Expectant Management of Retained Products of Conception Compered Surgical and Drug Treatment Following Missed Abortion
Maryam Ahmadi1*, Elaheh Talebi Ghane2 and Zahra Maleki Delarestaghi1
1Department of Obstetrics and Gynecology, School of Medicine Fatemieh Hospital, Hamadan University of Medical Sciences. Hamadan Iran
2Modeling of Noncommunicable Diseases Research Center, Hamadan University of Medical Science, Hamadan Iran
Submission: February 27, 2024; Published: March 07, 2024
*Corresponding author: Maryam Ahmadi, Department of Obstetrics and Gynecology, School of Medicine Fatemieh Hospital, Hamadan University of Medical Sciences, Hamadan, Iran
How to cite this article: Maryam Ahmadi*, Elaheh Talebi Ghane and Zahra Maleki Delarestaghi. Expectant Management of Retained Products of Conception Compered Surgical and Drug Treatment Following Missed Abortion. Glob J Reprod Med. 2024; 10(5):555798. DOI: 10.190880/GJORM.2024.10.555798.
Abstract
Background: Surgical intervention is the standard treatment for retained products of conception (RPOC) following pregnancy. However, due to the complications associated with surgical methods, alternative therapeutic approaches are practiced as well. The treatment outcomes for RPOC in patients who experienced either miscarriage or legal abortion before 22 weeks of gestation were examined.
Methods: A total of 598 patients diagnosed with RPOC based on clinical findings and sonography between 2021 and 2022 at Fatemieh Hospital (Hamadan, Iran) were examined. They were assessed for clinical characteristics, self-expulsion, severe bleeding, haemoglobin levels, and the need for additional curettage.
Results: Out of 205 patients treated with medication, 178 cases (86%) had successful treatment. Among 146 patients with conservative management, 98 cases (67%) were treated successfully. Additionally, out of 247 patients treated surgically, 244 cases (98%) achieved successful expulsion without the need for further interventions (P<0.001). All patients receiving medical treatment and half of those treated through conservative management who did not have a successful expulsion underwent curettage. In both non-surgical treatment groups, the volume of retained products was greater in cases with unsuccessful expulsion. This difference was not significant in medical treatment; however, it was statistically significant in patients with conservative treatment. In total, 17 patients (2.8%) experienced a decline in haemoglobin levels, with 10 patients (4.1%) in the surgical group, four patients (7.2%) in the medical treatment group, and three patients (1.5%) in the surgical treatment group (P>0.05).
Conclusion: Medical and conservative management can serve as alternatives to surgical intervention in patients with RPOC, especially those with a thinner endometrial thickness.
Keywords: Abortion; Curettage; Conservative management; Retained products of conception
Abbreviations: Retained Products of Conception (RPOC); Dilatation and Curettage (D&C); THR: Transcervical hysteroscopic resection
Introduction
Retained products of conception (RPOC) refer to fetal or placental tissue that remains in the uterine cavity after pregnancy [1]. Diagnostic criteria for RPOC are an ongoing debate, which have not achieved unanimous consensus. Clinical manifestations of RPOC during the first three months of pregnancy may include prolonged or excessive vaginal bleeding, lower abdominal pain with or without fever, delayed return to menstruation, and a positive pregnancy test, along with sonographic findings consistent with RPOC following miscarriage [2]. Supportive sonographic findings for diagnosing RPOC include an echogenic mass within the endometrial cavity and the presence of low-resistance Doppler flow. However, endometrial thickness alone may not be indicative of RPOC in the absence of clinical symptoms [3]. Recent developments regarding the diagnosis and incidence of this condition have witnessed two significant changes. One pertains to the increased utilization of assistive procedures, which has led to a rise in its incidence compared to previous figures [4].
The second change relates to the enhanced diagnostic capability of colour Doppler ultrasonography, especially in patients with a history of miscarriage. RPOC, particularly when hyper vascular, can induce severe haemorrhage. The natural course of RPOC is not well-understood, and it remains unclear which patients may experience significant bleeding during expectant management [5]. Surgical interventions, including dilatation and curettage (D&C) or transcervical hysteroscopic resection (TCR), are certainly reliable and effective for RPOC; however, they are associated with multiple complications such as intraoperative bleeding and the potential risk of infertility [4,6]. Recent years have seen an increasing inclination towards more conservative approaches. However, it is important to note that findings from studies in this context exhibit conflicting results, given differing study designs [7,8]. The aim of this cohort retrospective study was to provide insights into the outcomes of conservative management, medical treatment, and surgical intervention for RPOC in patients with a gestational age of less than 22 weeks following miscarriage or legal abortion.
Materials and Methods
This cohort retrospective study was conducted from2021 to 2021 at Fatemieh hospital. The research design was approved by the Ethics Committee of Hamadan (Iran)university of medical since under the ID: UMSH.REC.1401.653. Patients who had experienced a legal abortion or missed abortion with a gestational age of less than 22 weeks and were diagnosed with RPOC based on both sonographic findings and the specialist’s medical opinion were included in the study. Patients who were not accessible for follow-up were excluded from the study. Patients were categorized into four groups based on the results of sonographic findings related to RPOC (less than 10 mm, 10 to 15 mm, 15 to 20 mm, and 20 to 50 mm). Patients were divided into three treatment groups: curettage, medical treatment with misoprostol, and conservative management with follow-up sonography. Surgical treatment was performed under general or spinal anaesthesia in a lithotomy position using a curette or curettage.
Conservative management was carried out for stable patients with follow-up sonography, while medical treatment followed a standardized protocol, the details of which have been previously examined [9]. Patients who received misoprostol didn’t receive antibiotics. Data collection included variables such as age, gender, parity, gravidity, BMI, gestational age, history of miscarriage, sonographic findings, self-expulsion, occurrence of severe bleeding, haemoglobin drop, and the need for repeat curettage. All patients were followed up after the completion of menstruation in the subsequent cycle, and patients who underwent curettage were not followed further. The data were analysed using SPSS v23 (p<5%). Quantitative variables were presented as means and standard deviations, and qualitative variables were presented as frequencies and percentages. Independent t-tests and ANOVA were used to compare quantitative variables between two groups. Chi-squared or Fisher’s exact tests were utilized to compare qualitative variables between groups.
Results
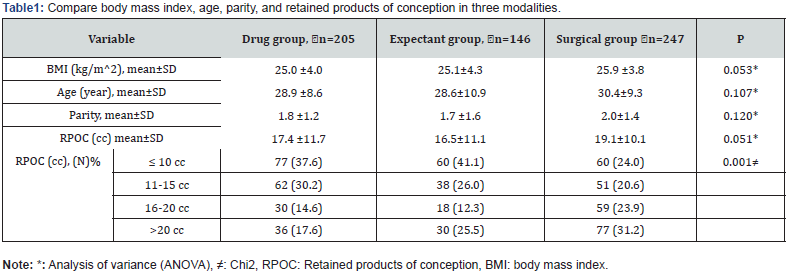
Out of 598 patients, 247 individuals (41.3%) underwent surgical curettage, 205 (34.3%) received medical treatment with misoprostol, and 146 patients (24.4%) received conservative management and follow-ups using sonography. No statistically significant differences were observed between the three groups in terms of body mass index, age, live birth count, and the volume of retained products of conception based on sonographic findings. However, when analysing the thickness of the remaining volume, the highest thickness was observed in patients who underwent curettage, and the lowest thickness was related to patients who received conservative management. Nevertheless, the Bonferroni post hoc test demonstrated that there were no statistically significant differences among the three groups. The highest thickness was observed in women who underwent surgery treatment (Table 1). Out of the 205 patients who received medical treatment, 178 patients (86.8%) successfully explained the retained products of conception, and out of the 146 patients in the conservative management group, 98 patients (67.1%) had complete expulsion without the need for surgical intervention. Among the 247 patients who underwent dilatation and curettage (surgical treatment), 244 patients (98%) successfully explained the retained products without the need for further interventions. A chi-squared test showed that there was no statistically significant difference among the three treatment groups (P<0.001, X2=81.1). Additionally, pairwise comparisons between the groups showed statistically significant differences (Figure 1) (P<0.001).
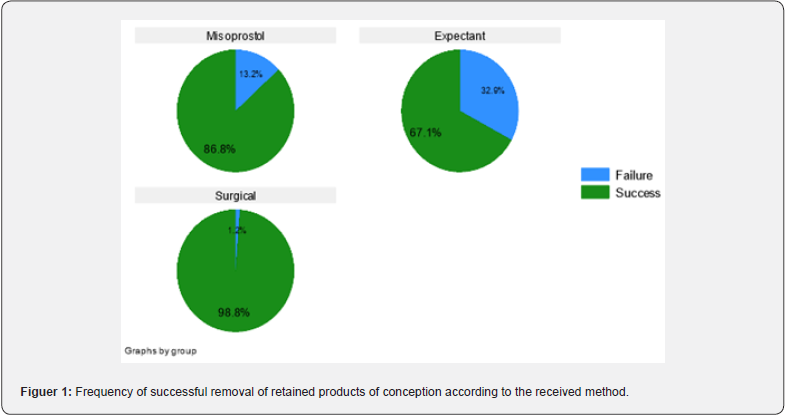
All patients who initially received medical treatment and did not have successful expulsion eventually underwent surgical intervention. Half of the patients in the conservative management group who did not achieve successful expulsion received surgical treatment, while the remaining half successfully explained the retained products with medication. Among the patients who had previously undergone surgery and still had retained products, three patients were treated again, with two of them receiving medical treatment and one patient undergoing surgical intervention. In total, 17 patients (2.8%) experienced a decline in haemoglobin levels, with 10 patients (4.1%) in the surgical group, four patients (2.7%) in the medical treatment group, and three patients (1.5%) in the surgical treatment group. Additionally, a total of four patients (0.7%) experienced sepsis, with two patients in the conservative management group, one patient in the surgical treatment group, and one patient in the medical treatment group, and there was no statistically significant difference between the three treatment groups regarding both outcomes. In both nonsurgical treatment groups, patients who did not have a successful treatment had a higher volume of retained products of conception. This difference was statistically significant in the medical treatment group but not in the conservative management group.
Discussion
Furthermore, nearly all patients (98.8%) who underwent surgical intervention achieved successful expulsion. However, it is important to note that this method may lead to severe bleeding during surgery and necessitate hysterectomy in some cases. Moreover, surgical management may result in intrauterine adhesions (Asherman’s syndrome), which can subsequently lead to infertility, recurrent miscarriages, or abnormal uterine anatomy [3]. An alternative approach to curettage, combined with dilatation and curettage, is hysteroscopic resection, which has shown a lower risk of intrauterine adhesions, more effective removal of uterine contents, and a reduced risk of infertility compared to curettage. Nonetheless, this method requires sufficient experience and access to more advanced equipment, which may be less readily available in certain healthcare facilities [10]. Recent findings from a study demonstrate that hysteroscopic resection, compared to dilation and curettage (D&C), offers the advantage of earlier return to pregnancy, a lower risk of intrauterine adhesions, and more effective evacuation of uterine contents. The study’s results, analysed by Hooker et al. [3] indicated that the occurrence of intrauterine adhesions after curettage and TCR was 30% and 13%, respectively. One of the pharmaceutical approaches to avoid performing curettage is the use of misoprostol tablets. The findings indicated that nearly 87% of patients can have successful expulsion, especially in patients with a thinner remaining volume. Prostaglandins and their analogs are widely used for inducing abortion. Misoprostol, as a prostaglandin E1 analog, is used extensively in early pregnancy termination and has proven advantageous due to its availability, ease of use, cost-effectiveness, convenient storage, and minimal side effects.
Sublingual and vaginal methods are common for administering misoprostol, each with distinct effectiveness, and the required dosage is based on pregnancy weeks and the type of abortion. In sublingual administration, the serum concentration peaks shortly, whereas the vaginal method has fewer side effects [11,12]. However, studies have raised questions about the effectiveness of misoprostol in patients diagnosed with RPOC.
For instance, a systematic review in 2016 failed to establish any significant association supporting the success rate of misoprostol use in the management of RPOC, particularly for preventing the need for surgical intervention [3]. Stewart et al. [13] estimated the successful expulsion rate in RPOC patients equal to 64.6%. This contrasts with the present study, where the success rate was 86.8%, which could be attributed to different diagnostic criteria. Medical treatment using misoprostol provides an alternative to surgery for patients unwilling to undergo surgical procedures. The findings of a cohort study by Chambers et al. [14] demonstrated a successful outcome in 93% of patients with RPOC based on clinical findings. Recently, several studies have reported the protective effects of delayed treatment in RPOC. However, regrettably, the term RPOC encompasses a broad spectrum, including various pregnancies in the past from early pregnancy to term pregnancy. Nevertheless, it remains unclear which patients may benefit more from conservative management [15,16].
The findings demonstrated that approximately 67% of patients initially considered for RPOC had successful expulsion with follow-up care. In patients without successful expulsion, only half required surgical intervention. Therefore, for patients with stable hemodynamic and a diagnosis of RPOC, a significant portion of them can be successfully managed without the need for surgery. Shi Tanaka et al. [6] studied 19 patients, including 14 with spontaneous abortion and five with induced abortion and indicated that all patients undergoing conservative management had successful expulsion, while 11 patients with RPOC required surgical treatment. Wada et al. [17] studied 44 patients diagnosed with RPOC and showed that 77% of patients could have successful expulsion with conservative management, without the need for specific treatment. The need for additional interventions in patients with haemorrhage and hypervascularity in RPOC was significantly higher. Kamaya et al. [18] also showed that 29% (51 out of 176 cases) of patients diagnosed with RPOC required surgical intervention, consistent with the results of the present study. A clinical trial conducted by Tzur et al. [19]. demonstrated that patients diagnosed with RPOC receiving misoprostol treatment had a treatment success rate of 61.8% (42 out of 68 cases), while the success rate with conservative management was 57.1% (36 out of 63 cases), with no statistically significant difference between the two groups (P=0.590). In a retrospective study by Takahashi et al. [15] on 59 patients with RPOC, 23 (39%) of them were successfully managed conservatively and RPOC was resolved. However, it is worth noting that the patient groups in their study were different from the present study, with a mix of preterm (7 cases) and term (40 cases), and only 12 cases (20%) had abortion. A The study had limitations due to its retrospective nature, including the inherent inaccuracies and incomplete data recorded in the patients’ medical records. Studies with larger sample sizes or clinical trials are recommended.
Conclusion
Treatment options for patients diagnosed with RPOC, based on clinical and sonographic findings in stable conditions, include conservative management, medical treatment using misoprostol, and surgical intervention. Surgical treatment in these patients involves curettage combined with dilation, which is the standard treatment for these patients. Although surgical treatment in these patients offers advantages such as complete and rapid removal of residual tissue, it can be associated with various complications, including anaesthesia-related risks, haemorrhage, and uterine adhesions. The findings indicated that with the use of medical and conservative management, it is possible to prevent surgery in at least 60% of the patients.
Acknowledgements
The study was funded by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences. The authors express their gratitude to Mr. Mohammad Faryadres for his assistance in drafting the article and for submitting it to this journal.
References
- Vitale SG, Parry JP, Carugno J, Cholkeri-Singh A, Della Corte L, et al. (2021) Surgical and reproductive outcomes after hysteroscopic removal of retained products of conception: a systematic review and meta-analysis. Journal of minimally invasive gynecology 28(2): 204-217.
- Abbasi S, Jamal A, Eslamian L, Marsousi V (2008) Role of clinical and ultrasound findings in the diagnosis of retained products of conception. Ultrasound Obstet Gynecol 32(5): 704-707.
- Hooker AB, Aydin H, Brölmann HA, Huirne JA (2016) Long-term complications and reproductive outcome after the management of retained products of conception: a systematic review. Fertil Steril 105(1): 156-164.e1-2.
- Groszmann YS, Healy Murphy AL, Benacerraf BR (2018) Diagnosis and management of patients with enhanced myometrial vascularity associated with retained products of conception. Ultrasound in Obstetrics & Gynecology 52(3): 396-399.
- Murtaza UI, Ortmann MJ, Mando-Vandrick J, Lee AS (2013) Management of first-trimester complications in the emergency department. Am J Health Syst Pharm 70(2): 99-111.
- Shitanaka S, Chigusa Y, Kawahara S, Kawasaki K, Mogami H, et al. (2020) Conservative management for retained products of conception after less than 22 weeks of gestation. J Obstet Gynaecol Res 46(10): 1982-1987.
- Namazi G, Haber HR, Tavcar J, Clark NV (2021) Minimally invasive management of retained products of conception and the adherent placenta. Curr Opin Obstet Gynecol 33(4): 311-316.
- Levinsohn-Tavor O, Sharon NZ, Feldman N, Svirsky R, Smorgick N, et al. 2022 Managing patients with suspected postpartum retained products of conception using a novel sonographic classification. Acta Radiol 63(3): 410-415.
- Morris JL, Winikoff B, Dabash R, Weeks A, Faundes A et al. (2017) FIGO’s updated recommendations for misoprostol used alone in gynecology and obstetrics 138(3): 363-366.
- Muffley PE, Stitely ML, Gherman RB (2002) Early intrauterine pregnancy failure: a randomized trial of medical versus surgical treatment. Am J Obstet Gynecol 187(2): 321-325.
- Kapamadzija A, Vukelić J, Bjelica A, Kopitović V (2010) [Medical abortion--modern method for termination of pregnancy]. Med Pregl 63(1-2): 63-67.
- Bettahar K, Pinton A, Boisramé T, Cavillon V, Wylomanski S, et al. (2016) [Medical induced abortion]. J Gynecol Obstet Biol Reprod (Paris) 45(10): 1490-514.
- Stewart KT, Lee JS, Pan K, Albert AY, Fisher S (2020) Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: a retrospective cohort study. Eur J Contracept Reprod Health Care 25(6): 474-479.
- Chambers DG, Mulligan EC (2009) Treatment of suction termination of pregnancy‐retained products with misoprostol markedly reduces the repeat operation rate. Australian and New Zealand Journal of Obstetrics and Gynaecology 49(5): 551-553.
- Takahashi H, Ohhashi M, Baba Y, Nagayama S, Ogoyama M, et al. (2019) Conservative management of retained products of conception in the normal placental position: A retrospective observational study. Eur J Obstet Gynecol Reprod Biol 240: 87-92.
- Grewal K, Al-Memar M, Fourie H, Stalder C, Timmerman D, et al. (2020) Natural history of pregnancy-related enhanced myometrial vascularity following miscarriage. Ultrasound Obstet Gynecol 55(5): 676-682.
- Wada Y, Takahashi H, Suzuki H, Ohashi M, Ogoyama M, et al. (2021) Expectant management of retained products of conception following abortion: A retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 260: 1-5.
- Kamaya A, Krishnarao PM, Nayak N, Jeffrey RB, Maturen KE (2016) Clinical and imaging predictors of management in retained products of conception. Abdom Radiol (NY) 41(12): 2429-2434.
- Tzur Y, Berkovitz-Shperling R, Goitein Inbar T, Bar-On S, Gil Y, et al. (2022) Expectant vs medical management for retained products of conception after medical termination of pregnancy: a randomized controlled study. Am J Obstet Gynecol 227(4): 599.e1-599.e9.






























