Detecting Psychiatric Comorbidity in Persons with Respiratory Diseases Using the New Free for Use Nimhans Screening Scale
Gayatri Saraf1, Santosh K Chaturvedi2*, Harish T2, Uma Buggi3 and Shashidhar Buggi3
1Maharashtra Institute of Mental Health, India
2National Institute of Mental Health and Neuro Sciences, India
3Rajeev Gandhi Institute of Chest Diseases, India
Submission: May 19, 2017; Published: July 27, 2017
*Corresponding author: Santosh K Chaturvedi, National Institute of Mental Health and Neuro Sciences, Bangalore, India
How to cite this article: Jolanda N, Hasan H, Roland H.Lung Function in Combined Pulmonary Fibrosis and Emphysema Syndrome, What to Expect. Int 002 J Pul & Res Sci. 2017; 2(1): 555578. DOI:10.19080/IJOPRS.2017.02.555578
Abstract
Background: Despite the high prevalence and morbidity of respiratory disorders, the psychological aspects have not received the same attention as other areas of general medicine such as heart diseases or cancer.
Aim/Objectives: To assess the psychiatric morbidity in outpatients with respiratory diseases using the NIMHANS screening scale.
Methods: Patients were consecutively selected from outpatient services of a tertiary care respiratory disease hospital over a period of 9 months. Patients were screened by a qualified psychiatrist for psychiatric morbidity using a 21-item screening scale. The 21 item screening scale has screening questions to assess for depression, anxiety, psychosis, substance use and chronic pain.
Results: A total of 85 patients were assessed. Majority of the patients were males (68%), with a mean age of 42.6 (±16.0) years, belonged to lower socio-economic strata (89%), were married (83%) and came from an urban background (73%). The most common respiratory diagnosis was pulmonary tuberculosis (52%), followed by chronic obstructive pulmonary disease (27%). 48% had a concomitant psychiatric diagnosis, 9% had been referred by the chest physician for psychiatric evaluation. 43% had substance abuse, the commonest being nicotine (25%). Mean score on NIMHANS screening questionnaire was 10.0±6.1. The tool was found to have a sensitivity of 0.71 and specificity of 0.77 in this population
Conclusion: NIMHANS 21 items scale is useful in detecting psychiatric co-morbidity in patients with respiratory diseases. Though psychiatric comorbidity including substance use in respiratory diseases is high, the rates of psychiatry referrals are quite low. Our study highlights the need to screen for psychiatric disorders in respiratory disease patients. Development and validation of short screening instruments for use by chest physicians and psychiatrists in medical settings would help in early detection and prompt treatment of psychiatric disorders in these settings.
Keywords: NIMHANS: National Institute of Mental Health and Neuro Sciences; ATT: Anti Tuberculosis Treatment
Introduction
Respiratory diseases are common, disabling and have far-reaching impact on an individual’s ability to perform the vital function of respiration independently. In respiratory disorders, functioning is impaired because of chronic pain breathlessness, dependence on nursing personnel and frequent hospitalisations [1].
Psychiatric issues are common in patients with respiratory disease [2]. Prevalence rates of as high as 19-40% for depression and 28-36% for anxiety have been reported in patients with COPD [3,4]. In a study, subclinical depressive symptoms that do not meet the diagnostic criteria were found to afflict as high as 25% of patients having COPD [4]. Studies also indicate significant comorbidity between asthma and anxiety, especially an elevated prevalence of generalised anxiety disorder and panic disorder [5,6]. Tuberculosis is also associated with a high rate of depression and anxiety [7,8]. In addition, psychiatric disorders and substance use lead to poor adherence to Anti Tuberculosis Treatment (ATT) and are associated with poor outcomes [9]. Comorbid psychiatric conditions also lead to greater disability [10].
There is a paucity of literature in the area of prevalence and correlates of psychiatric disorders in respiratory diseases. Most screening scales for psychiatric morbidity are very expensive. The objective of this study was to assess the pattern of psychiatric comorbidity in respiratory diseases using the National Institute of Mental Health and Neuro Sciences (NIMHANS) screening scale.
Methods
NIMHANS screening scale is a 21-item scale, with questions aimed at assessing for psychiatric caseness. It was reduced from 28 items. Item reduction and analysis was done on the developed 28 NIMHANS screening tool for psychological problems. It was administered on 50 normal subjects above 18 years of age. The tool was developed in English, Hindi and Kannada languages using back to back translation. Split half reliability of the tool is 0.84. Score of 11 and above indicates presence of psychiatric distress in normal populations. Discriminate validity has been developed with sensitivity of 0.76 and specificity of 0.82 [11]. It is free of any charges and can be obtained by writing to the author [SKC].
All patients then underwent a detailed psychiatric evaluation to assess for psychiatric morbidity. Psychiatric diagnosis was given after a psychiatric interview as per the ICD-10 classificatory system. Appropriate interventions were done for patients including pharmacotherapy and psychological interventions. The study was approved by the institutional ethics committee of Rajeev Gandhi Institute of Chest Diseases, Bengaluru, India.
]
Result
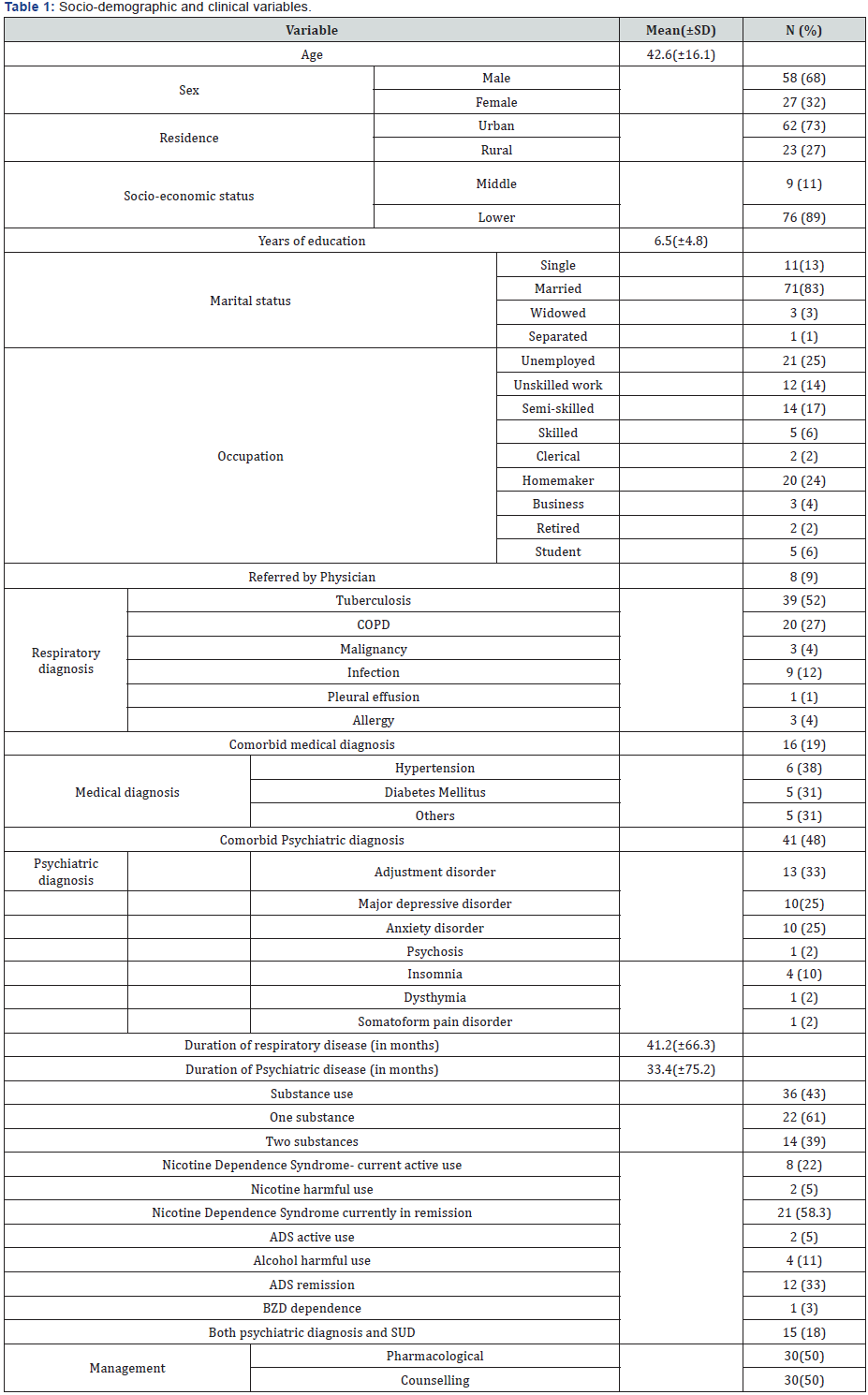
Majority of the patients were males (68%), with a mean age of 42.6 (±16.1) years, belonged to lower socio-economic strata (89%), were married (83%) and came from an urban background (73%). The mean years of education were 6.5 (±4.8) years, and the mean duration of the respiratory disease was 41 (±66) months. The most common respiratory diagnosis was pulmonary tuberculosis (52%), followed by chronic obstructive pulmonary disease (27%). 21% of the subjects had diagnosis such as infection, allergy, malignancy and pleural effusion. 19% of them also had a comorbid medical diagnosis such as diabetes, hypertension or dyslipidemia. Though 48% had a concomitant psychiatric diagnosis as per clinical assessment, only 9% had been referred by the chest physician for evaluation. The commonest psychiatric diagnosis as per ICD-10 classificatory system was adjustment disorder (32%), followed by major depression (25%) and anxiety disorders (25%). 43% had substance abuse, the commonest being nicotine (25%).

Of the 31 patients who were smokers, 14(45%) qualified for a psychiatric diagnosis (p-0.822%). Half (50%) of the 30 patients with tuberculosis qualified for a psychiatric disorder, however this was not statistically significant (p-0.824). A total of 33 patients scored above the cut-off score of 12 on the NIMHANS screening instrument of which 25 had a psychiatric diagnosis by clinical interview. Mean score on NIMHANS screening questionnaire was 10.0±6.1. The tool was found to have a sensitivity of 0.71 and specificity of 0.77 in this population at a cut-off score of 12 (Table 2).
Discussion
The study demonstrates a high prevalence (48%) of psychiatric disorders in patients with respiratory diseases. This is in line with previous studies which have demonstrated a high prevalence of depression [12,13], anxiety [3,14], panic attacks [15] and substance use [16] in respiratory diseases. Perhaps due to the high comorbidity between respiratory and psychiatric disease, the Global Initiative for Chronic Obstructive Lung Disease guidelines recommend that all COPD patients should be assessed for feelings of depression and anxiety [17].
Half of the patients with tuberculosis were found to have a psychiatric disorder. This confirms previous studies which have found a high psychiatric morbidity in tuberculosis. Factors such as stigma, isolation, psychological reaction to disclosure of diagnosis and side effects of Anti Tuberculosis Treatment (ATT) are said to explain higher rates of psychiatric morbidity. Psychiatric disorders when present may adversely impact adherence, leading to relapse and multi-drug resistance.
We found a high prevalence of substance use disorders (43%) in patients with respiratory disease, the commonest being nicotine (25%). Close to half (45%) of smokers in this study qualified for a psychiatric disorder. Approximately 10-15% of smokers develop COPD [18]. Smokers are also at a higher risk of developing lung cancer, interstitial lung diseases and bronchial asthma [19]. Moreover, smokers also benefit from quitting in terms of improvement in lung parameters [20]. Towards that effect, smoking cessation programs have been found to be useful in respiratory diseases [21].
Recognising psychiatric disorders in general hospitals becomes difficult because Psychiatric services may not always be available. Moreover, even in hospitals where liaison services are present, it is not feasible to screen all patients due to cost, time and manpower involved. Hence screening instruments validated for use in the respiratory disease populations are needed in order to rapidly assess and detect psychiatric disorders [11-14]. These screening instruments need to be simple, effective and easy to use by physicians and general practitioners in primary care and chest medicine settings where a qualified psychiatrist might not always be available. There is a need for setting upconsultation- liaison services in chest medicine hospitals.
Conclusion
Psychiatric morbidity is common in patients with respiratory disorders, however most are not detected or referred by the physicians. The NIMHANS screening scale is an effective, way of rapid assessment and screening in respiratory diseases, at no cost. The tool also has a good sensitivity and specificity in this population, which render it useful in these settings.
References
- Moussas G, Tselebis A, Karkanias A, Stamouli D, Ilias I, et al. (2008) A comparative study of anxiety and depression in patients with bronchial asthma, chronic obstructive pulmonary disease and tuberculosis in a general hospital of chest diseases. Ann Gen Psychiatry 7(1): 7.
- Wells KB, Golding JM, Burnam MA (1988) Psychiatric disorder in a sample of the general population with and without chronic medical conditions. Am J Psychiatry 145(8): 976-981.
- Di Marco F, Verga M, Reggente M, Maria Casanova F, Santus P, et al. (2006) Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir Med 100(10): 1767-1774.
- Yohannes AM, Baldwin RC, Connolly MJ (2006) Depression and anxiety in elderly patients with chronic obstructive pulmonary disease. Age Ageing 35(5): 457-459.
- Katon WJ, Richardson L, Lozano P, McCauley E (2004) The relationship of asthma and anxiety disorders. Psychosom Med 66(3): 349-355.
- Hasler G, Gergen PJ, Kleinbaum DG, Ajdacic V, Gamma A, et al. (2005) Asthma and panic in young adults: a 20-year prospective community study. Am J Respir Crit Care Med 171(11): 1224-1230.
- Aydin IO, Uluşahin A (2001) Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: applicability of GHQ-12. Gen Hosp Psychiatry 23(2): 77-83.
- Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, et al. (2014) Prevalence and associated factors of depressive state among pulmonary tuberculosis patients in Manila, The Philippines. Int J Tuberc Lung Dis 18(2): 174-179.
- Pachi A, Bratis D, Moussas G, Tselebis A (2013) Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013: 489865.
- Kim HF, Kunik ME, Molinari VA, Hillman SL, Lalani S, et al. (2000) Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics 41(6): 465-471.
- Sharma MK, Chaturvedi SK (2014) Development and validation of NIMHANS screening tool for psychological problems in Indian context. Asian J Psychiatr 10: 33-38.
- Negi H, Sarkar M, Raval AD, Pandey K, Das P (2014) Presence of depression and its risk factors in patients with chronic obstructive pulmonary disease. Indian J Med Res 139(3): 402-408.
- Heaney LG, Conway E, Kelly C, Gamble J (2005) Prevalence of psychiatric morbidity in a difficult asthma population: relationship to asthma outcome. Respir Med 99(9): 1152-1159.
- Centanni S, Di Marco F, Castagna F, Boveri B, Casanova F, et al. (2000) Psychological issues in the treatment of asthmatic patients. Respir Med 94(8): 742-749.
- Goodwin RD, Pine DS (2002) Respiratory disease and panic attacks among adults in the United States. Chest 122(2): 645-650.
- Lebowitz MD (1981) Respiratory symptoms and disease related to alcohol consumption. Am Rev Respir Dis 123(1): 16-19.
- Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, et al. (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176(6): 532-555.
- (1996) Cigarette smoking and health. American Thoracic Society. Am J Respir Crit Care Med 153(2): 861-865.
- Anderson DO (1964) Smoking and respiratory disease. Am J Public Health Nations Health 54(11): 1856-1863.
- Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, et al. (2000) Smoking Cessation and Lung Function in Mild-to-Moderate Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 161(2 pt 1): 381-390.
- Tønnesen P, Carrozzi L, Fagerström KO, Gratziou C, Jimenez-Ruiz C, et al. (2007) Smoking cessation in patients with respiratory diseases: a high priority, integral component of therapy. Eur Respir J 29(2): 390- 417.






























