Outcome of Tracheostomy for Ventilated Patients during Covid-19 Pandemic - A Single Center Experience
Bernasconi Matteo1*, Bernasconi Gianpiero2, Lanzi Fabio3, Llamas Michael3 and Arigoni Michele4
1Department of General Surgery, Regional Hospital of Locarno (La Carita), Switzerland
2Department of Emergency Medicine, Regional Hospital of Lugano, Switzerland
3Department of Intensive Medicine, Regional Hospital of Locarno (La Carita), Switzerland
4Department of General Surgery, Hospital of Uster, Switzerland
Submission: July 15, 2022; Published: July 27, 2022
*Corresponding author: Bernasconi Matteo MD, Department of General Surgery, Regional Hospital of Locarno (La Carita), Via all’Ospedale 1, 6660 Locarno, Switzerland
How to cite this article: Bernasconi M, Bernasconi G, Lanzi F, Llamas M, Arigoni M. Outcome of Tracheostomy for Ventilated Patients during Covid-19 Pandemic - A Single Center Experience. Int J Pul & Res Sci. 2022; 6(1): 555678. DOI: 10.19080/IJOPRS.2022.06.555678
Abstract
Background: Tracheostomy is a useful tool in the management of mechanically ventilated patients allowing shorter ICU length of stay and sedative consumption. Although its use in COVID-19 patients was initially controversial, we decided to introduce tracheostomy in our strategy of ICU patient management. The aim of our retrospective study is to describe the outcomes of intubated COVID-19 patients comparing patients who underwent tracheostomy to those who did not.
Methods: Data of all intubated COVID-19 patients, treated from 25.02.20 to 06.03.21 in our hospital were collected from our patient registry. Tracheotomy was performed either though a percutaneous dilatational (PDT) or an open surgical technique (OST). Mortality was analyzed and compared between the groups of tracheostomy (A) and non-tracheotomy (B) patients.
Results: A total of 187 intubated COVID-19 patients (mean age 68 years; 71% men) were included in the study. 104 (56%) underwent tracheostomy, PDT being the preferred technique. 30 days mortality of all intubated patients was 54 of 187 (29%). The mortality of tracheotomy patients was significantly lower than non-tracheostomy patients (15% vs 49%; p<.001). Early tracheostomy (< 14 days) led to shorter ICU and hospital length of stay. No surgeon performing tracheostomy developed COVID-19.
Conclusion: Our study is the largest case series of patients comparing intubated COVID-19 patients undergoing tracheostomy to those who did not. Our results show a better mortality rate for tracheostomy patients compared to non-tracheostomy patients. Tracheostomy was therefore not only a safe strategy in management of ventilated bed availability but seems to also affect survival in a positive way.
Keywords: Tracheostomy; Covid-19; Pandemic; Intubation; Ventilated Patients
Abbreviations: ARDS: Acute Respiratory Distress Syndrome; BMI: Body Mass Index; COVID-19: Coronavirus Disease 2019; EOC: Ente Ospedaliero Cantonale; FiO2: Fraction of Inspired Oxygen; ICU: Intensive Care Unit; IMV: Invasive Mechanical Ventilation; NEWS: National Early Warning Score; ODL: Ospedale Regionale di Locarno; OST: Open Surgical Tracheostomy; PaO2: Partial Pressure of Oxygen; PDT: Percutaneous Dilatational Tracheostomy; SARS-COV-2: Severe Acute Respiratory Syndrome Coronavirus 2; SD: Standard Deviation
Introduction
On 11 March 2020, the World Health Organization declared Coronavirus disease 2019 (COVID-19) as a pandemic disease [1]. Between February and May 2020, the first pandemic peak hit the canton of Ticino in southern Switzerland. Because of the border with northern Italy, Europe’s first affected region, our region also witnessed rapid growing numbers of infected patients, hospitalizations and deaths. With a high prevalence of people over-65 years (23%) in a population of about 360’000 inhabitants [2] our canton feared a collapse of the health system. Local government decided to divide acute health facilities in COVID and non-COVID hospitals. Our hospital, Ospedale Regionale di Locarno (ODL) is part of the multi-site public hospital network Ente Ospedaliero Cantonale (EOC). It was designated as one of the two COVID-19 dedicated hospitals in southern Switzerland on 11 March 2020. In normal conditions, ODL has a total capacity of 180 beds. The whole facility was dedicated to COVID-19 patients and non-COVID activities were outsourced to other hospitals of the EOC network.
Our intensive care unit (ICU) capacity was expanded from 8 to 45 ventilator equipped beds. Surgical activity in our hospital was also limited to COVID patients. This organization allowed centralization of material (e.g., mechanical ventilators) and specialized medical and nursing staff. Geographic separation of COVID patients was further thought to help limit the spread of the pandemic and to protect non-COVID patients and health workers. The management of SARS-CoV-2 (severe acute respiratory syndrome induced by Coronavirus disease 2019) patients in need of a mechanical ventilation is consuming many resources. Patients suffering acute respiratory distress syndrome (ARDS) as in our COVID-19 patients have a high mortality and long ICU hospitalization time [3]. Tracheostomy is a useful tool in the general management of intubated ARDS patients. It is known to reduce ICU stay, duration of mechanical ventilation and cumulative sedation dose, thus allowing earlier rehabilitation [4-6].
Positive effect on mortality is however controversial [5]. At the beginning of the COVID pandemic, the use of tracheostomy was not recommended because of the potential risk of infection of health care workers performing this operation [7-9]. We decided however to use this procedure in the management of our intubated COVID patients to face the increasing demand of ICU beds and the shortage of supply of sedatives (Propofol and Midazolam) present during the first pandemic wave. We further created a new intermediate ward with 24 beds able to admit relatively stable tracheostomized patients still in need of ventilatory aid, thus relieving the pressure on the ICU. This strategy was kept in place also during the second pandemic wave from November 2020 to March 2021 even if the number of daily admissions was not as important as during the first wave.
Since the first pandemic wave, several studies have been published on the use of tracheostomy in the management of ICU patients showing safety of the procedure [10-16]. Only a few of these reports presented cohorts with more than 100 patients. To our knowledge only one study compared tracheostomy patients with non-tracheostomy patients and the use and timing of tracheostomy in COVID-patients remains controversial [14]. The aim of our study is to describe our experience in the management of intubated COVID-19 patients between March 2020 and March 2021 comparing outcomes between patients who underwent tracheostomy to those who did not.
Methods
The study was approved by our local ethics committee (2021-00475, Rif. CE TI 3829). All COVID-19 patients admitted to our ICU and subjected to invasive mechanical ventilation (IMV) during the first and second pandemic wave between 25.2.2020 and 06.03.2021 were included in the study. Inclusion criteria were age>18, COVID-19 infection confirmed by nasopharyngeal or oropharyngeal swab and intubation. Exclusion criteria was explicit refusal of study consent. Data including demographic information, co-morbidities, clinical characteristics, e.g., national early warning score (NEWS [17]), ARDS classification (Berlin classification [18]) and tracheostomy procedure details were retrospectively extracted from the digital medical records of our patients. The treating ICU specialist decided about indication and timing for tracheostomy depending on patient’s conditions.
Parameters to guide for patient selection included unfit for extubation, no need for prone positioning for more than 24 hours, positive end-expiratory pressure (PEEP) ≤980 Pa, fraction of inspired oxygen (FiO2) ≤50% and hemodynamic stability without increasing doses of vasoactive drugs. A special surgical team was created for tracheotomies and a standard in-house procedure protocol was defined. Percutaneous dilatational tracheostomy (PDT) using either the Ciaglia or the Twist technique was the preferred surgical procedure. It was performed at patient’s bedside under bronchoscope guidance performed by an anesthesiologist or a pneumologist. Decision to use either the Ciaglia or the Twist technique was based on the availability of tracheostomy material. In case of contraindication to PDT-because of anatomical characteristics (e.g., wide and short neck), open surgical tracheostomy (OST) was performed in a negative-pressure operating theatre. Healthcare providers protected themselves with personal protective equipment following internal guidelines.
No special investigations regarding patient infectivity (e.g., Polymerase chain reaction test) were performed prior to the procedure. For health care workers safety reasons, tracheostomy was performed under general anesthesia to reduce coughing risk and thus aerosolization during the procedure. A cuffed fenestrated tracheostomy tube with flange and a non-fenestrated inner cannula was used. Correct placement of the tracheostomy tube and absence of bleeding was confirmed by bronchoscopy. Pulmonary auscultation, observation of chest movements and end-tidal gas sampling confirmed correct functioning of the tracheostomy. To describe clinical course, time from symptoms onset to hospitalization and time between intubation and tracheostomy were collected. Time from intubation to decannulation was assessed for tracheostomy patients and, in analogy, time of intubation was collected for non-tracheostomy patients.
We defined two study periods corresponding to the first (February and May 2020) and the second (November 2020 and March 2021) pandemic wave. Patients were further divided into 2 groups depending on if they underwent tracheostomy (A) or not (B). As outcome parameters, we analyze 30-day mortality as well as hospital and ICU length of stay for all patients and we compared them between the two patient groups (A and B). All patients were followed up for at least 30 days. Patients of the first pandemic wave had even 60 days follow up. Statistical analysis was performed using student T-test for comparison of mean values. For dichotomous differences, we used the Fisher T-test for small samples and the Chi-square test with Yates correction for samples greater than 5. Kaplan-Meier functions were used to depict survival curves. Statistical significance was defined as P<.05.
Results
Between 25 February 2020 and 6 March 2021, 1572, patients with COVID-19 infection were admitted in our hospital, 242 (15%) patients were transferred to ICU. Of these, 189 (87%) needed intubation and mechanically ventilation. Two patients retrospectively actively refused participation to the study and were withdrawn. Retrospective analysis was therefore performed on 187 patients (80 first wave patients; 107 second wave patients). Tracheostomy was performed in 104 patients (group A: 56%), whereas 83 patients (group B: 44%) were not subjected to this procedure. Mean age of our patient cohort was 68 years (SD 10; range 33-86 years) and the male to female ratio was 133 to 54 (71% vs. 29%). ARDS was classified following the Berlin classification as severe in 126 patients (67%). Mean duration of symptoms prior to hospital admission was 6.3 days (SD 4) and the mean national early warning score (NEWS) at admission was 7.3 (SD 3).
The most frequent comorbidities were arterial hypertension in 104 of 187 patients (56%), obesity in 73 (39%), diabetes in 62 (33%), heart disease in 51 (27%) and chronic obstructive pulmonary disease (COPD) in 31 patients (17%). 66 of 187 patients (35%) were under antiplatelet or anticoagulant therapy (Table 1 & 2). The NEWS score was significant higher in the first pandemic wave compared to the second wave (8 vs 6.7; P=.004). There was no further significant difference for any other of the characteristics neither between first and second pandemic wave patients nor between group A (tracheostomy) and B (no tracheostomy). Of the 104 patients undergoing tracheostomy, 101 patients (96%) underwent bedside PDT. In one patient PDT was not successful and conversion to open technique was necessary. Ciaglia technique was used in 89 of 101 cases (88%) while the Twist technique was performed in 12 patients (12%).
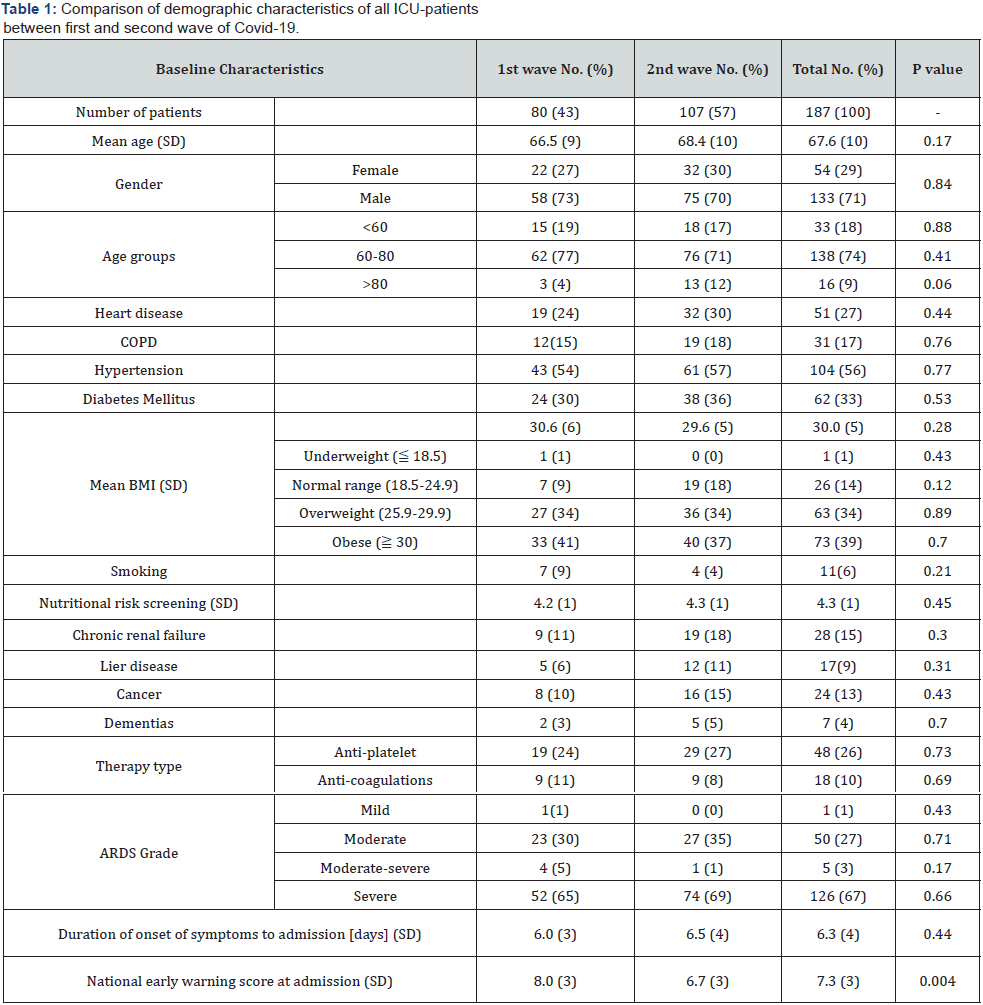
SD: Standard Deviation; ICU: Intensive Care Unit; COPD: Chronic Obstructive Pulmonary Disease; BMI: Body Mass Index; ARDS: Acute Respiratory Distress Syndrome
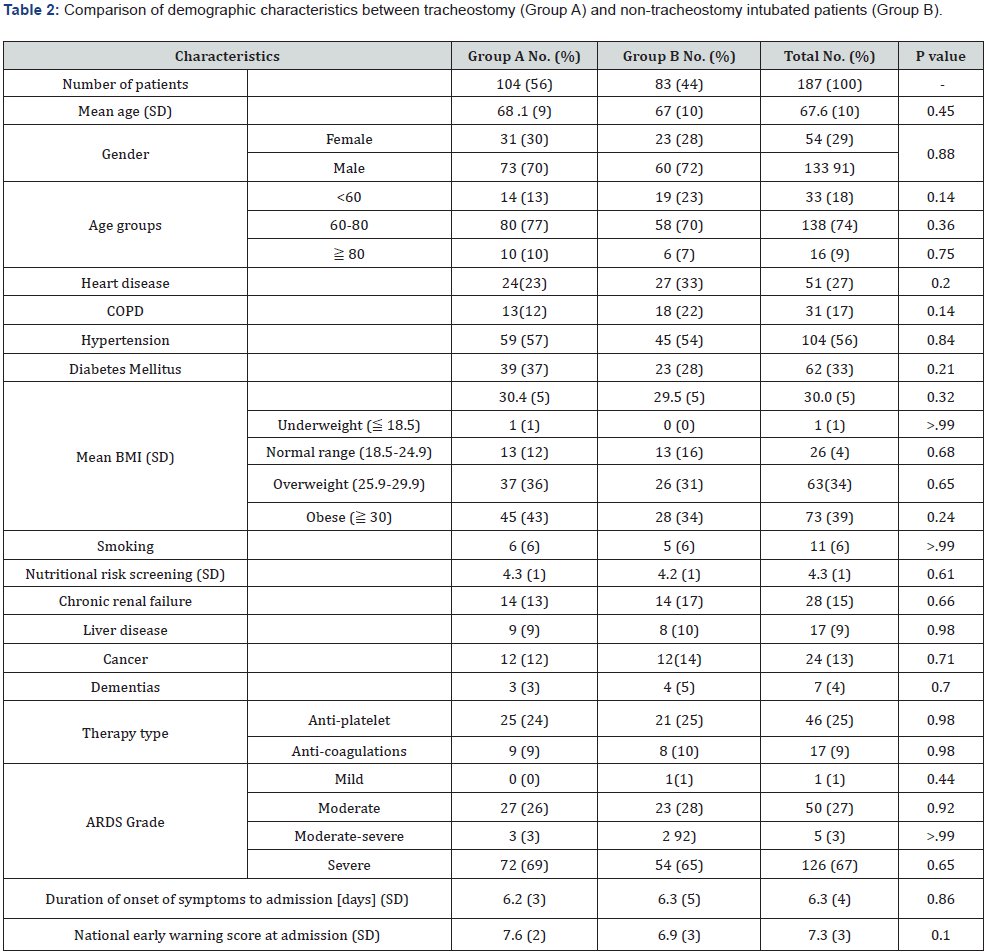
SD: Standard Deviation; COPD: Chronic Obstructive Pulmonary Disease; BMI: Body Mass Index; ARDS: Acute Respiratory Distress Syndrome.
In three obese patients (3%) with very short neck, the risk of PDT failure was considered as high and OST was performed. Our ICU specialists advocated large calibre tracheostomy cannula to facilitate ventilation and diminish the risk of mucus plug formation. According to this, a 10mm cannula was placed in 65 of 104 patients (62%), while in 39 cases (38%) we inserted an 8.5mm cannula. During the first COVID-19 wave we performed 49 (47%) tracheostomy and 55 (53%) during the second wave. Mean time between intubation and tracheostomy was 13.7 (SD 6; range 5-33) days (Table 3). During the first pandemic wave tracheostomy were performed significantly earlier than during the second wave (14.7 vs 12.6 days; P=.06, (Table 3). All patients developed at least one complication (Table 4).
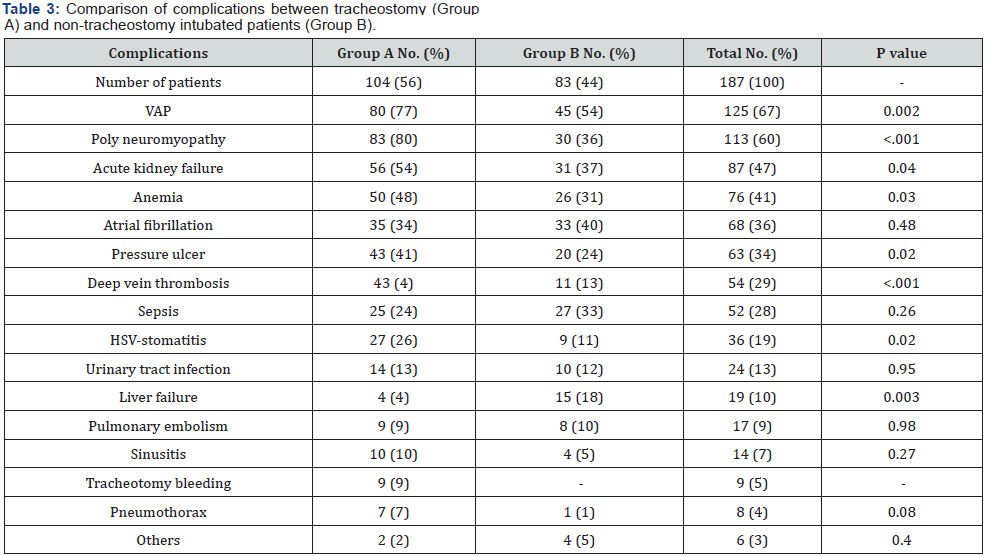
HSV: Herpes Simplex Virus; VAP: Ventilated Associated Pneumonia.
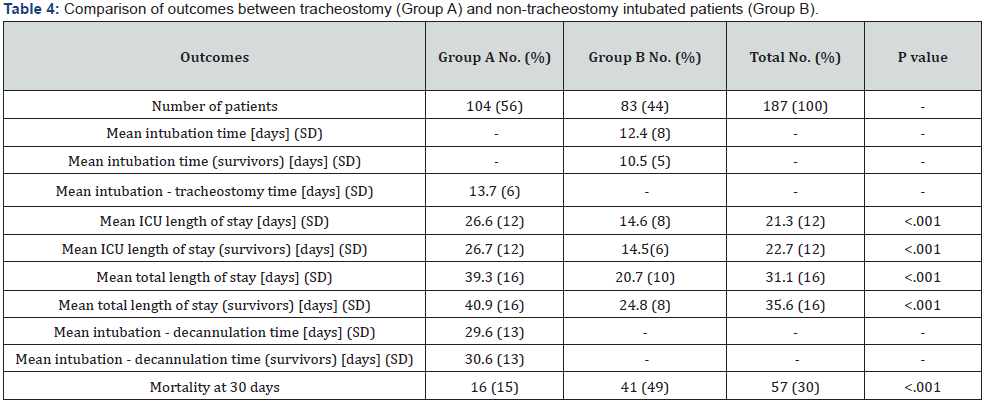
SD: Standard Deviation; ICU: Intermediate Care Unit. No significant difference in 30 days mortality was seen between first and second pandemic wave. Mean timing of tracheostomy after intubation longer during the second wave (14.7 vs 12.6 days, P= .06). Subgroup of no tracheostomy group removing deaths and recovery within two weeks (Subgroup B1, 44 patients) shows higher 30 days mortality than tracheostomy group with 20 deaths (45% vs 15% P<.001).
The most frequent complications were ventilator associated pneumonia (VAP) in 125 of 187 patients (67%), polyneuropathy in 113 (60%), acute kidney failure in 87 (47%), anemia in 76 (41%), atrial fibrillation in 68 (36%), pressure ulcers in 63 (34%), deep vein thrombosis in 54 (29%) and sepsis in 52 patients (28%). Of the 104 tracheostomy patients, nine (9%) developed a local bleeding and in one case surgical hemostasis was necessary. No other procedure related complication were observed. VAP, polyneuropathy, acute kidney failure, anemia, pressure ulcer, DVT, HSV-stomatitis, and liver failure occurred more frequently in the tracheostomy group. No member of the surgical tracheostomy team developed COVID-19 during the study period. Total hospital length of stay was significantly higher in the tracheostomy group (39.3 vs 20.7 days; P<.001). The same applies for ICU length of stay (26.6 vs 14.6 days; P<.001). These differences in length of stay were still significant when considering only survivors.
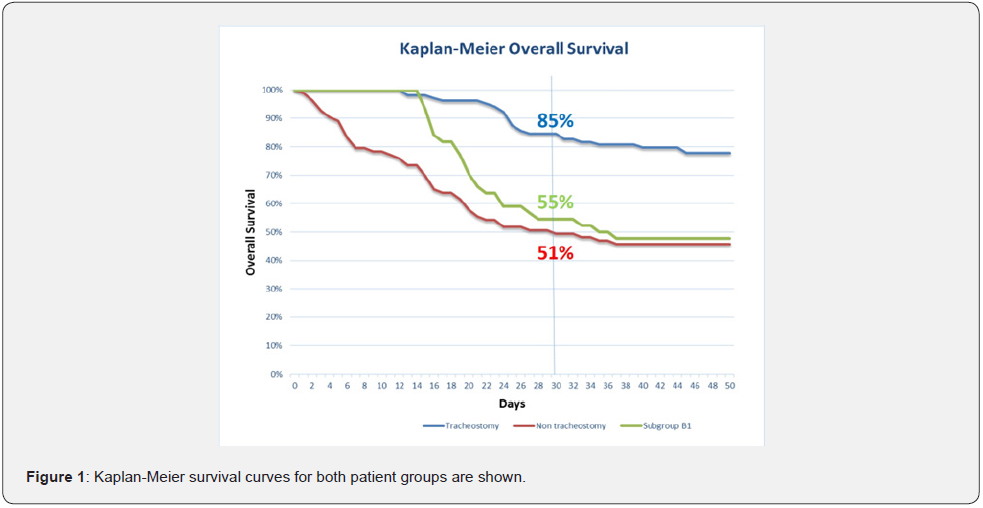
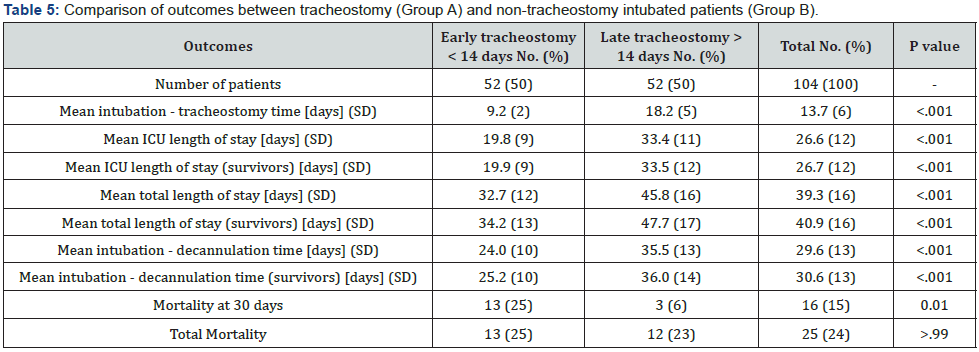
The mean time from intubation to decannulation was 30.6 (SD 13; range 12-76) days for survivors of the tracheostomy group. In total 77 of 104 (74%) patients could be decannulated, two of these patients however died after decannulation. Over 80% of decannulation occurred during hospitalization, the rest in the rehabilitation clinic where patients were transferred. Mean intubation time for group B survivors was 10.5 days (Table 3). To further stratify the tracheostomy group, we separated early (<14 days) and late (≥14 days) tracheostomy patients as shown in (Table 5). Early tracheostomy led to significant shorter hospital and ICU length of stay and to a shorter time from intubation to decannulation. Kaplan-Meier survival curves for both patient groups are shown in (Figure 1). Overall, 30 days mortality for our patient cohort was 57 of 187 patients (30%).
SD: Standard Deviation; ICU: Intermediate Care Unit
Mortality did not change between the first and the second pandemic wave. There was a significant lower mortality in the tracheostomy group at 30 days with 16 deaths of 104 patients (15%) vs 41 deaths of 83 patients (49%, P<.001). In the non-tracheostomy group B, many patients died before reaching the criteria necessary for tracheostomy or recovered rapidly, thus not needing any tracheostomy. Trying to correct this selection bias we removed from group B patients who left the ICU (death or recovery) in the first 14 days after intubation (comparable to the mean time between intubation and tracheostomy). Mortality of the tracheostomy cohort was still lower compared to this new subgroup (B1) of 44 non-tracheostomy patients with 20 deaths (15% vs 45%, P<.001). Mortality of tracheostomy patients was not affected by the timing of tracheostomy (early vs late). At end of follow up 76 of 104 tracheostomy patients were still alive (73%) and 2 patients were lost.
Discussion
Our study is one of the largest single institution studies of COVID-19 patients undergoing tracheostomy extending over a period of 12 months thus covering the first and second pandemic wave that overcame Europe. Overall, 30 days mortality of all intubated patients of 57 of 187 (30%) is lower to the pooled ICU mortality rate of 40% published in the systematic review by Armstrong et al. [19]. In contrast to this review, we did not witness any change in mortality over the course of the study period. In our study intubated patients undergoing tracheostomy (A) showed a lower mortality than those who had no tracheostomy (B). This appeared although no difference in patients characteristics were found between these two cohorts. These findings are in line with the results published in the only other study comparing these two patients groups [14]. Because of the indication criteria for tracheostomy there is however an important selection bias in the non-tracheostomy group, which contains patient fit for early extubation as well as patients too instable for tracheostomy.
This is reflected in the fact that mean intubation time for all patients and for survivors in this group was shorter than the mean time from intubation to tracheostomy in group A (12.4 resp. 10.8 vs 13.7 days). The majority of group A patients either recovered or died very quickly as shown in the Kaplan-Meier survival curves. To try to eliminate this bias we build a subgroup (B1) of non-tracheostomy patients removing patients who died or recovered before 14 days, which corresponds to the mean time of from intubation to tracheostomy. Mortality of group A (tracheostomy patients) remained still lower. Although the effect on survival remains unclear, tracheostomy has shown its benefit in the ARDS management in non-COVID patients shortening ICU length of stay, duration of mechanical ventilation and sedative consumption [4-6]. The use of this procedure is however controversial in COVID-patients. Early study and guidelines suggested avoiding tracheostomy, suggesting the procedure only after careful evaluation and not before 10-21 days [7-9].
Because of the initial very bad course of intubated COVID-19 patients the need for this procedure was questioned. High concerns about contagion of health care workers during the procedure also detracted from this operation. Several studies suggested various tracheostomy techniques to minimize disease spread and some guidelines advocated avoiding percutaneous procedures [20]. Tracheostomy is therefore seldom used in the management of COVID-19 patients (only in 9% of intubated patients) as shown in the study by the COVID-ICU [21]. In our institution tracheostomy was part of the management of ICU patients from the beginning with 104 of 187 (56%) of the mechanically ventilated patients undergoing this operation. Our strategy did not change in time between the first and the second pandemic wave. Meanwhile various studies show the safety and potential advantages of tracheostomy in COVID-19 patients [10-16]. The review by Al Omari et al. [22] shows that open surgical tracheostomy is the most used technique.
We used preferably the percutaneous technique (in 101 of 104 of the cases) at the patient’s bedside. This approach failed only in one patient and an open technique was necessary. A similar conversion rate was reported by Breik et al. [14]. Bleeding of the tracheostomy was the only other procedure related complication with a lower rate (9 of 104 patients, 9% of cases) than reported by other authors [10,13,15] but in line with the studies with most patients [14,16]. Over the whole study period, no surgeon performing tracheostomy contracted COVID-19 confirming the safety of the procedure for health care workers. The mortality rate found in the tracheostomy group is in line with the published data [22], in particular when compared to the largest studies with a similar follow up of more than 30 days [13-14,16]. Unfortunately, even for survivors at 30 days the risk of death remains present [21].
Indeed, the number of survivors decreased from 88 at 30-day to 76 at end of the follow up with two patients lost. Non-procedural complication rate was higher in the tracheostomy group for several complications including VAP, polyneuropathy, acute kidney failure, pressure ulcers and deep vein thrombosis. To our knowledge no other study compared complications in these two patient groups. The higher complication rate could be explained by the fact that tracheostomy patients had a significant longer ICU and hospital length of stay than intubated patients (14.6 vs 26.6 resp. 24.8 vs 40.9 days, P<.001). In the non-tracheostomy group, many patients died or recovered fast, thus having less time to develop complications. Breik et al. [14] found similar higher length of stay in the tracheostomy group. These high values correspond to the ICU and total hospitalization times seen in COVID-19 patients with severe ARDS as in our patient cohort [21].
While in non-COVID-19 patients tracheostomy showed shorter ICU and hospital length of stay this was not the case in our study on COVID patients. Selection bias in the non-tracheostomy group is probably the reason for this. With time the usefulness of tracheostomy in COVID-19 patients has been recognized and guidelines have been adapted [23], but the timing of the procedure is still controversial [24,25]. In our patient cohort survival of tracheostomized patients was not influenced by the time of tracheostomy confirming the results of other authors [10,14]. Other studies however showed a benefit on survival by early tracheostomy [12,15]. Nevertheless, we showed a clear benefit of early tracheostomy for ICU and total hospital length of stay as well as for the time to decannulation confirming findings of other authors [10,12,14-15]. Not being a randomized study and the decision to tracheostomy being dictated by the clinical course of the patient, there is a clear bias in patient selection between the early and the late tracheostomy groups.
Our study presents some limitations. It is a retrospective single center study and there is a selection bias in the non-tracheostomy patient group as presented above. A study randomizing patient now in which they fulfill the criteria allowing tracheostomy would have to be carried out to confirm our findings. The relative low mortality rate compared to the literature in our tracheostomy group shows that our strategy did not harm the patient as for survival.
Conclusion
In our experience, tracheostomy resulted a safe tool in the management of mechanically ventilated COVID-19 patients and was associated with a lower 30-day mortality compared to non-tracheostomy patients. Early procedure led to shorter ICU and total hospital length of stay as well as shorter time to decannulation. It helped manage the ICU resources especially in the first pandemic wave. Further research is warranted to confirm benefits of tracheostomy on survival.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
References
- WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020.
- (2020) Ufficio di statistica del Cantone Ticino, 01 Popolazione: panoramica del tema.
- Bellami G, Laffey JG, Pham T, Fan E, Brochard L, et al. (2016) Epidemiology patterns of care and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315(8): 788-800.
- Siempos I, Ntaidou TK, Filippidis FT, Choi AMK (2015) Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: a systematic review and meta-analysis. Lancet Resp Med 3(2): 150-158.
- Chorath K, Hoang A, Rajasekaran K, Moreira A (2021) Association of early vs late tracheostomy placement with pneumonia and ventilator days in critically ill patients: A meta-analysis. JAMA Otolaryngol Head Neck Surg 147(5): 450-459.
- Wang R, Pan C, Wang X, Xu F, Jiang S, et al. (2019) The impact of tracheotomy timing in critically ill patients undergoing mechanical ventilation: A meta-analysis of randomized controlled clinical trials with trial sequential analysis. Heart Lung 48(1): 46-54.
- Chao TN, Braslow BM, Martin ND, Chalian AA, Atkins J, et al. (2020) Tracheostomy in ventilated patients with COVID-19. Ann Surg 272(1): e30-e32.
- Smith D, Montagne J, Raices M, Dietrich A, Bisso IC, et al. (2020) Tracheostomy in the intensive care unit: Guideline during COVID-19 worldwide pandemic. Am J Otolaryngol 41(5): 102578.
- Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, et al. (2020) Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol 277(8): 2173-2184.
- Botti C, Lusetti F, Peroni S, Tommaso N, Castellucci A, et al. (2021) The role of tracheostomy and timing of weaning and decannulation in patients affected by severe COVID-19. Ear Nose Throat J 100(Suppl-2): 116S-119S.
- Chao T, Harbison S, Braslow B, Hutschinson CT, Rajasekaran K, et al. (2020) Outcomes after tracheostomy in COVID-19 patients. Ann Surg 272: e181-e186.
- Aviles-Jurado FX, Prieto-Alhambra D, Gonzalez-Sanchez N, de Osso J, Arancibia C, et al. (2020) Timing, complication and safety of tracheotomy in critically ill patients with COVID-19. JAMA Orolarygol Head Neck Surg 147(1): 1-8.
- Kwak P, Connors J, Benedickt PA, Timen MR, Wang B, et al. (2021) Early outcomes from early tracheostomy for patients with COVID-19. JAMA Otolaryngolog Head Neck Surg 147(3): 239-244.
- Breik O, Sharna N, Dawson C, Bangash MN, Idle M, et al. (2020) Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study. Br J Anaesth 125(6): 872-879.
- Tang Y, Wu Y, Zhu F, Yang X, Huang C, et al. (2020) Tracheostomy in 80 COVID-19 patients: a multicenter, retrospective, observational study. Front Med 7: 615845.
- Martin-Villares C, Molina-Ramirez CP, Bartolome-Benito M, Bernal-Sprekelsen M, COVID ORL ESP Collaborative Group (2021) Outcome of 1890 tracheostomies for critical COVID-19 patients: a national cohort study in Spain. Eur Arch Otoralyngol 278(5):1605-1612.
- Myrstad M, Ihle-Hansen H, Tveita AA, Andersen EL, Nygard S, et al. (2020) National Early Warning Score 2 (NEWS2) on admission predicts severe disease and in-hospital mortality from Covid-19 - a prospective cohort study. Scand J Trauma Resusc Emerg Med 28(1): 66.
- Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, et al. (2012) The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 38(10): 1573-1582.
- Armstrong RA, Kane AD, Cook TM (2020) Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies. Anaesthesia 75(10): 1340-1349.
- Foster P, Cheung T, Craft P, Baran K, Kryskow M, et al. (2020) Novel Approach to reduce transmission of COVID-19 during tracheostomy. J Am Coll Surg 230(6): 1102-1104.
- COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Inverstigators (2021) Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med 47(1): 60-73.
- Al Omari A, Al-Ashqar R, Alabd Alrham R, Nuseir A, Allan H, et al. (2021) Assessment of the harms and potential benefits of tracheostomy in COVID-19 patients: narrative review of outcomes and recommendations. Am J Otolaryngol 42(4): 102972.
- McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, et al. (2020) Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Resp Med 8(7): 717-725.
- Brenner MJ, Feller-Kopman D, De Cardenas J (2021) Point: tracheostomy in patients with COVID-19. Should we do it before 14 days? Yes. Chest 159(5): 1723-1727.
- Pandian V, Septimiu M, Lamb C (2021) Counterpoint: tracheostomy in patients with COVID-19. Should we do it before 14 days? No. Chest 159(5): 1727-1729.






























