Reintubation After Planned Extubation - A Prospective Cohort Study Investigating Risk Factors and Outcomes in Critically Ill Patients
James S Krinsley1*, Michael A Bernstein1, Estella Rodriguez Alonso1, Nneka Nwachukwu1 and Marcus J Schultz2
1Department of Medicine, Stamford Hospital and Columbia Vagelos College of Physicians and Surgeons, USA
2Department of Intensive Care, Amsterdam University Medical Centers, Netherlands
Submission:February 24, 2021;Published:March 11, 2021
*Corresponding author: James S. Krinsley MD, Division of Critical Care, Department of Medicine, Stamford Hospital and Columbia Vagelos College of Physicians and Surgeons, 1 Hospital Plaza, Stamford, CT 06902 USA
How to cite this article: James S K, Michael A B, Estella R A, Nneka N, Marcus J S. Reintubation After Planned Extubation - A Prospective Cohort Study Investigating Risk Factors and Outcomes in Critically Ill Patients. Int J Pul & Res Sci. 2021; 4(5): 555650. DOI: 10.19080/IJOPRS.2020.04.555650
Abstract
Background: Failed extubation (FE) occurs in 2 to 25% of patients after planned extubation (PE), depending on the patient population studied.
Methods: Single-center retrospective analysis of consecutive patients undergoing invasive mechanical ventilation (MV) between May 2005 and July 2018. FE was defined as the need for reintubation within 48 hours of PE. Demographics, severity of illness scores and outcomes of FE were captured prospectively for all patients. Review of the electronic medical record was conducted to capture retrospectively relevant clinical characteristics close to each PE.
Results: Of 4,703 patients who underwent MV 2,898 had successful PE and 190 (6.2%) FE. Patients who had a FE were older (p=0.0153), more likely to be functionally dependent prior to MV (p<0.0001) and had higher APACHE III scores (p<0.0001) compared to those who had a successful PE. The most common reason for reintubation was hypoxic respiratory failure due to retained secretions (40.0%). FE was independently associated with ICU LOS >7 days (p<0.0001), MV >7 days (p<0.0001), and ICU mortality (p=0.0004), but not hospital mortality, and 34.7% required tracheostomy. The number of days of MV before planned extubation (p<0.0001), functional dependence (p=0.0002), APACHE III score (p=0.0484), nonoperative respiratory (p=0.0074) and neurosurgical admission (p=0.0225) were risk factors for FE.
Conclusion: In this large longitudinal single-center cohort, FE was independently associated with prolonged ICU LOS, MV days and ICU mortality. A longer duration of ventilation before PE, high severity of acute illness and functional dependency increased the risk of FE.
Keywords: Mechanical ventilation; Extubation; Reintubation; Respiratory failure; Intensive care unit
Abbreviations: APACHE: Acute Physiology and Chronic Health Evaluation; CPAP: Continuous Positive Airway Pressure; EMR: Electronic Medical Record; FE: Failed Extubation; ICU: Intensive Care Unit; IQR: Interquartile Range; LOS: Length of Stay; MV: Mechanical Ventilation; OR: Odds Ratio; PE: Planned Extubation; SD: Standard Deviation
Background
The timing of liberation from invasive mechanical ventilation (MV) is one of the most difficult decisions facing clinicians in the intensive care unit (ICU). Prolonged MV is associated with significant morbidity and risk of mortality [1]. Premature liberation from the ventilator can lead to failed extubation (FE), commonly defined as the need for reintubation within 24-72 hours of a planned extubation (PE). While a low rate of FE may reflect unnecessary caution, a high rate may suggest inadequate evaluation of the patient’s readiness for extubation readiness. The “optimal” rate of FE likely depends on the clinical characteristics of the patient population [2].
There is only limited literature describing the outcomes of patients who need reintubation after a planned extubation (PE) as well as the risk factors for FE3-9, and no single study has evaluated these two issues in the same cohort. The purpose of the current investigation is to fill this knowledge gap. The primary aim of this study was to determine the association between FE and clinically relevant patient-centered outcomes, including duration of MV, ICU LOS and ICU and hospital mortality, and need for tracheostomy. We also determined which factors have an independent association with FE. The tested hypotheses were that occurrence of FE worsens clinical outcomes, and that certain patient factors increase the risk of FE.
Methods
Patients
This investigation includes data from consecutive patients who received invasive MV between October 2005 and July 2018 in the mixed medical-surgical intensive care unit (ICU) of Stamford Hospital, a university-affiliated teaching hospital in Stamford, CT. The study protocol was approved by the local institutional review board that waived the need for individual informed consent.
Setting and extubation practice
Care in the unit was delivered by an intensivist-led team, round-the clock respiratory therapists and qualified nurses in a 1 to 2 to 1 to 1 nurse to patient ratio, depending on patient acuity. Liberation from the ventilator was guided by a respiratory therapist-driven protocols. The final decision to extubate a patient was made by the attending intensivist, based on integration of three general factors-consideration of patient’s overall medical status, a perceived capacity for the patient to successfully protect the upper airway after extubation, and demonstration of the patient’s capacity to tolerate low levels of MV support for at least 2 hours.
Data abstraction
Information abstracted from the ICU’s comprehensive database included patient demographics and comorbidities, ICU diagnosis, severity of illness scores (calculated prospectively by one of the authors (JSK) and entered prospectively into the database), duration of MV and ICU length of stay (LOS), and mortality status in ICU and in hospital discharge. In all patients, preadmission functional status was characterized on a 9-point scale and recorded prospectively in the database using all available information in the electronic medical record (EMR) at the time of ICU admission.
For the purpose of this investigation patients were characterized as being functionally independent, i.e., able to perform basic activities of daily living, or functionally dependent. Detailed review clinical characteristics captured in the electronic medical record at the time of planned extubation, including relevant ventilator settings, sedatives received and level of alertness, and upper airway characteristics. Causes of FE were also characterized and included hypoxic or hypercapnic respiratory failure and their etiologies, inability to protect the upper airway, and neurologic diagnoses.
Endpoints
The primary outcome was the association between FE and clinical outcomes, specifically total duration of invasive MV, ICU LOS, and ICU and hospital mortality. Secondary outcomes were risk factors for FE, and tracheostomy incidence in patients who had FE.
Statistical analysis plan
Continuous data are presented as mean (SD) or median (IQR) and compared using Student’s t test or the Mann Whitney rank sum test, as appropriate. Categorical data are presented as percentages and compared using Chi-square tests. We compared patients with FE to the patients who did not have FE after planned extubation.
We constructed multivariable models to assess the independent effects of FE on ICU mortality, hospital mortality, prolonged MV (>7 days) and prolonged ICU LOS (>7 days) as well as factors independently associated with FE. For each of these models we considered for inclusion relevant parameters that were significant at p value <0.05 and used backwards logistic regression to include in the final model all parameters that were significant at p value <0.10.
Results
Patients
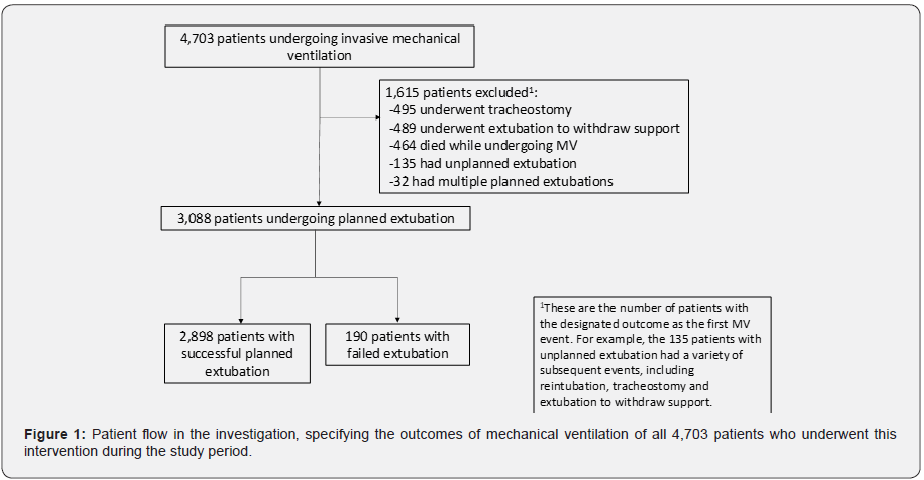
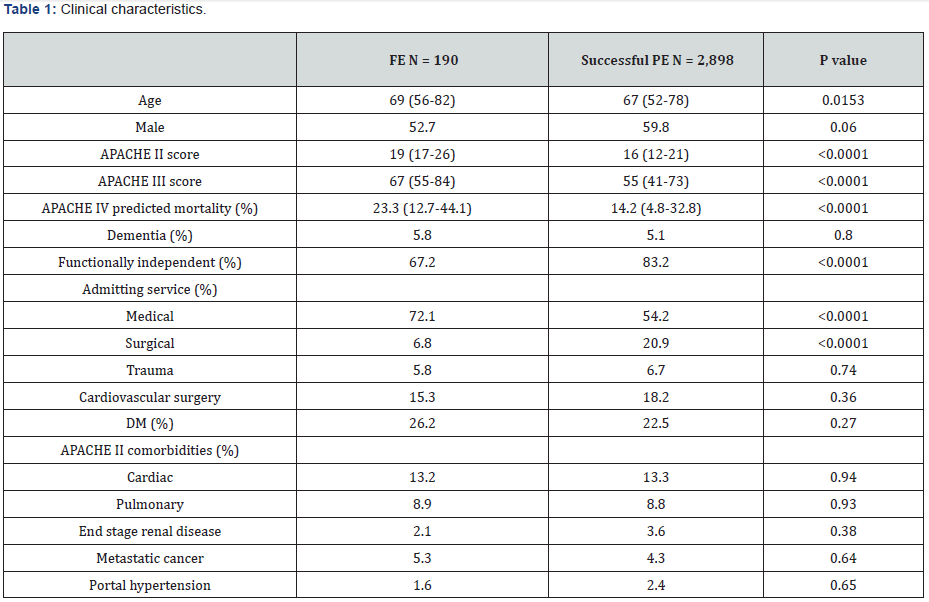
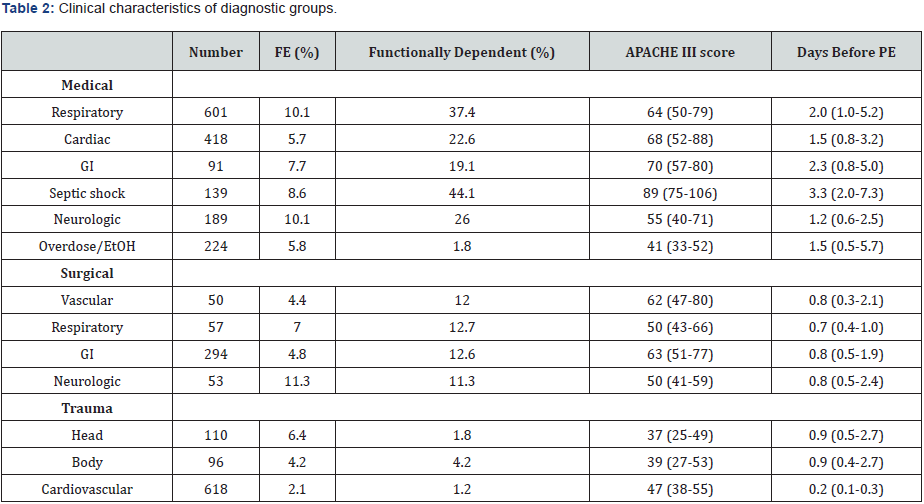
A total of 4,703 patients underwent invasive MV during the study period. Supplementary (Figure 1) illustrates patient flow. The cohort includes patients undergoing PE as their initial MV procedure. A total of 2,898 patients never required reintubation (i.e., had a successful PE) and 190 (6.2% of the cohort) had FE. (Table 1) details clinical characteristics of patients who had a FE compared to patients with successful PE. Patients who had a FE were older, had higher severity of illness scores, were more often functionally dependent prior to hospitalization and were more often admitted with medical rather than surgical diagnoses. Supplementary (Table 2) details clinical characteristics of patients based on specific diagnostic categories.
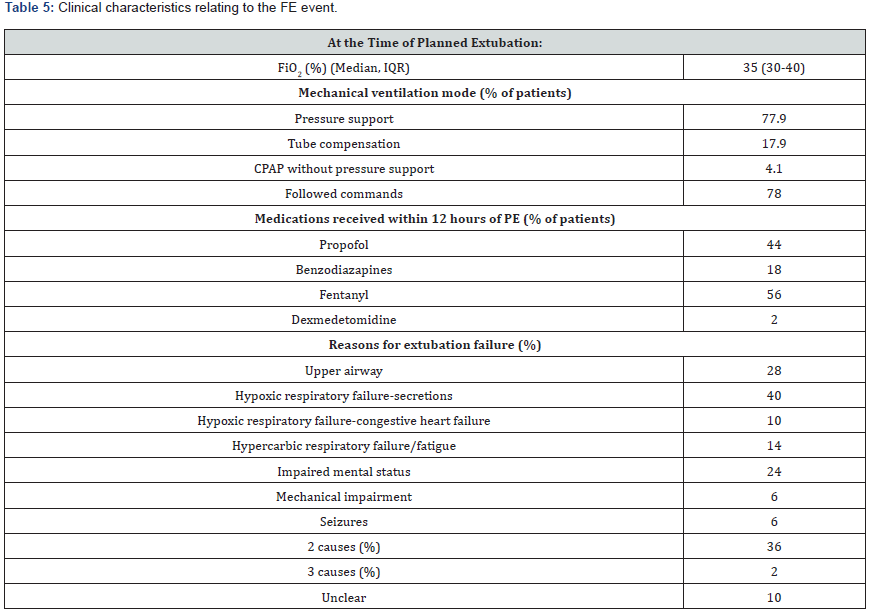
The rate of FE ranged from 2.1% for patients following cardiovascular surgery to 11.3% for patients following neurosurgical procedures. Among patients with non-surgical admitting diagnoses, those for respiratory (10.1%) and neurologic (10.1%) reasons had the highest rate of FE. The most common reason for reintubation was hypoxic respiratory failure due to the patient’s inability to clear upper airway secretions. Upper airway dysfunction, including edema and stridor, occurred in approximately one fourth of the patients, as did impaired mental status. Multiple causes of post extubation failure were seen in over one third; in 10% the cause could not be determined from review of the electronic medical record.
Association between FE and clinical outcomes
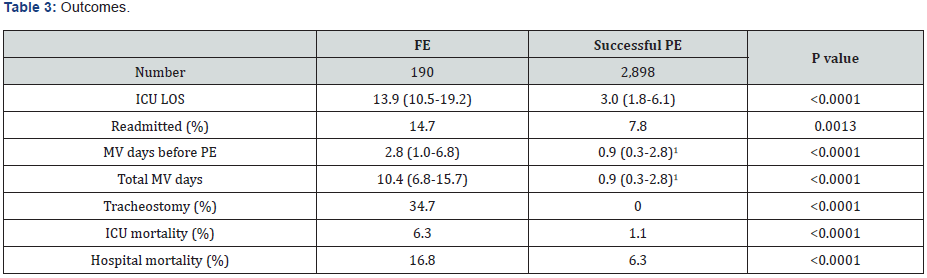
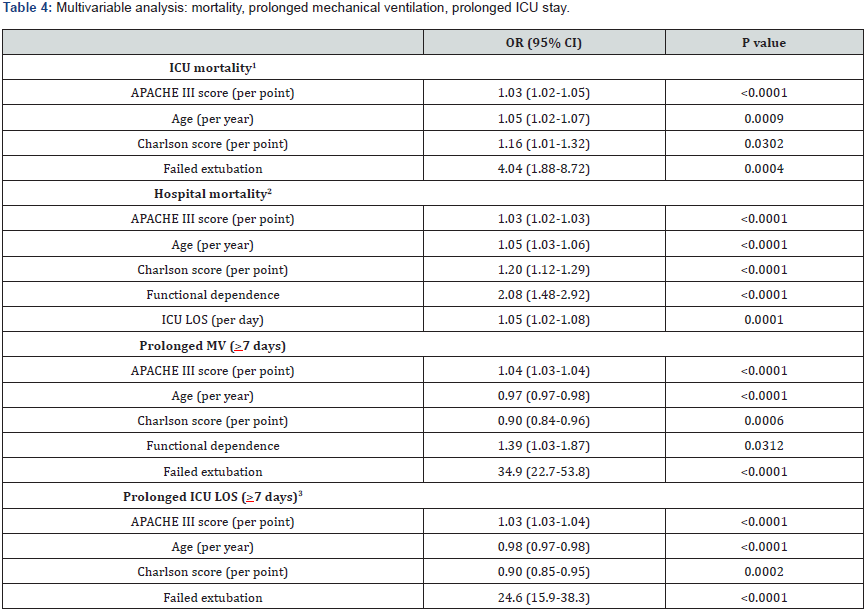
(Table 2) details clinical outcomes of patients with FE compared to those who did not need reintubation. Patients with FE had substantially longer ICU LOS and duration of mechanical ventilation. Their readmission rate to the ICU was nearly twice as high, compared to patients who had successful PE. More than one third underwent tracheostomy. Finally, ICU and hospital LOS were significantly higher. (Table 4) details the results of multivariable analysis, demonstrating that FE was independently associated with ICU mortality, prolonged MV and prolonged ICU LOS.
Risk factors for FE
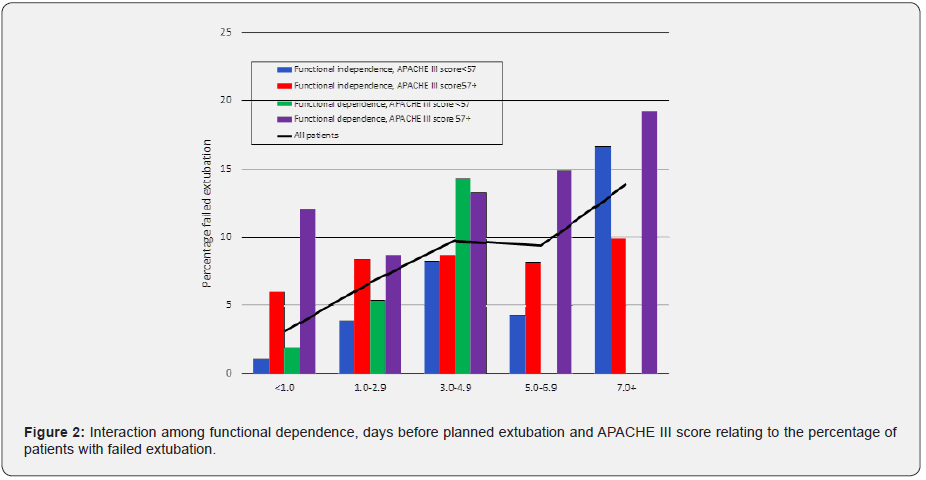
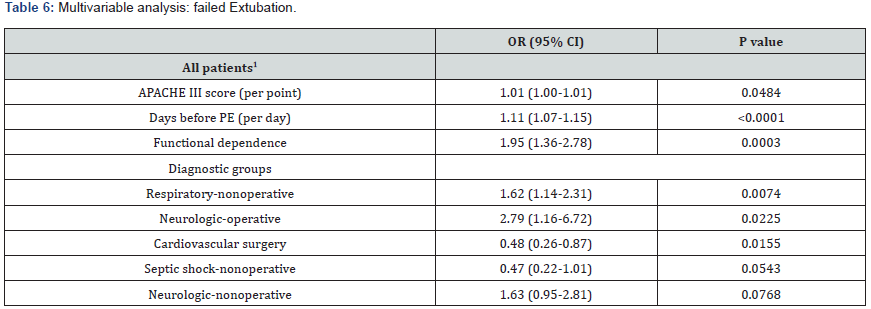
(Table 5) reports other clinical parameters at the time of PE and reasons for reintubation for the FE cohort. Most were extubated from the pressure support or tube compensation mode, using low levels of FiO2 and CPAP, instead of from a trial of spontaneous ventilation using t-piece. Nearly half had received fentanyl or propofol during the previous 12 hours; a much smaller percentage had received benzodiazepine or dexmedetomidine. A large majority were able to follow commands. (Table 6) details outcomes of multivariable analysis for factors independently associated with FE. In a model not including admitting diagnostic category these included: functional dependence, duration of MV before PE and APACHE III score. Additional multivariable models including diagnostic category demonstrate that nonoperative respiratory diagnoses and operative surgical diagnoses were independently associated with increased risk of FE and cardiovascular surgery diagnoses and nonoperative septic shock were independently associated with decreased risk of FE. (Figure 1) illustrates the rate of FE as a function of days of MV prior to PE, APACHE III and functional dependence. The OR (95% CI) of FE comparing patients who were functionally dependent and had >4 days of MV before planned extubation compared to those without these characteristics was 5.70 (3.54-9.18) (p<0.0001).
Discussion
This investigation of a large consecutive group of patients admitted to a mixed medical surgical ICU of a university affiliated teaching hospital demonstrates that failed extubation (FE) was independently associated with prolonged ICU LOS, prolonged duration of MV and ICU mortality. These patients often needed tracheostomy. The most common cause of respiratory failure requiring reintubation after planned extubation (PE) was retained secretions leading to hypoxia, followed by hypercarbia and altered mental status. The combination of >4 days of MV prior to PE and lack of functional independence identified a subgroup that was at very high risk of FE.
Relationship to prior literature
Previously published investigations of FE differed in their definitions (48 hours to 7 days after planned extubation); the patient populations studied; the choice of analysis of risk factors or clinical outcomes as the primary outcome of interest and the choice of potential risk factors for FE that were evaluated [2]. In addition, some studies were published more than 20 years ago, limiting their external validity in view of the numerous changes in clinical practice over this period. Most studies of FE include a relatively small number of patients with the sentinel event; to our knowledge the 190 patients with FE in the current investigation represents the largest single center cohort of such patients in the literature.
Risk factors for FE
A variety of clinical parameters have been evaluated in different investigations as potential risk factors for FE. These include severity of illness scores, such as APACHE II, age [3], rapid shallow breathing index, positive fluid balance [4] and the presence of chronic respiratory disease [5]. The duration of MV prior to PE was associated with risk of FE in one study [6] but not in all [5]. Other identified factors included the presence of severe left ventricular dysfunction and ICU acquired delirium [6]. Among a cohort of brain injured patients with a high rate of FE (22.7%), predictors of successful planned extubation included age <40, Glasgow Coma Scale score >10; the presence of visual pursuit and the presence of swallowing attempts by the patient, highlighting the broad diversity of predictive factor for FE that have been evaluated in the literature [7].
Jaber et al. [8] investigated a more contemporary cohort of 1,514 patients undergoing PE, among whom 157 (10.4%) required reintubation within 48 hours [8]. Of these, 45% had “airway” causes of FE, 50% “non-airway” causes and 5% a combination. Multivariable analysis determined that some risk factors were common to both mechanisms (coma as the reason for initiation of mechanical ventilation, ineffective cough) while others were associated with “airway” etiologies (copious secretions and mechanical ventilation >8 days) and others with “non-airway etiologies (respiratory failure and sequential organ failure assessment (SOFA) score).
The current investigation is unique in its determination that lack of functional independence, defined as the capacity to carry out the routine activities of daily living, and identified prospectively in the entire cohort, was independently associated with risk of FE. Frailty is increasingly recognized as being an important influence in the outcomes of patients with critical illness [9] and adds predictive value to standard mortality prediction models [10].
Causes of extubation failure
Epstein and colleagues evaluated the causes of FE in 74 medical ICU patients with FE, dividing these broadly into “airway” etiologies (upper airway obstruction (23.4%); retained secretions (25.5%)) and “non-airway” etiologies (respiratory failure (44.7%); CHF (36.2%); encephalopathy (14.9%)), with higher mortality noted among patients who had non-airway etiologies of extubation failure [11]. The reasons for reintubation after planned extubation in the study by Frutos-Vivar et al included increased work of breathing (45%); hypoxia (22%; not further specified); respiratory acidosis (11%); retained secretions (10%); decreased mental status (6%); hypotension (6%) (4).
Notably, these etiologies for extubation failure are similar to those observed in the current investigation, in which hypoxic respiratory failure from secretions (40.0%), upper airway dysfunction (28.0%), impaired mental status (24.0%), hypercarbic respiratory acidosis/fatigue (14.0%) and hypoxic respiratory failure due to congestive heart failure (10.0%) were the most common. Differences in patient population and the challenge of ascribing a unique cause of cause of the FE event likely explain these findings.
Outcomes of FE
Epstein reported that patients with FE had increased ICU LOS as well as higher hospital mortality compared to those with successful PE [3]. Most studies have confirmed that ICU LOS and duration of MV were longer in patients with FE than in those with successful planned extubation and that ICU or hospital mortality was higher [4-7,11]. However, multivariable analysis was not performed in these to demonstrate an independent association of FE with these outcomes. The current investigation demonstrated, using multivariable analysis, that FE was independently associated with prolonged MV, ICU LOS and ICU mortality.
Strengths and limitations
The large size of the cohort and its heterogeneous population of medical and surgical patients increases the external validity of the investigation. This study included a rich description of clinical characteristics and outcomes of the patients, many of which were collected in a uniform manner prospectively by a single author, increasing the reliability and completeness of the data. Several limitations must be mentioned. First, the study does not include all of the potential risk factors for FE evaluated in the other investigations referenced here. Second, the factors that were analyzed at the time of planned extubation were reviewed in the cohort with FE, but not in a matching cohort of patients without FE. Third, this is an observational investigation, thus all associations are not necessarily reflecting a causal relation. FE, though, cannot be the subject of a randomized clinical trial. Therefore, conclusions must be considered hypothesis-generating, rather than as proof of causality.
Clinical implications
Since FE is associated with adverse outcomes, attempts to prospectively identify patients at risk for this occurrence are potentially beneficial and apply to a broad population of patients admitted to the ICU. These factors-functional dependences, duration of MV prior to planned extubation, severity of illness upon presentation to the ICU and admission with operative or nonoperative neurologic diagnoses or nonoperative respiratory diagnoses. Notably, the combination of lack of functional independence prior to hospitalization and duration of MV >4 days identified a cohort that had a nearly 6-fold increase in the odds of FE. Identification of a patient at high risk of FE should prompt treating clinicians to be especially prudent regarding the decision to liberate the patient from MV. Future studies may focus on strategies, such as routine administration of high flow nasal oxygen [12] or noninvasive mechanical ventilation [13], diagnostic modalities such as diaphragmatic ultrasound [14,15] or predictive analytics [16] to prevent FE in these high-risk patients.
Conclusion
In this large single-center investigation of patients undergoing invasive MV, FE, defined as reintubation within 48 hours of PE, was independently associated with prolonged ICU length of stay, prolonged duration of mechanical ventilation and ICU mortality. FE patients frequently needed tracheostomy. Functional dependence prior to admission was independently associated with risk of failed extubation, a novel finding, as was duration of mechanical ventilation prior to planned extubation, severity of illness and admission to the ICU with neurologic diagnoses or nonoperative respiratory diagnoses. Prospective identification of patients at increased risk for failed extubation has the potential to inform clinical decision making and improve clinical outcomes.
References
- Esteban A, Anzueto A, Frutos F, Inmaculada A, Laurent B, et al. (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation: A 28-day international study. JAMA 287(3): 345-355.
- Krinsley JS, Reddy PK, Iqbal AS (2012) What is the optimal rate of failed extubation? Crit Care 16(1): 111.
- Epstein SK, Ciubotaru RL, Wong JB (1997) Effect of failed extubation on the outcome of mechanical ventilation. Chest 112(1): 186-192.
- Frutos-VF, Ferguson ND, Esteban A, Scott KE, Yaseen A, et al. (2006) Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest 130(6): 1664-1671.
- Thille AW, Harrois A, Schortgen F, Brun BC, Brochard L (2011) Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med 39(12): 2612-2618.
- Thille AW, Boissier F, Ben GH, Razazi K, Mekontso DA, et al. (2015) Risk factors for and prediction by caregivers of extubation failure in ICU patients: A prospective study. Crit Care Med 43(3): 613-620.
- Asehnoune K, Seguin P, Lasocki S, Antoine R, Adrien D, et al. (2017) Extubation success prediction in a multicentric cohort of patients with severe brain injury. Anesthesiology 127(2): 338-346.
- Jaber S, Quintard H, Cinotti R, Karim A, Jean MA, et al. (2018) Risk factors and outcomes for airway failure versus non-airway failure in the intensive care unit: a multicenter observational study of 1514 extubation procedures. Crit Care 22(1): 236.
- Muscedere J, Waters B, Varambally A, Sean MB, J Gordon B, et al. (2017) The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med 43(8): 1105-1122.
- Krinsley JS, Wasser T, Kang G, Bagshaw SM (2017) Pre-admission functional status impacts the performance of the APACHE IV model of mortality prediction in critically ill patients. Crit Care 21(1): 110.
- Epstein SK, Ciubotaru RL (1998) Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am J Resp Crit Care Med 158(2): 489-493.
- Hernandez G, Vaquero C, Gonzalez P, Carles S, Fernando FV, et al. (2016) Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA 315(13): 1354-1361.
- Nava S, Gregoretti C, Fanfulla F, Enzo S, Mario G, et al. (2005) Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med 33(11): 2465-2470.
- Vivier E, Muller M, Putegnat JB, Julie S, Stephanie B, et al. (2019) Inability of diaphragm ultrasound to predict extubation failure: A multicdenter study. Chest 155(6): 1131-1139.
- Haji K, Haji D, Canty DJ, Royse AG, Green C, et al. (2018) The impact of heart, lung and diaphragmatic ultrasound on prediction of failed extubation from mechanical ventilation in critically ill patients: a prospective observational pilot study. Crit Ultraound J 10(1): 13.
- Keim-Malpass J, Enfield K, Calland J, Lake D, Clark M (2018) Dynamic data monitoring improves predictive analytics for failed extubation in the ICU. Physiol Meas 39(7): 075005.






























