Iatrogenically Ruptured Pulmonary Hydatid Cyst Presenting as Haemoptysis - A Case Report
Sumit Mehra*
Department of Respiratory, Sleep, General and Acute Medicine, Flinders Medical Centre, Australia
Submission: March 25, 2018; Published: April 09, 2018
*Corresponding author: Sumit Mehra, Department of Respiratory, Sleep, General and Acute Medicine,Flinders Medical Centre, SA-5042, Australia, Tel: 61-0477412243; Email: sumitmeh2000@yahoo.com
How to cite this article: Sumit Mehra. Iatrogenically Ruptured Pulmonary Hydatid Cyst Presenting as Haemoptysis - A Case Report. Int J Pul & Res Sci. 2018; 3(1): 555604. DOI: 10.19080/IJOPRS.2018.03.555604
Abstract
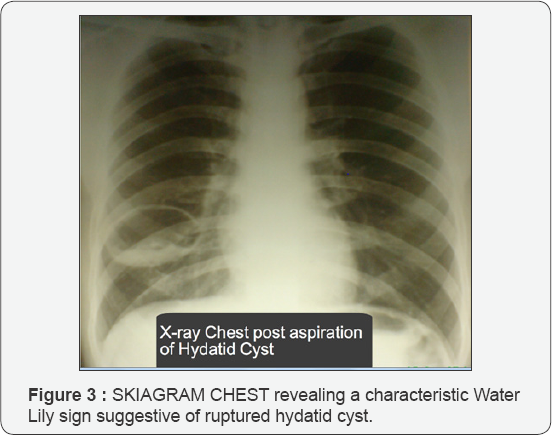
A 35-year-old male patient presented to us with complaint of massive haemoptysis. His chest radiograph revealed a characteristic water lily sign indicative of ruptured hydatid cyst. Patient then gave the history of inadvertent aspiration from the cyst by a private practitioner. Cystic fluid on examination had showed plenty of hooklets and scolices of Echinococcus granulosus. Diagnosis of hydatidosis was further confirmed by serology. Patient was then put on supportive treatment along with albendazole chemotherapy and he improved on them suggestive of efficacy of albendazole even in case of complicated hydatid cyst such as rupture.
Keywords: Haemoptysis; Hydatid cyst; Pulmonary hydatidosis
Introduction
Haemoptysis is one of the most dreaded manifestations of cardiopulmonary disease. Haemoptysis in adults is most often caused by tuberculosis, bronchitis, bronchiectasis, trauma or bronchogenic carcinoma [1]. We report here an unusual cause of massive haemoptysis, which was due to a ruptured pulmonary hydatid localized in the lungs and was misquandering as tuberculosis.
Case Report
A 28-year-old male patient was referred to us with complaints of massive haemoptysis that followed inadvertent aspiration of pulmonary cyst by a private practitioner. He further gave history of chest pain and cough with expectoration, of two years' duration that got aggravated following aspiration. He gave history of had taken antibiotics and antitubercular drugs in the past without any clinical improvement. He was non-smoker and nonalcoholic and had no history of diabetes and hypertension. His family history was also not significant. His general physical examination revealed pallor and weakness. His hemoglobin was 10gram percent, total leukocyte count was 11,600 cells/mL, differential count was P71, L19, M2, E8, B0 and E.S.R. (Westergreen) was 80mm/ hour. His X-ray chest (Figure 1) revealed a space-occupying lesion in lower zone of right hemi thorax. His CT Thorax (Figure 2) revealed a cystic lesion in right lung. His new X-ray chest was carried out and the aspirated fluid was sent for investigation. X-ray (Figure 3) revealed a characteristic Water Lily sign suggestive of ruptured hydatid cyst. Examination of the aspirated fluid showed hooklets, scolices and fragments of cyst wall resembling Echinococcus granulosus. Further serology was carried out to confirm the diagnosis. Antibodies to Echinococcus were significantly positive (1:18) by indirect haemagglutination test (IHA). Patient was ultimately started on high dose of oral albendazole therapy. Patient has clinicoradiologically (Figure 4) improved as on albendazole therapy and is presently asymptomatic.



Discussion
Larvae of the tapeworm Echinococcus cause echinococcosis or hydatid disease. Four species are recognized but Echinococcus granulosus causes the vast majority of infestations in humans. Hydatid disease may involve any organ of the body. However due to the effect of hepatic and pulmonary capillary sieves in containing the larvae, approximately 65% to 70% cysts occur in the liver followed by 15% to 30% in lungs. The remaining 3% to 5% cysts may be found virtually anywhere but most commonly in the spleen, kidney, brain and bones. Thus, liver and lungs are the two common sites of involvement in hydatid disease. Concomitant involvement of both liver and lung may be noticed in 10% of the cases [2], a condition given the name Hepatopulmonary Hydatidosis (HPH Disease) [3]. Isolated primary pulmonary hydatidosis with normal liver and no other sites of localization of the cyst is an unusual finding. Pulmonary echinococcal cysts are usually solitary but may be multiple in 20-30% cases [4]. It is further more common in children and less common in adults [5].
Hydatid disease may present with varied clinical manifestations. Involvement of lung by hydatid cyst may result in chest pain, chronic cough, expectoration, dyspnea, eosinophillic pneumonitis, pneumothorax, pleural effusion, parasitic lung embolism and even haemoptysis [6]. The mechanism of haemoptysis as in pulmonary hydatidosis may be due to pressure erosion of a bronchus or an obstructive effect with a bronchial infection. There may be occasional rupture of cyst into the bronchus resulting in massive haemoptysis as seen in the present case [7,8]. Underlying etiology for haemoptysis may be unknown in 20% of the cases [9]. Rupture of hydatid cyst can occur spontaneously and sometimes can be an initial manifestation of the occult disease. However it more commonly occurs after accidental aspiration of pulmonary hydatid cyst as in our case. In recent years percutaneous aspiration has been reported to be safe as the treatment of pulmonary hydatid cyst [10].
However it should be done under albendazole coverage and they should be punctured under US or CT guidance in the presence of an anesthesiologist who intervenes in cases of allergic manifestations or anaphylactic shock. But in this case aspiration was done accidentally and in unguided manner. Such a procedure has long been discouraged because of risks of anaphylactic shock and spillage of the fluid and this may even be lethal. Although surgery was earlier considered to be essential but now chemotherapy is considered as to be effective in treating pulmonary hydatidosis even if complications such as rupture occur. Galankis E et al. [11] reports a case of rupture of cyst in an 11-year-old boy with bacterial super infection who was treated with 3 courses of albendazole and recovered fully, uneventfully and without relapse. Even rupture following treatment with albendazole may occur [11,12]. However continuing albendazole in such cases also led to eventual cure of the disease [12]. Whether albendazole really increases the chances of cyst rupture remains to be answered. However, it is recommended that Albendazole should be continued even if the patient develops rupture of the cyst [13]. It should also be used in setting where the fluid leakage is not obvious like during surgery to minimize or eliminate the chances of recurrence and dissemination.
References
- Griffith DE, Girard WM, Wallace RJ (1993) Clinical features of pulmonary disease by rapidly growing mycobacteria: An analysis of 154 patients. Am Rev respire Dis 147(5): 1271-1278.
- Recep T, Sema O, Nuri S, Refik A, Ibrahim A, et al. (2002) Pulmonary hydatid cysts in children. Ann Med Sci 9: 59-62.
- Olgun KA, Fikret Kanat, Emel Turk, Mustafa UK (2002) Comparison between pulmonary and hepatopulmonary hydatidosis. Eur J Cardiothorac Surg 21(3): 489-496.
- McPhail JL, Arora TS (1967) Intrathoracic hydatid disease. Dis Chest 52(6): 772.
- Keramidas D, Mavridis, G, Soutis M, Passalidis A (2004) Pediatric Surgery International 19: 774-776.
- Eckert J, Deplazes P (2004) Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev 17(1): 107-135.
- Bharati S, Bharati B (2002) Hydatid disease of lungs - unusual cause of haemoptysis. Indian Pediatr 39: 1062-1063.
- Pandey A, Arya CL, Asthana AK (2007) Pulmonary hydatidosis: An unusual cause of haemoptysis. Indian J Med Microbiol 25(2): 158-160.
- Purriel P, Schantz PM, Beovide M, Medoza G (1973) Human ehiniococcosis in Uruguay: A comparison of indices of morbidity and mortality. Bull World Health Organ 49(4): 395-402.
- Akhan O, Ozmen MN, Dincer A (1994) Percutaneous treatment of pulmonary hydatid cyst. Cardiovasc Intervent Radiol 17(5): 271-275.
- Galankis E, Besis S, Pappa C, Nicolopoulos, Lapatsanis P (1997) Treatment of complicated pulmonary echinococcocis with albendazole in childhood. Scand J Infect Dis 29(6): 638-640.
- Talwar D, Dhariwal A, Gupta B, Gupta D (1990) Albendazole in Pulmonary hydatid disease J Chest Dis All Sci 32: 40237-40241.
- Parvaiz A Koul, Mohammad Khalil Kanjwal (2006) Albendazole Induced Rupture of Pulmonary Hydatid Cysts. The Internet Journal of Pulmonary Medicine 6: 1.






























