Epidemiological features of papillary carcinoma of the breast in a developing community
Wilson IB Onuigbo*
Department of Pathology, Medical Foundation and Clinic, Nigeria
Submission: October 27, 2016; Published: December 09, 2016
*Corresponding author: Wilson IB Onuigbo, Department of Pathology, Medical Foundation and Clinic, 8, Nsukka Lane, Enugu 400001, Nigeria, Email:wilson.onuigbo@gmail.com
How to cite this article: Wilson I O. Epidemiological features of papillary carcinoma of the breast in a developing community. Int J cell Sci & mol biol. 2016; 1(3): 555561. DOI:10.19080/IJCSMB.2016.01.555561
Abstract
A separate challenge in characterizing papillary carcinoma of the breast is related to the fact that a large proportion of the literature consists of individual case reports. The scarcity of information was remedied from certain centers. The present paper seeks, therefore, to add materials obtained from a histopathology data pool covering the Ibo or Igbo Ethnic Group domiciled in a developing community in Nigeria.
Keywords: Breast Cancer; Papillary; Developing community; Nigeria
Introduction
In presenting an overview of papillary carcinoma of the breast, Pal’s associates [1] asserted thus: “A separate challenge in characterizing papillary carcinoma is related to the fact that a large proportion of the literature devoted to this entity is comprised of individual case reports.” Therefore, the present paper considers materials accruing from a histopathology data pool such as the one established in Birmingham (UK) for facilitating epidemiological analysis [2]. In particular, papillary breast carcinomas of the Ibo or Igbo Ethnic Group, which is domiciled in the South Eastern part of Nigeria [3], are analyzed.
Investigation
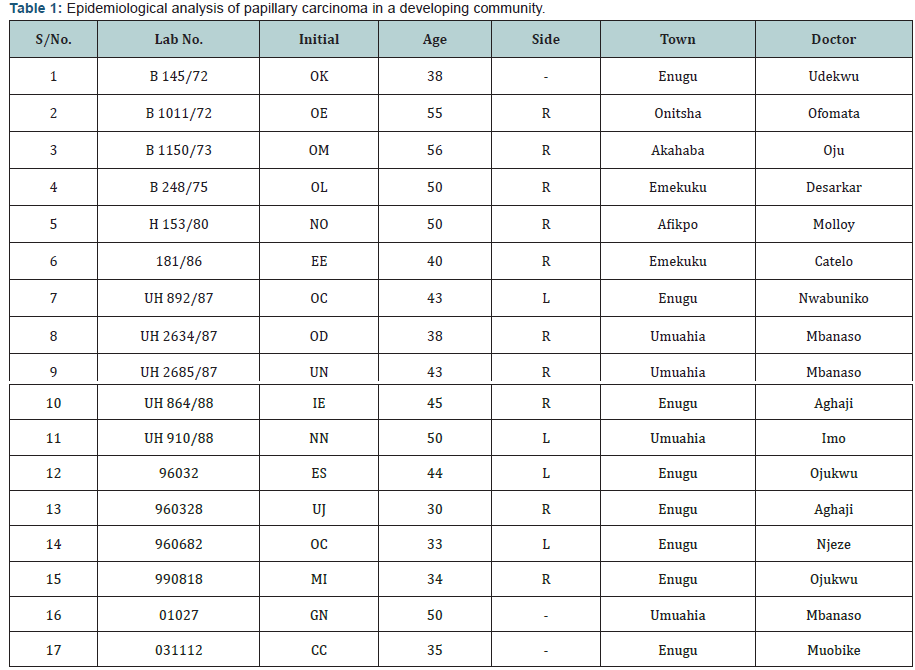
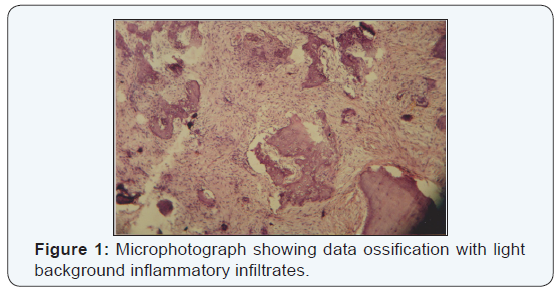
From the 1970s, the author received at a Reference Pathology Laboratory situated in Enugu, the capital city of the Eastern Region of Nigeria, biopsy specimens together with detailed information. The data are analyzed in respect of papillary carcinoma of the breast in Table 1(Figure 1).
Discussion
Tabulation elevates Enugu, the cosmopolitan city, with 7 cases, i.e., almost half of the series. Interestingly, Dr .Aghaji preponderated with 2 cases, the rest being distributed among 5 individual doctors. As for the remaining half of the cases, Dr. Mbanaso preponderated with 3 cases, while Missionary Hospitals took pride of place in the remainders. Incidentally, Dr. Mbanaso himself co-authored with me the important message concerning the usefulness of a centrally based Laboratory to a distant hospital [4]. This is important because there was argument in UK about distance militating against the usefulness of such a laboratory [5].
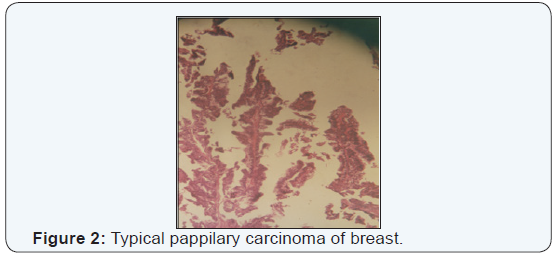
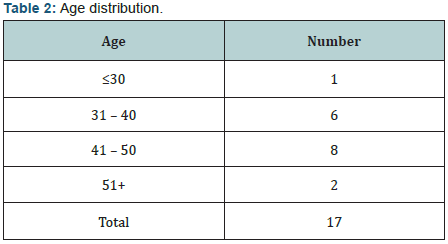
It is worth noting that all the above personal cases were distinctly invasive. This is unlike the many reports on encapsulated papillary carcinoma [6-9] and even the intracystic variety [10, 11]. Of course, explanations were attempted in all of them (Table 2) (Figure 2).
It was better appreciated elsewhere. Thus, as in the previously mentioned article [1], “The scarcity of information underscores the need for further treatment- and outcome-related studies in papillary carcinoma of the breast.” On the other hand, by calling it “solid papillary carcinoma” [12], it was defined as a “distinctive form of papillary carcinoma characterized by closely apposed expansive, cellular nodules.”
In contrast, I am persuaded that my documented examples bore the imprint of their picturesquely papillary. Thus, my descriptions ranged across “frankly papillary,” “marked papillary arrangement,” and “thrown into papillary folds.” In other words, as Pal and colleagues appreciated [1], “Distinction of invasive papillary carcinoma from non-invasive forms is critical, as each entity carries a unique prognosis.” In the words of Rakha’s group [6], “However, the classification of papillary carcinoma (whether they are in situ or invasive), its behavior, and management remain a matter of debate.” No! Such debate should not continue.
References
- Pal SK, Lau SK, Kruper L, Nwoye U, Garberoglio C, et al. (2010) Papillary carcinoma of the breast: An overview. Breast Cancer Res Treat 122(3): 637-645.
- Macartney JC, Rollaston TP, Codling BW (1980) Use of a histopathology data pool for epidemiological analysis. J Clin Pathol 33(4): 351-353.
- Basden GT (1966) Niger Ibos. Cass, London, UK.
- Onuigbo WIB, Mbanaso AU (2005) Urban histopathology service for a remote Nigerian hospital. Bull Roy Coll Pathol 132: 32-34.
- Lilleyman J (2002) From the president. RC Path Bull Roy Coll Pathol 117: 2-3.
- Rakha EA, Gandhi N, Climent F, et al. (2011) Encapsulated papillary carcinoma of the breast: An invasive tumor with excellent prognosis. Am J Surg Pathol 35(8): 1093-1103.
- Rakha EA, Varga Z, Elsheik S, Ellis IO (2014) High-grade encapsulated papillary carcinoma of the breast: an under-recognized entity. Histopathology 66(5): 740-746.
- Richards S, Li Y, Loffe O (2016) Encapsulated and solid papillary carcinoma of the breast: Case reports and review of clinicopathologic features. Pathol Case Rev 21(1): 32-36.
- Chauhan K, Monika G (2016) An unusual case of encapsulated papillary carcinoma of breast. J Cancer Metas Treat 2: 224-227.
- Reefy SA, Kamesshki R, Sada DA, Elewah AA, Awadhi AA, et al. (2013) Intracystic papillary breast cancer: a clinical update. Ecancermedicalscience 7: 286.
- Benkaddour YA, Hasnaoui SE, Fichtali K, Fakhir B, Jalal H, et al. (2012) intracystic papillary carcinoma of the breast: Report of three cases and literature review. Case Rep Obstet Gynecol, 2012: 979563.
- Tan BY, Thike AA, Ellis IO (2016) Clinicopathologic characteristics of solid papillary carcinoma of the breast. Am J Surg Pathol 40(10): 1334- 1342.





























