Put A Cap on It: An Unusual Presentation and Protracted Diagnosis of an Inhaled Motorbike Tyre Cap
Ysabelle Embury-Young1*, Georgina Mynott2 and Andrew Low2
1Department of Otolaryngology, Bristol Royal Infirmary, University Hospital Bristol and Weston NHS Trust, United Kingdom
2Department of Respiratory Medicine, Bristol Royal Infirmary, University Hospital Bristol and Weston NHS Trust, United Kingdom
Submission: July 29, 2022; Published: August 17, 2022
*Corresponding author: Ysabelle Embury-Young, Bristol Royal Infirmary, University Hospital Bristol and Weston NHS Trust, Bristol, BS8 2HW. United Kingdom
How to cite this article: Ysabelle E-Y, Georgina M, Andrew L. Put A Cap on It: An Unusual Presentation and Protracted Diagnosis of an Inhaled Motorbike Tyre Cap. Int J Pul & Res Sci. 2022; 6(1): 555679.DOI: 10.19080/IJOPRS.2022.06.555679
Abstract
Foreign body inhalation is rare in the adult population, and where clinical history is uncertain a high index of suspicion is warranted [1]. The typical clinical presentation of foreign body inhalation includes acute shortness of breath; cough; and wheeze. The majority of foreign bodies can be retrieved with flexible bronchoscopy, with rigid bronchoscopy a second-line option [2]. We report a case of a gentleman in his late 50’s referred to respiratory two week wait clinic with a seven month history of a productive cough, breathlessness and intermittent haemopytsis. Computed Tomography (CT) Thorax demonstrated a soft tissue lesion in the right bronchus intermedius with associated right middle and lower lobe collapse, suspected to be a primary lung malignancy. When reviewed in clinic he revealed that his symptoms started after taking his Salbutamol inhaler which he kept uncapped in his trouser pocket. On inhalation he experienced the sensation of something hitting the back of his throat. A flexible bronchoscopy revealed a foreign body in the right bronchus intermedius which was too embedded to be retrieved. He was referred to Thoracic surgery for rigid bronchoscopy who removed a tyre tube cap from the right bronchus intermedius which when shown to the patient he immediately recognised as his motorbike tyre tube cap. This case demonstrates the importance of inhaler technique education including incorporating inspection and re-capping of inhalers [3,4]. We report our case due to its’ unique features: a protracted diagnosis and an unusual presentation.
Keywords: Inhaled foreign body; Respiratory; Thoracic Surgery; General Practice; Bronchoscopy
Abbreviations: GP: General Practitioner; CXR: Chest X-Ray; CT: Computed Tomography; 2WW: Two-Week Wait
Introduction
Foreign body inhalation is rare in the adult population, and where clinical history is uncertain a high index of suspicion is warranted [1]. The typical clinical presentation of foreign body inhalation includes acute shortness of breath; cough; and wheeze. The majority of foreign bodies can be retrieved with flexible bronchoscopy, with rigid bronchoscopy a second-line option [2]. Other cases of differing foreign body inhalation from uncapped inhalers have been described, demonstrating the importance of inhaler technique education including incorporating inspection and re-capping of inhalers [3,4]. We report our case due to its’ unique features: a protracted diagnosis and an unusual presentation.
Case Presentation
A gentleman in his late 50’s first presented to his General Practitioner (GP) in 2021 with a short history of a cough, breathlessness and increased inhaler use. He had a background of Asthma. At the time of his first presentation, he did not have a permanent residential address and had intermittently lived in his car and a shipping container. He was treated for an acute exacerbation of asthma with antibiotics and steroids which led to a temporary improvement in his symptoms. Over the following six months, he consulted with his GP on multiple occasions with symptoms thought to be related to his poor living conditions.
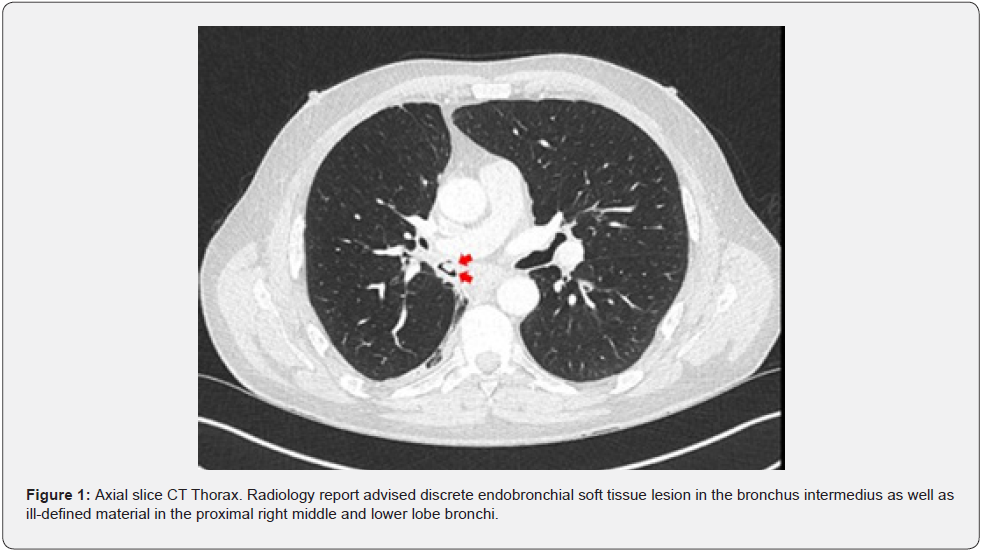
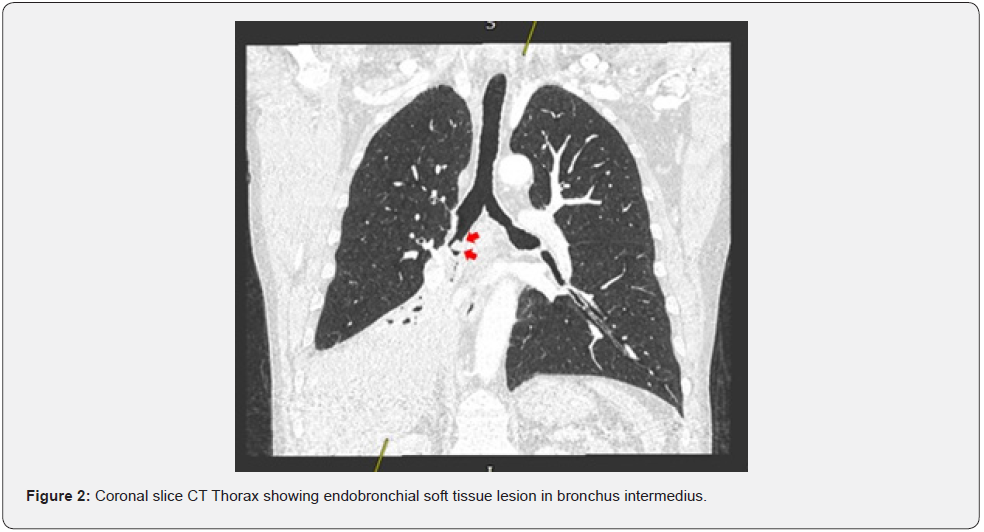
One month later due to persistence of his symptoms a chest x-ray (CXR) was organised by his GP which showed a small right-sided effusion. A repeat CXR performed five months later showed right lower lobe atelectasis and further imaging was advised. A CT Thorax was performed and showed a soft tissue lesion in the right bronchus intermedius with associated right middle and lower lobe collapse and enlarged ipsilateral hilar and mediastinal lymph nodes. Due to these appearances, there was a high suspicion of malignancy, with preliminary staging T4N2M0, and respiratory referral via two-week wait (2WW) clinic was organised.
On review of his CT imaging, it was noted that the soft tissue lesion was intraluminal (Figure 1). Furthermore, the coronal view showed areas of patency around the periphery of the lesion (Figure 2). Due to the intraluminal location of the soft tissue mass, the differential diagnoses considered were an inhaled foreign body or a carcinoid tumour. In respiratory 2WW clinic direct questioning was used to elucidate whether there was any possibility of foreign body inhalation. He recalled cutting down a tree and becoming tight chested, which led him to use his Salbutamol inhaler. On using his inhaler, he instantly felt something hit the back of his throat. This sensation continued throughout the day, however the following morning it had resolved. He then developed his recurrent chest symptoms several weeks later.
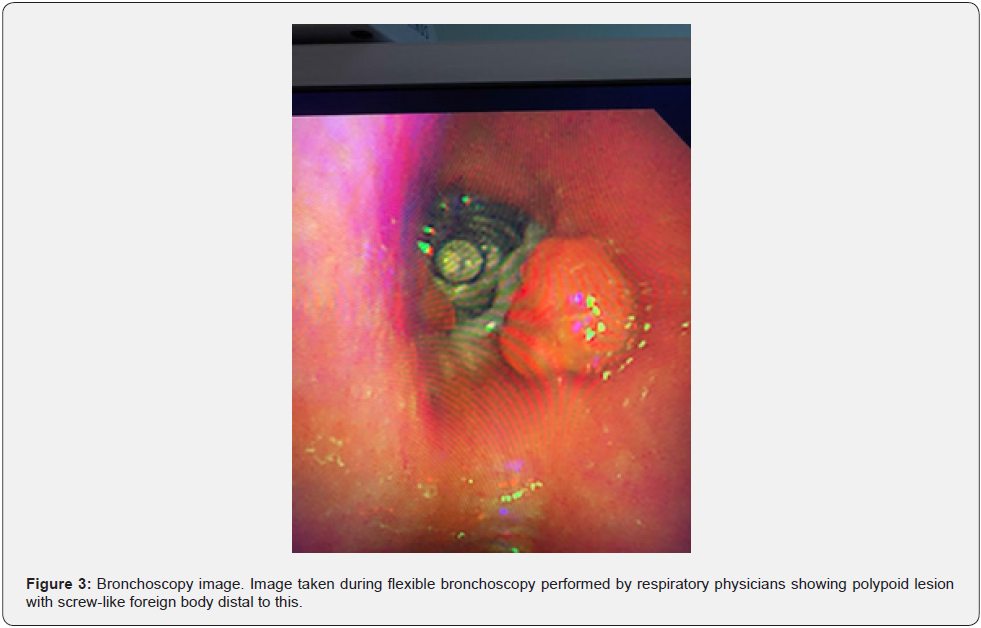
A flexible bronchoscopy was performed which revealed a polypoid lesion in the bronchus intermedius with a screw-like foreign body distal to this (Figure 3). The object was firmly embedded and could not be removed with forceps. The patient was referred to Thoracic surgery for an urgent rigid bronchoscopy which allowed successful removal of a black plastic foreign body. The patient was shown the foreign body following the procedure and instantly recognised it as a motorbike inner tube cap from his Harley Davidson. He reported that he often kept these in his trouser pockets alongside his inhaler. Despite regularly recapping his inhaler he conceded he must not have capped it on that occasion allowing the cap to lodge in the mouthpiece. The endobronchial lesion seen proximal to the foreign body was also removed and the histology was confirmed as benign granulation tissue. Two months after his procedure he reported his exercise tolerance had improved to his pre-morbid baseline and his cough has almost completely resolved. A plan has been made for a 3-month interval CT thorax.
Discussion
Foreign body inhalation is a potentially life-threatening but rare condition in adults. The most common location of inhaled foreign bodies is the right bronchial tree due to its anatomical location and vertical orientation. The majority of inhaled foreign bodies can be retrieved by flexible bronchoscopy in adults, however where this fails rigid bronchoscopy is second-line treatment. Rigid bronchoscopy requires general anaesthesia and has higher associated mortality [1,2]. This case demonstrates a rare but important mechanism of foreign body inhalation. The inspiratory effort required to correctly administer a metered dose inhaler can provide enough force to lodge foreign bodies that have become caught in the inhaler mouthpiece deep into the bronchial tree. Other cases of foreign body inhalation from uncapped inhalers have been described, and these cases demonstrate the importance of good inhaler technique education including incorporating inspection and re-capping of inhalers [3,4].
Asthma UK highlight and summarise patient information for inhaler technique including the importance of checking the mouthpiece prior to use [5]. We believe this case is unique due to the delay in presentation, protracted diagnosis and initial concerns about malignancy, which if pursued may have led to inappropriate investigation and further delay. This patient presented repeatedly with persistent symptoms to primary care and his history of possible aspiration was increasingly overlooked as time passed such that this was not spontaneously volunteered by the patient and was only established following specific questioning. Furthermore, his lack of permanent residential address contributed to a delayed diagnosis due to missed correspondence for radiology appointments, as well as poor living conditions felt to be contributing to his symptoms.
Conclusion
This case demonstrates the importance of inhaler education to ensure dust cap replacement as part of good inhaler technique. This is a rare but important and preventable mechanism of foreign body aspiration. Finally, this case highlights the importance of thorough history-taking to ensure important differential diagnoses are not missed.
References
- Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F (2017) Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis 9(9): 3398-3409.
- Sehgal IS, Dhooria S, Ram B, Navneet S, Ashutosh NA, et al. (2015) Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respiratory Care 60(10): 1438-1448.
- Pelham A (2014) An unusual mechanism of foreign body aspiration: a vignette from the emergency department. BMJ Case Rep 2014: bcr2013202248.
- Blake LK, Silverstone E, Yates D (2015) Treasure in the chest. BMJ Case Rep 2015: bcr2014207398.
- How to use a pMDI inhaler. Asthma UK.






























