehabil101(1): 48-52.
- Kim Y, Kim SW, Chang HH, Kwon KT, Bae S, et al. (2022) Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis 22(1): 1-12.
- Lledo GM, Sellares J, Brotons C, Sans M, Anton JD, et al. (2022) Post-acute COVID-19 syndrome: a new tsunami requiring a universal case definition. Clin Microbiol Infect 28(3): 315-318.
- Cueto-Robledo G, Porres-Aguilar M, Puebla-Aldama D, MDP Barragan-Martinez, Jurado-Hernandez MY, et al. (2022) Severe pulmonary hypertension: an important sequel after severe post-acute COVID-19 pneumonia. Curr Probl Cardiol 47(3): 101004.
- Korompoki E, Gavriatopoulou M, Fotiou D, Ntanasis‐Stathopoulos I, Dimopoulos MA et al. (2022) Late‐onset hematological complications post COVID‐19: An emerging medical problem for the hematologist. Am J Hematol 97(1): 119-128.
- Nolen LT, Mukerji SS, Mejia NI (2022) Post-acute neurological consequences of COVID-19: an unequal burden. Nat Med 28(1): 20-23.
- Motahharynia A, Naghavi S, Shaygannejad V, Adibi I (2022) Abrupt bilateral blindness as a rare post-acute demyelinating consequence of COVID-19. eNeurologicalSci 28: 100411.
- Rolin S, Chakales A, Verduzco-Gutierrez M (2022) Rehabilitation Strategies for Cognitive and Neuropsychiatric Manifestations of COVID-19. Curr Phys Med Rehabil Rep 10(3): 182-187.
- Ebrahim NR, Shanker A, Sarosiek I, Boschman J, Espino K, et al. (2022) Gastrointestinal symptoms and the severity of COVID‐19: Disorders of gut–brain interaction are an outcome. Neurogastroenterology Motil 34(9): e14368.
- Sanyaolu A, Marinkovic A, Prakash S, Zhao A, Balendra V, et al. (2022) Post-acute Sequelae in COVID-19 Survivors: an Overview. SN Compr Clin Med 4(1): 91.
- Bornstein SR, Cozma D, Kamel M, Hamad M, Mohammad MG, et al. (2022) Long-COVID, metabolic and endocrine disease. Horm Metab Res 54(8): 562-566.
- Algarni AS, Alamri NM, Khayat NZ, Alabdali RA, Alsubhi RS et al. (2022) Clinical practice guidelines in multisystem inflammatory syndrome (MIS-C) related to COVID-19: a critical review and recommendations. World J Pediatr 18(2): 83-90.
- Munipalli B, Seim L, Dawson NL, Knight D, Dabrh AMA (2022) Post-acute sequelae of COVID-19 (PASC): a meta-narrative review of pathophysiology, prevalence, and management. SN Compr Clin Med 4(1): 90.
- Moher D, Shamseer L, Clarke M, Davina G, Alessandro L, et al. (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1): 1.






























