Complication and Sequelae of Pulmonary Tuberculosis: A Tertiary Care Center Experience
Vinod Pal, Kanmani MK, Ketaki Utpat, Unnati Desai* and JM Joshi
Department of Pulmonary Medicine, TN Medical College and BYL Nair Hospital, India
Submission: April 01, 2022;; Published: April 27, 2022
*Corresponding author: Dr. Unnati Desai, Associate Professor and Incharge, Department of Pulmonary Medicine, TN Medical College and BYL Nair Hospital, India
How to cite this article: Vinod P, Kanmani MK, Ketaki U, Unnati D, JM Joshi. Complication and Sequelae of Pulmonary Tuberculosis: A Tertiary Care Center Experience. Int J Pul & Res Sci. 2022; 5(5): 555674. DOI: 10.19080/IJOPRS.2022.05.555674
Abstract
Background: Tuberculosis (TB) is a grave infectious disease caused by the bacillus Mycobacterium tuberculosis (MTB). Pulmonary tuberculosis remains an important public health problem globally and one of most common infectious disease. Tuberculosis can cause wide variety of complication respiratory or non-respiratory. We studied complication and sequelae of pulmonary tuberculosis.
Methodology: A prospective observational study was conducted, the study included all patients presenting with complications of tuberculosis in newly diagnosed and previously treated patients referred to the Pulmonary Medicine Department. Patients not willing to give consent for the study or the patient with incomplete data were excluded. TB was diagnosed on the basis of sputum Gene Expert, Line Probe Assay and Conventional Drug Sensitivity testing.
Results: Of the total 310 cases, 176(57%) patients were males and 134(43%) were female patients. The mean age of all patients was 41.72 years. Among the 310 cases 293(95%) were drug sensitive tuberculosis and 17(5%) patients were of drug resistant tuberculosis. Out of the 310 patients; 160(51%) patients had post TB COPD as complication of TB. Most common complication was post TB COPD while least common was BPF seen in 8(2.5%) patients. The most common co-morbidity was DM which was seen in 15 (5%) patients. Cough was most common among various symptom with which patient presented to hospital. Out of 310 patient who had complication due to tuberculosis 301(97%) patient were hospitalised and 9(3%) patients were treated on OPD basis. Most common complication which leads to hospitalisation was post TB COPD with or without respiratory failure.
Conclusion: Complications are part of spectrum of tuberculosis, however early diagnosis and management will help in salvaging of precious life.
Keywords: Pulmonary tuberculosis; Hemoptysis; Respiratory failure; Post TB; COPD
Abbreviations: TB: Tuberculosis; MTB: Mycobacterium Tuberculosis; ATT: Anti-Tuberculosis Therapy; SCC: Short Course Chemotherapy; DOTS: Directly Observed Treatment Short Course; RNTCP: Revised National TB Control Programme; WHO: World Health Organization; the USAID: United States Agency for International Development; COPD: Chronic Obstructive Pulmonary Disease; PTE: Pulmonary Thromboembolism
Introduction
Tuberculosis (TB) is a grave infectious disease caused by the bacillus Mycobacterium tuberculosis (MTB), which most commonly affects the lungs known as pulmonary TB but can affect other sites as well (extra pulmonary TB). The disease is spread by droplet infection generated when people suffering with pulmonary TB cough or sneeze. Overall, a relatively small proportion (5-15%) of the estimated 2-3 billion people infected with M. tuberculosis develop TB disease during their lifetime. The most effective anti-tuberculosis therapy (ATT) is the short course chemotherapy (SCC) consisting of first-line anti-TB drugs i.e., intensive phase of isoniazid, rifampicin, ethambutol, pyrazinamide followed by continuation phase of rifampicin, isoniazid and ethambutol. The ATT is administered as Directly Observed Treatment Short course (DOTS) program, implemented by the Revised National TB Control Programme (RNTCP) in our country [1].
Complication of tuberculosis significantly contributes to mortality and morbidity of patients. Delay in presentation and poor compliance to treatment give rise to complication in any part of the body. Common complications are haemoptysis, pleural effusion, aspergilloma, post tubercular bronchiectasis, post tubercular COPD, Spontaneous pneumothorax. Rare complications are tuberculous laryngitis, pulmonary artery hypertension and chronic corpulmonale, tuberculous endo bronchitis, tracheitis, ATT induced hepatitis, tuberculosis associated acute respiratory failure, paradoxical reaction and tuberculous vasculitis. Despite the efficacious therapy available in current era for tuberculosis, complication occur due to the anatomical and vascular destruction at the diseased areas leading to nidus of infection and structural compromise [2].
Materials and Methods
A prospective observational study was conducted at the pulmonary medicine department of TNMC & BYL Nair Hospital with IEC permission with ECARP/2018/129. 310 patients were enrolled in the study. The study included all patients presenting with complications of tuberculosis in newly diagnosed and previously treated patients referred to the Pulmonary Medicine Department. Patients not willing to give consent for the study or the patient with incomplete data were excluded. TB was diagnosed on the basis of sputum Gene Expert, Line Probe Assay and Conventional Drug Sensitivity testing. It is a prospective observational study, so data was collected from the patient presenting with complication of pulmonary tuberculosis due to active or past treated pulmonary tuberculosis. In cases with past history of PTB, the details were collected from available records and history. Details of these patients with complications were reviewed and noted for demographic data, history, sputum examinations, co-morbidities and severity of complications. These patients were treated with anti TB therapy under RNTCP (revised national tuberculosis control programme). The treatment outcomes of these patients were noted. Patients with incomplete records were excluded. Demographic data in form of age, sex, past history of pulmonary TB, details of TB therapy, sputum examination details, complications of tuberculosis in the form of nature of complication, time of occurrence, management and outcome of complications were noted (Table 1).

Result
Of the total 310 cases, 176(57%) patients were males and 134(43%) were female patients. Overall youngest patient was of age 11 years and the oldest was of age 82 years. Most of the patients were of age group 21-40 and 41-60 years with 114(37%) patient each and second most common age group was 61-80 years with 46(15%) patients (Table 2). The mean age of all patients was 41.72 years. 35(11%) patients were between 10 to 20 years of age. Among the 310 cases 293(95%) were drug sensitive tuberculosis and 17(5%) patients were of drug resistant tuberculosis (Table 3). 160(51%) patients had post TB COPD as complication of TB. Out of 160 patients all had respiratory failure, among them 69(43%) had type 1 respiratory failure and 91(57%) had type 2 respiratory failure; 58(18.7%) patients had haemoptysis; 30(9.6%) patients had ATT induced hepatitis and same number of patients had empyema (Table 4&5).
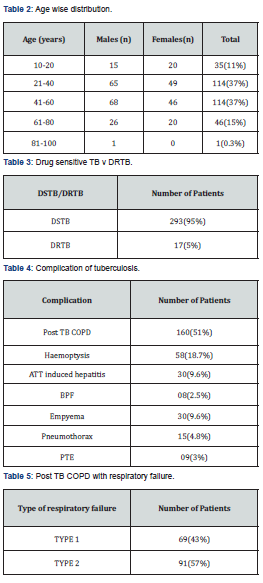
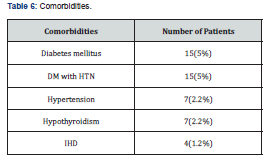
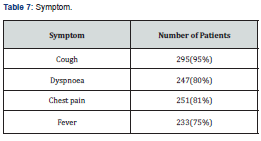
Pneumothorax was seen in 15(4.8%), pulmonary thromboembolism was seen in 9(3%) patients. Most common complication was post TB COPD while least common was Broncho-pleural fistula seen in 8(2.5%) patients. While the various associated comorbidities observed were seen in around 48 patients who were on ATT or had ATT intake. The most common co-morbidity was DM which was seen in 15(5%) patients. Hypothyroidism was noted in 7(2.2%) patients, while IHD was seen in 4(1.2%) patients and Diabetes mellitus with HTN in 15(5%) patients. HTN alone was seen in 7(2.2%) patients (Table 6). Cough was most common among various symptom with which patient presented to hospital. Cough was present in 295(95%) patients. Chest pain was second most common symptom on presentation seen in 251(81%) patients.
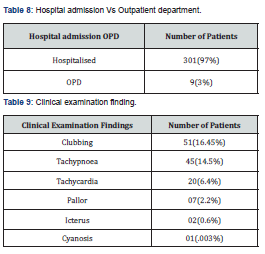
Dyspnoea was seen in 247(80%) while least common symptom was fever which was seen in 233(75%) patients (Table 7). Out of 310 patient who had complication due to tuberculosis 301(97%) patient were hospitalised and 9(3%) patients were treated on OPD basis (Table 8). Most common complication which leads to hospitalisation was post TB COPD with or without respiratory failure. In all post TB COPD patient most, common respiratory failure was type 2 RF. On clinical examination most common finding was clubbing seen in 51(16.45%) patients followed by tachypnea seen in 45(14.5%). Tachycardia was seen in 20(6.4%) patients; pallor was seen in 7(2.2%) followed by icterus in 2(0.6%). Cyanosis was least common clinical finding seen in 1(0.3%) patient out of 310 patients presented with complication of pulmonary tuberculosis (Table 9).
Discussion
Tuberculosis is a disease that has plagued humankind for centuries. In spite of excellent anti-tuberculous chemotherapy, a number of important complications of tuberculosis are still commonly seen. Some of these are caused by the disease, and others are the sequelae of therapy. Thus, some are seen immediately, and others occur months or even years after the onset of disease. Occurrence of complication can be seen as early as during active disease itself to even decades after last episode of tuberculous infection. Mean age in our study was 41.72 years. In most countries the F/M sex ratio in prevalent cases was similar or lower than that in notified cases, suggesting that F/M differences in notification rates may be largely due to epidemiological differences and not to differential access to health care [3-7].
In our study out of 310 patients enrolled in study 176(57%) were male where in 134(43%) patients were female. The main factor contributing to delay among women was described as fear of social isolation from the family or the community. Stigma was described as closely related to contextual factors such as gender-roles. Socio-economic status and level of education seemed to be mediated via denial and concealment of tuberculosis disease, thus causing delay. The main factor contributing to delay among men was described as fear of individual costs of diagnosis and treatment. In conclusion, there is a need for better understanding of behavioural factors and for developing strategies that take these into account. Health workers need to better understand gender and social aspects of tuberculosis control, particularly aspects that influence the likelihood for achieving equality in diagnosis and cure.
These complications may involve the lungs, mediastinum, pleura, chest wall, or any combination of these structures. This study was prospective observational study of complication of pulmonary tuberculosis, wherein 310 Patient were enrolled at tertiary care centre. Data was analysed to assess age, sex wise distribution, complications, microbiological correlation with sputum examination positivity (Gene Xpert, AFB smear and AFB culture), treatment taken, percentages of various complications, comorbidities was calculated. Pulmonary tuberculosis being infectious disease should be diagnosed and treated as early as possible to prevent its transmission and complication. Early diagnosis and adequate treatment is key in preventing tuberculosis spread and its complication. Many advances have come in diagnosis and management of tuberculosis but in poor economic country tuberculosis still contributes to significant morbidity and mortality [8-10].
The main reason for complication of tuberculosis is inaccessible health care facility, lack of infrastructure, insufficient manpower, lack of awareness about disease, insufficient testing facility, unavailability of anti-tubercular drug. Due to delay in diagnosis and treatment tuberculosis give rise to long term or short term complication which should be addressed swiftly to prevent morbidity and mortality. Our study was conducted at tertiary care centre and the patient were referred to us who were difficult to diagnose, treat or with complication either due to tuberculosis itself or due to anti-tuberculous treatment. There is not many studies who have studied complication of tuberculosis, in this we have highlighted various complication of pulmonary tuberculosis and their management.
Globally, 4.1% of new TB cases are reported to be MDR. Concordant with previous surveys our study recorded DSTB to be 95% and DRTB 5%. The First National Anti-Tuberculosis Drug Resistance survey conducted by the Indian Government in collaboration with the World Health Organization (WHO) and the United States Agency for International Development (USAID) showed that close to 23% of new cases have resistance to any drug with MDR-TB detected in 3% [11]. Mono-resistance to rifampin was not seen and resistance to isoniazid (INH) was highest (any 11%, mono-resistance 4%), followed by resistance to pyrazinamide (any 7%, mono-resistance 4%) and streptomycin (any 7%, mono-resistance 2%). Among patients previously treated for TB, there were high levels of resistance to first-line drugs-tested isoniazid (any 25%, mono-resistance 8%) followed by resistance to streptomycin (any 13%, mono-resistance 2%), pyrazinamide (any 9%, mono-resistance 4%) and ethambutol (any 7%, mono-resistance 0.21%) [11].
The high rates of drug resistance to both first-line and second-line drugs is alarming, but it is likely the survey is underestimating the true burden of resistance in India. The survey only included patients with smear-positive TB, excluding smear-negative TB and extra pulmonary TB, as well as patients diagnosed in jails and prisons. Most striking was the lack of involvement of the private sector, which may be treating more cases of TB than is currently estimated, with high rates of drug resistance reported from cities like Mumbai. India has set an ambitious goal of TB elimination by 2025. The large burden of DR-TB will limit progress towards that goal. Rarely, does the cliché ‘prevention is better than cure’ carry as much weight as it does with DR-TB. We believe that a multipronged strategy focusing on improving diagnostic capacity, guaranteeing high-quality treatment and preventing transmission will be central to meeting the challenge of DR-TB in India.
Obstructive airway disease has many causes tuberculosis, which can be a cause of this has not been studied in detail. Even the organisations, like GOLD and GINA, authority figures in chronic obstructive pulmonary disease (COPD) have not recognized, treated pulmonary TB as main etiological factor, which again shows that post pulmonary tuberculosis obstructive airway disease is a clinical entity in its infancy. Post tubercular impairment can manifest as reversible or irreversible obstructive airway disease, mixed defect or as pure restrictive defects. Cavitation, extensive fibrosis, bulla formation and bronchiectasis implicated in the genesis of COPD caused by the destroyed lung due to pulmonary tuberculosis. For many persons with tuberculosis, microbiological cure is just the beginning, not the end of their illness.
Post tuberculosis pulmonary impairment has emerged as a distinct clinical entity, which is almost indistinguishable from other forms and hence we review this topic further. Case control study by Pasipanodya et al comparing pulmonary function in prospectively identified pulmonary tuberculosis patients who had completed at least 20 weeks of therapy showed that airflow impairment was present in 59% of tuberculosis subjects. In our study 160(51%) patients had post tuberculosis COPD which is consistent with other studies available and it was the commonest complication. Pulmonary impairment associated with obstructive airways disease is recognised as a common complication of advanced tuberculosis. Post tuberculosis airway obstruction is a separate clinical entity. It requires insight, understanding and evaluation of its evolution, clinical course and management. The exact pathogenesis of the development of this disorder is unclear.
The time of occurrence of post-tuberculosis airway disease was variable, nearly 50% of the study group in various studies developed it within one year of stopping chemotherapy [1,12,], while the rest developed later [13]. Tuberculosis can cause chronic impairment of lung function which increases incrementally with the number of episodes of tuberculosis [13]. Only a few studies have been done to identify this entity, but all the studies have definitely concluded that such an entity exists. However, the exact abnormality that results from tuberculosis infection has to be considered in detail with future studies and a better understanding of the pathophysiology of airflow limitation may point the way to therapeutic strategies for control of symptoms in these patients.
Haemoptysis was second most common complication seen in our study. Haemoptysis is a common and potentially serious complication of pulmonary TB [14]. The incidence of haemoptysis in patients with pulmonary TB is reported to range from 15 to 35 percent in our study haemoptysis was seen in 58(18.7%) patients. Occurrence of haemoptysis does not imply that the TB is active. Haemoptysis may occur as the initial manifestation of active TB, during the course of treatment, or, even after the disease is apparently cured. Haemoptysis can be streaky or massive and life-threatening in most instances bed rest, sedation, and resuscitative measures aimed at restoring fluid balance and haemodynamic status control the bleeding. Broad spectrum antibiotics are administered to treat super- added bacterial infection. Anti-tuberculosis treatment is indicated in patients with active TB.
Spontaneous pneumothorax has been reported in 5 to 15% of patients with pulmonary TB [15,16]. In countries where TB is a common problem, it is an important cause of pneumothorax. In consensus with several other study our revealed that 4.8% patient had pneumothorax and 9.6% patient had empyema. Spontaneous pneumothorax may result from rupture of a sub pleural TB cavity into the pleural space. Infection of pleural cavity results in pyopneumothorax. Other causes of pneumothorax include rupture of an open healed cavity or rupture of a bleb or bulla secondary to fibrosis and destruction of the lung [16]. Pneumothorax and empyema were managed with intercostal drainage tube if pneumothorax or empyema was significant to cause dyspnea to the patient.
The occurrence of drug-induced hepatotoxicity is unpredictable, but it is observed that certain patients are at a relatively higher risk than others. The clinical presentation of ATT-associated hepatitis is similar to that of acute viral hepatitis. ATT can cause varied degree of hepatotoxicity from a transitory asymptomatic rise in transaminases to acute liver failure. The frequency of hepatotoxicity in different countries varies widely from 2% to 39%. In our study ATT therapy induced hepatitis was seen in 30(9.6%) patients. The incidence has been reported to be higher in developing countries and factors such as acute or chronic liver disease, indiscriminate use of drugs, malnutrition, and more advanced TB have been implicated.
A high incidence of viral hepatitis has been reported to coexist in patients with TB in developing countries, resulting in misdiagnosis of ATT-induced hepatotoxicity, especially if serological tests are not performed. Fatality due to ATT-induced hepatotoxicity was found to be more likely when jaundice occurred after 6 weeks of the initiation of therapy, serum bilirubin levels were higher, or the treatment was continued despite jaundice. Several studies have shown that pre-existing hepatic diseases due to chronic viral infections with hepatitis B or C or HIV, alcoholism, aging, and malnourishment increase the risk of developing drug-induced hepatitis.
The management of persistent Broncho pleural fistula is one of the most complex challenges encountered by the chest physician. Broncho pleural fistulae most commonly arise as a postoperative complication, but can occur in other clinical settings, such as inflammatory disease of the lung, blunt chest trauma, tuberculosis and barotrauma [12, 17-19]. The current incidence of BPF following pulmonary resection due to tubercular or non-tubercular causes is generally reported as 2 to 5 percent. BPF was seen in only 08(2.5%) patient which was the least common complication in our study. When BPF occurs, the healing and repair process is still associated with substantial morbidity and mortality, prolonged hospitalization, and great expense. Data regarding coexisting pulmonary thromboembolism (PTE) in patients with tuberculosis are limited. Coexistence of tuberculosis and PTE is seen in 1 to 3 % patient in several studies conducted previously.
Our study too had 9(3%) patients with PTE. Compared with unprovoked PTE, PTE with respiratory tuberculosis is characterized by lower body mass index, higher levels of blood inflammatory markers, higher PESI and less frequent central PTE, but it is not associated with any differences in outcomes caused by PTE. Outcome of complication of tuberculosis in various studies are 10 to 90 %. All the patient enrolled in our study had favourable outcome because of early diagnosis, effective anti-tubercular treatment, close monitoring, multi-disciplinary approach, supervised treatment and regular follow-up. Effective management of TB requires attention to potential structural, metabolic, vascular, and infectious complications. In some instances, individualizing treatment regimens may be necessary. Immunosuppression and other host factors predispose to complications; others occur despite adequate treatment. Public health TB programs and health systems require additional resources to provide comprehensive TB and post-TB care.
Comorbidities noted in our study were DM in 15(5%) patients, DM with HTN in 15(5%) patients, HTN and hypothyroidism in 7(2.2%) patients and IHD was least common seen in 4(1.2%) patients. Various studies have demonstrated non communicable disease in form of DM and HTN to be most common comorbidity seen in tuberculous infection in adult population while nutritional deficiency seen among children population. Various forms of complications may result from pulmonary tuberculosis. It is important to be aware of the full spectrum of clinical and radiologic features of the sequelae to facilitate diagnosis and management of the complications of pulmonary tuberculosis.
Conclusion
Pulmonary tuberculosis if inappropriately treated is associated with significant mortality and morbidity. Complication in tuberculosis are frequent occurrence and can occur in a patient during treatment or after finishing treatment. Common complication are post tuberculosis COPD, haemoptysis, ATT induced hepatitis, BPF (Broncho pleural fistula), Empyema, pneumothorax and PTE (pulmonary thrombo embolism). Timely detection of complication prevents mortality. Comorbidities adversely affects outcome in tuberculosis. All the complication due to pulmonary tuberculosis required mainly symptomatic management with therapy monitoring, weight adjusted ATT with supervision. Complication due to tuberculosis arises mainly due to delay in diagnosis and initiation of treatment which can be avoided by strengthening existing health care facility. This highlights the urgent need and importance of identifying, screening, optimally treating and supervising therapy in these patients in addition to programmatic advancements in management of complication of tuberculosis.
References
- Jyotsna Joshi (2009) Textbook of Pulmonary Medicine. Tuberculosis. Anti-Tuberculosis Therapy. First Edition 4(3): 111.
- Bidwell JL, Pachner RW (2005) Hemoptysis: diagnosis and management. Am Fam Physician 72(7): 1253-1260.
- Sharma SK, Mohan (1997) A Pulmonary tuberculosis: typical and atypical cases. Case track series 1. Mumbai: Merind.
- Reechaipichitkul W, Latong S (2005) Etiology and treatment outcomes of massive hemoptysis. Southeast Asian J Trop Med Public Health 36(2): 474-480.
- Macnee W (2002) Chronic Bronchitis and Emphysema: Seaton A, Seaton D, Leitch AG. Crofton and Douglas’s Respiratory Disease, Blackwell Science, United Kingdom, Pp: 616-617.
- Leitch AG (2002) Pulmonary tuberculosis: Clinical features in: Seaton A, Seaton D, Leitch AG, editors. Crofton and Douglass’s Respiratory Disease, Blackwell Science, United Kingdom, Pp: 523.
- Rajasekharan S, Savitri S, Jeyaganesh D (2001) Post tuberculosis bronchial Asthma. Ind J Tub 48: 139.
- Hnizdo E, Singh T, Churchyard GJ (2000) Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax 55(1): 32-38.
- (2018) Ministry of Health and Family Welfare GoI. Report of the first national anti-tuberculois drug resistance survey 2014-16.
- Arinaminpathy N, Batra D, Khaparde, T Vualnam, N Maheshwari, et al. (2016) The number of privately treated tuberculosis cases in India: an estimation from drug sales data. Lancet Infect Dis 16(11): 1255-1260.
- Dalal A, Pawaskar A, Das M, Ranjan D, Pralhad P, et al. (2015) Resistance patterns among multidrug-resistant tuberculosis patients in greater metropolitan Mumbai: trends over time. PLoS One 10(1): e0116798.
- DJ Pierson, CA Horton, PW Bates (1986) Persistent bronchopleural air leak during mechanical ventilation. A Review of 39 cases. Chest 90(3): 321-323.
- Kim HY, Song KS, Goo JM, Lee JS, Lee KS, et al. (2001) Thoracic sequelae and complications of tuberculosis. Radiographics 21(4): 839-858.
- Pamra SP, Goyal SS, Raj B, Mathur GP (1970) Epidemiology of haemoptysis. Indian J Tuberc 17: 111-8.
- Hussain SF, Aziz A, Fatima H (1999) Pneumothorax: a review of 146 adult cases admitted at a university teaching hospital in Pakistan. J Pak Med Assoc 49(10): 243-246.
- Borrego GJC, Rivas LP, Remacha EMA (2003) Recurrent tuberculous pneumothorax and tuberculous empyema: an association of two rare complications. Arch Bronconeumol 39(10): 478-479.
- G Malave, ED Foster, J A Wilson, DD Munro (1971) Bronchopleural fistula, present-day study of an old problem. A review of 52 cases. Ann Thorac Surg 11(1): 1-10.
- JR Hankins, JE Miller, Safuh Attar, JR Satterfield, JS McLaughlin, et al. (1978) Bronchopleural fistula, thirteen-year experience with 77 cases. J Thorac Cardiovasc Surg 76: 755-762.
- Steiger Z, Wilson RF (1984) Management of bronchopleural fistulas. Surg Gynecolobst 158(3): 267-271.






























