Increasing Community-Based Access to Safe Therapeutic and Post Abortion Care for Adolescent Girls and Young Women (AGYW) in Urban Slums of the Federal Capital Territory, Nigeria: Implication for Self Care. and Task Shifting
Eremutha Awasighe Francis1* and Okpetu Emmanuel2
1Women Friendly Initiative (WFI), Kuje Abuja, Nigeria
2Department of Primary Health Care, Kuje Area Council, Nigeria
Submission: June 23, 2023; Published:July 31, 2023
*Corresponding author: Eremutha Awasighe Francis, Women Friendly Initiative (WFI), Employment Area, Kuje Abuja, Nigeria, Email: winitiative@wfi.org.ng
How to cite this article: Eremutha Awasighe F, Okpetu E. Increasing Community-Based Access to Safe Therapeutic and Post Abortion Care for Adolescent Girls and Young Women (AGYW) in Urban Slums of the Federal Capital Territory, Nigeria: Implication for Self Care. and Task Shifting. Glob J Reprod Med. 2023; 10(3):8055779. DOI: 10.19080/GJORM.2023.10.555788.
Abstract
Adolescent girls and young women face significant sexual and reproductive health challenges in Nigeria with barriers limiting access to safe therapeutic abortion and post abortion care. The situation is more pathetic at the grassroots, including urban slums where reproductive health services are limited. A baseline survey of safe and post abortion care knowledge, attitudes and practices of adolescent girls and young women in female dominated vocational skills was conducted in 3 urban slums within the Federal Capital Territory of Nigeria. This was followed by an intensive training on modern contraceptives, effective administration of Misoprotol for safe therapeutic and post-abortion care, supply of Misoprostol and contraceptives. This report presents the estimates of key project indicators that were measured at baseline (2021) and endline (2022), providing a summary assessment of significant changes that occurred in knowledge and practice among the community health providers and adolescent girls and young adults targeted.
All respondents were exposed to family planning and safe abortion information and service as a result of the intervention. There was a significant increase in the knowledge and performance of the respondents in the provision of both family planning methods and the use of Misoprostol for safe therapeutic abortion and post abortion care. Utilization of both modern contraceptives and safe abortion services increased at all intervention sites over the duration of the intervention. The task shifting safe therapeutic and post-abortion intervention showed favourable outcomes over the short implementation timeframe. The evaluation demonstrated the potential for sustainability with more efforts and further intervention.
Keywords: Abortion care; Contraceptives; Misoprostol; Maternal mortality;
Key Message Safe therapeutic abortion with the use of Misoprostol has been shown to be more effective and non-invasive compared to surgical procedure. The survey interventions promoted community-based access to Misoprostol bringing services nearer to the clients in the comfort of their homes thereby reducing the occurrence of unsafe clandestine abortions.
Introduction
Compared to the general public, Adolescent Girls and Young Women (AGYW) aged 15-24 years, have a greater vulnerability to unsafe abortion occasioned by unmet need for family planning and unwanted pregnancies [1]. This is because they are far more likely to enter into sexual relationships and also more likely to delay marriage in order to complete school and become better prepared to join the labour force [2]. Globally, an estimated 121 million unintended pregnancies occur each year among women of reproductive age, and ~60% end in abortion [3]. Nigeria has one of the highest maternal mortality ratios in the world [4], although the government has acknowledged the problem and is committed to improving maternal health, evidence suggests that progress has been limited, and unsafe abortion remains a major contributor to maternal morbidity and mortality. In 2017, according to PMA2020 [5], the annual incidence of likely abortions in Nigeria was 41.8% per 1000 women aged 15-49 (nearly 1.8 million abortions). Literature reviews indicates that unsafe abortion complications accounts for 20%-40% of maternal deaths in Nigeria [6].
WHO defines unsafe abortion as a procedure for terminating an unintended pregnancy either by individuals without the necessary skills or in an environment that does not conform to minimum medical standards, or both [7]. In Nigeria abortion is restricted by law, hence, the utilization of unsafe abortion to terminate unwanted pregnancy has become necessary [8]. While contributing to maternal mortality, unsafe abortion results in an estimated 20,000 deaths of women in Nigeria yearly, with majority of the survivors having to live with serious complications including damage to vital organs and infertility (Ezegwui et al., 2013) [9]. In addition there is the huge burden on the health system as most cases of complications are admitted in the hospital, draining scarce human and material resources.
Globally, medical abortion (MA) has become an increasingly important method for people seeking to terminate a pregnancy [10] While mifepristone followed by misoprostol is the preferred MA regimen recommended by the WHO, misoprostol alone is recommended as a safe and effective alternative where mifepristone is not available [11]. Medical Abortion (MA) refers to early pregnancy termination using drugs. It is a nonsurgical method of abortion administered through the use of the pharmaceutical drugs, mifepristone and misoprostol, or misoprostol alone. Misoprostol is a WHO-approved drug for MA that is widely available in pharmacies in low- and middle-income countries (LMICs) as it has other indications including treatment of gastric ulcers and postpartum haemorrhage. Medical abortion (MA) has the potential to expand access to safe abortion services because this method is well-suited for the primary health care setting. Misoprostol is registered in Nigeria but its use in abortion was off-label. Though MA has the potential to expand access to safe services, availability of service providers is a necessary requirement to meeting women’s reproductive health needs.
Overall, the delivery of quality FP services across Nigeria depends on the skilled providers and human resource availability at both public and private points of care. Nigeria’s Human Resources for Health have being affected by factors ranging from shortage of manpower with attendant burnout, lack of adequate hazard allowance, outstanding Medical Residency Training Fund, etc.; leading to a devastating decline in number of especially skilled health workers attending to an increasing number of clients seeking for medical services. Based on the realization of severe health care worker shortage globally especially in sub-Sahara Africa, Nigeria inclusive, the World Health Organization (WHO) proposed task shifting to improve access to health care services [12]. Task shifting is the name given to a process whereby specific tasks are moved, where appropriate, to health care workers with shorter training and fewer qualifications. Task shifting is considered as a public health initiative that takes a comprehensive approach, with intentions to address the health care workforce requirement of all priority health programmes in the country. In addition, task shifting is among strategies for accelerating the progress towards achievements of the health-related SDGs. As such, the policy focuses on key priority areas such as family and reproductive health and maternal and child health services (RMNCH), as well as HIV, TB, malaria and other communicable and non-communicable diseases in essential health services package (FMOH, 2014) [13].
Regarding FP, task sharing is commonly practiced in the public health sector to community healthcare workers (15-16) but not implemented often in the private sector with CPs and PPMVs despite it being considered a high impact practice in FP [14]. As reported by Dawson et al. (2013) [15], shifting and sharing tasks may increase access to and availability of maternal and reproductive health (MRH) services without compromising performance or patient outcomes which may be cost-effective. Similarly, the task to be shifted is defined and described, and where funding is moved to the new individual assigned to the task in a deliberate manner. Thus, task shifting succeed with deliberate support for training, services restructuring, mentoring, supervision, and continuous support from existing health system structures [15,16]. Researches has demonstrated that strengthened collaborations and effective referral linkage between traditional and non-traditional health care providers such as birth attendants, community health workers and women artisan groups to facilitate distribution of contraceptives and abortion medications in the communities is a task-shifting option that could reduce unwanted pregnancy and the associated maternal morbidity and mortality from unsafe clandestine abortion [17].
Health Service provision in Nigeria can be either public or private entities but all primary health care (PHCs) facilities are funded by the government. The private sector also encompasses Private Patent Medicine Vendors (PPMVs) and Community Pharmacies (CPs). PPMVs are only allowed to stock condoms and to re-supply oral contraceptive pills, CPs can dispense pills and in some cases provide injectable while hospitals can offer a greater number of contraceptive methods [18]. A previous baseline study by Eremutha and Okpetu (2021) [19] explored the task shifting potentials of non health community based providers of comprehensive maternal health services in urban slums. The study demonstrated that major gaps exist in knowledge, attitude and practice of family planning and safe therapeutic abortion among out-of-school adolescent girls and young women in urban slums of the Federal Capital Territory of Nigeria. To ameliorate these gaps, the study recommended health education campaigns targeting young females engaged in out-of-school vocational skills through peer influence, community involvement and grass root seminars actively provided by government and NGO, has the potential to increase both the availability and quality of family planning delivery, abortion safety and general maternal health and well-being in Nigeria.
Following the baseline, a comprehensive training workshop on modern contraceptives and effective administration of Misoprotol for safe therapeutic and post-abortion care for selected community health providers and patent medicine vendors was conducted. The training provided an increase in the health providers’ knowledge on modern family planning methods, built their capacities on the proper dosage in the administration of Misoprostol for safe abortion and also changed their attitudes in the stigma attached to abortion. The intervention also included the provision of essential commodities in selected facilities to ensure that safe abortion services were available when the services are sought by the adolescent girls and young women within the communities.
This end line study therefore, is targeted at analysing post – intervention data and evaluate if interventions were adequate and achieving desired programme objectives; to establish the magnitude of impact of project intervention. Similarly, the survey evaluated the changes in knowledge about family planning and abortion-related issues, changes in abortion care-seeking, and service utilization as a result of this intervention. Specifically, this study is aimed at providing proof to the concept for designing cost effective interventions for community-based access to Family Planning and Therapeutic Safe & Post Abortion Care services among Adolescent Girls and Young Women (AGYW) in urban slums in Nigeria using the task shifting, task sharing model.
Methodology
The survey adopted both quantitative and qualitative descriptive research design, and was carried out in three districts of the Federal Capital Territory (FCT) of Nigeria namely Mpape, Kubwa and Nyanya as in the baseline survey. The data consisted of 200 Exit Interviewer-administered Questionnaire to clients extracted from the clinic data in the last one year; Key informant Interviews (KII) conducted with [20] trained health providers comprising of community nurse/midwives, community health workers and Private Patent Medicine Vendors (PPMV).
A total of 15 questions exit-interviewer, semi-structured questionnaire were administered to 200 clients extracted from participating clinic records. The questionnaires were divided into two sections; the first section generated information on the sociodemographic data of the respondents; the second section assessed respondents’ practice of family planning and safe therapeutic abortion services. Information about adolescent girls and young women who attended the project participating clinics/hospitals and used misoprostol in the last one year was extracted.
A 6- question KII guide on issues relating to reproductive health services including family planning and safe therapeutic abortion/ post-abortion care offered, significance of project interventions in service provision for the clinic in general, challenges/ limitations faced in service provision and recommendations for the sustainability of service provision. The KII guide contained an introduction of the researcher and full disclosure of the survey, ethical considerations as well as request for consent. All projecttrained health providers within the participating clinics/hospital were interviewed.
Information gathered from the questionnaire was cleaned and coded for data entry. It was then entered and analyzed using SPSS (Statistical Package for the Social Sciences) software version 17.0. The quantitative data were analyzed for frequency of occurrence. The information from the KIIs were transcribed and analyzed for themes and contents. Ethical approval was obtained from the Health Research Ethics Committee (HREC) of the Federal Ministry of Health. The research team ensured privacy during the interviews and discussions as well as in reporting of data. Consent was obtained from all participants by explaining the full extent of the survey and having them sign the consent form. Patient and Public Involvement statement: Participants were recruited during the baseline survey for voluntary participation in the intervention phase of the project. The training modules were informed and developed based on participants’ requests and suggestions during the baseline. Also, supplies of misoprotol and contraceptive commodities were distributed to participating clinics/outlets based on requested stock and re-stock.
Results
Socio-demographic Characteristics
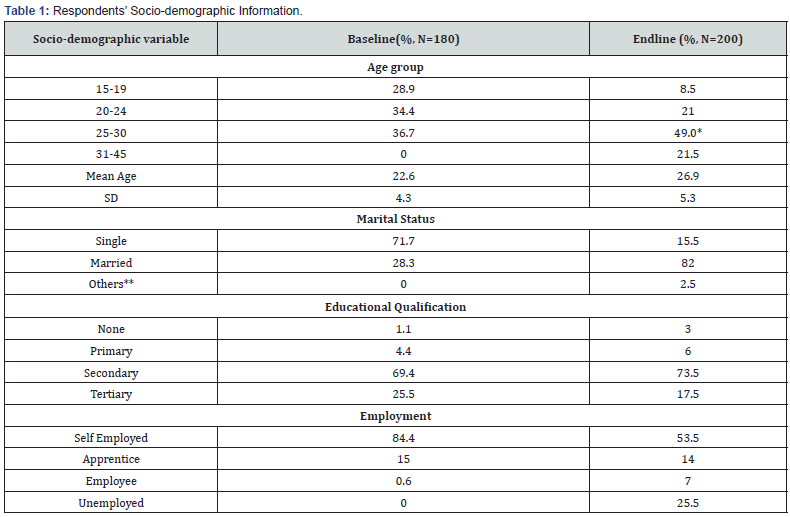
Age, marital status, educational qualification and vocational status of respondents were some of the key background variables collected from respondents at both baseline and endline. The endline survey identified more women in the age group (between 25-30 years) as well as more married women than the baseline as shown below in Table 1. Comparing the proportions from the baseline with the endline sample using a test of the difference between two proportions, the endline survey identified more women in the age group (between 25-30 years) as well as more married women than the baseline survey.
Knowledge and Attitude for Safe Abortion and Family Planning
Knowledge and attitudinal scores of the health providers were calculated for each respondent. Score for family planning was calculated for each respondent using a 10-point knowledge scale. Each correct answer had a score of 2, an incorrect answer or a no response had a score of 0 and the open-ended questions had a score of 4. The scores were then summed up to give a composite knowledge score for each respondent. The higher the score, the higher the knowledge and vice versa. Similarly, attitudinal score for family planning and safe abortion was calculated for each participant using a 10-point knowledge scale. Each correct answer had a score of 1, an incorrect answer or a no response had a score of 0. The scores were then summed up to give a composite attitudinal score for each respondent. The higher the score, the more positivethe attitude and vice versa (Table 2).
* Two-sample test of proportions, significance level p < 0.05
**Separated, divorced or widowed
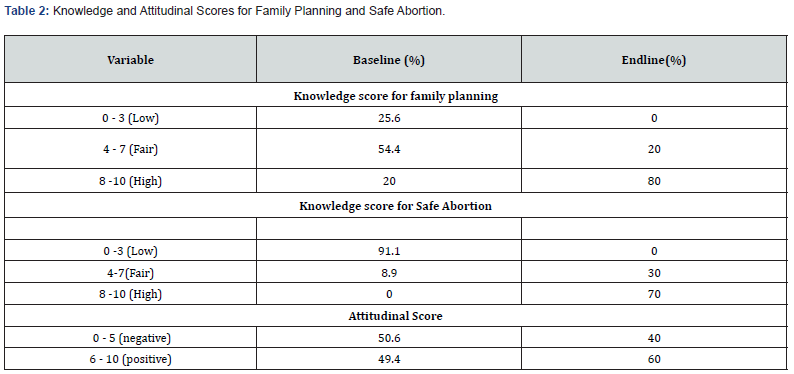
At endline, participant’s attitudes toward abortion changed, nearly all participants in the intervention who were interviewed agreed that they should provide safe abortion information to women who request it. Nearly all agreed that healthcare workers deserve respect for providing abortion care and that abortion should be legally available in the country for any woman who needs it (80%). Among those interviewed at endline, 70% reported discussing safe abortion with colleagues since their training and 84% had spoken to a friend or relative about the risks of having an unsafe abortion.
Contraceptive Uptake
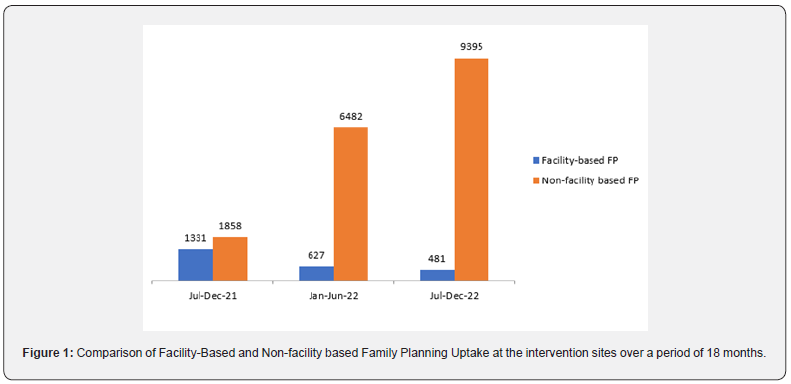
Modern contraceptive use has increased significantly since the baseline survey. Pill use rose slightly from 2.2% to 3.5%. Use of injectables also increased from 0.6% to 5.0% during this period. LARCs use increased from 1.7% in the baseline to 10.0% at the endline; the increase was much higher for implants compared to IUDs. In the endline survey, 7.5% of the women were using implants, representing a four-fold increase from the 1.7% recorded at baseline. Also the contraceptive method with the highest uptake at the baseline was condom while the use of implants had the highest increase at the endline survey. This reflects the access to implants made possible at community level that the project supported Figure 1 also shows steady increase in Family Planning Uptake at non-facility based sites of intervention and a decline at facility-based intervention sites. The modern contraceptive uptake rate among currently married women increased significantly from 6.1% to 17.0% as shown in Table 3,4.
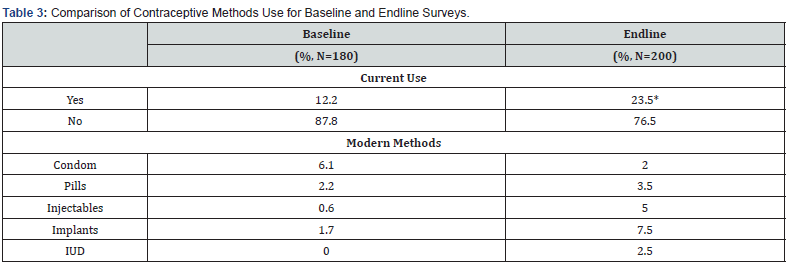
*significance level p < 0.05
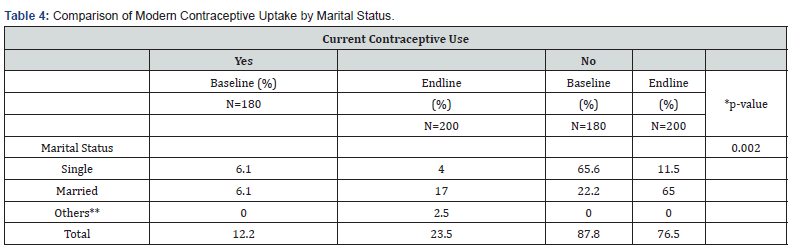
*Chi-square test, significance level p < 0.05
**Separated, divorced or widowed
Post-Abortion Contraceptive Use
Respondents’ records showed significant change in the uptake of contraception after safe abortion. The reasons according to the providers included mandatory supply of condoms plus at least one of three other methods of family planning commodities at the end of each procedure. Records showed that 99.9% of clients received post procedure contraception. However, there was poor revisit for re-supply to ascertain continuity.
Misoprostol Use Use
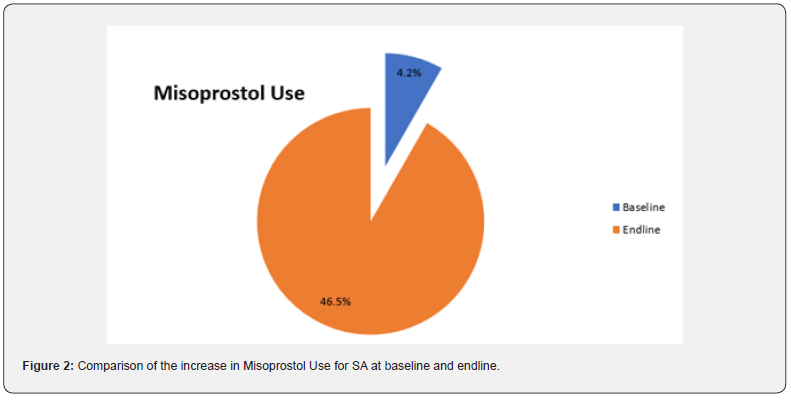
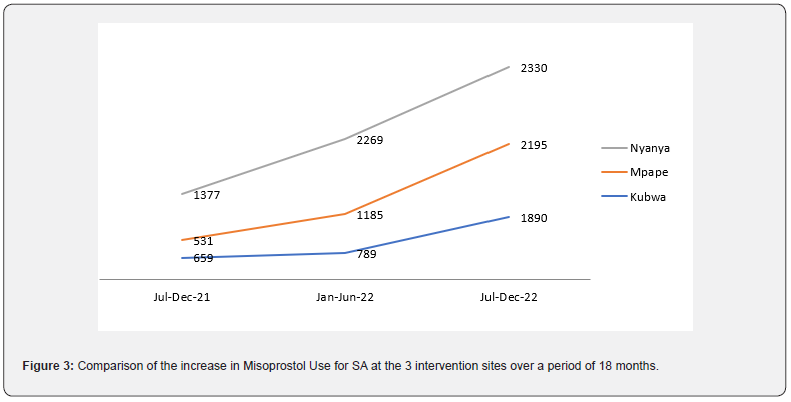
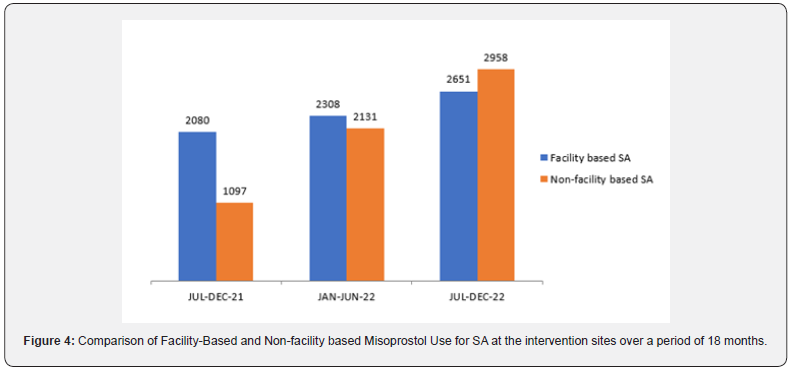
Figure 2 shows the increase in induce safe therapeutic abortion cases using misoprotol following the onset of the intervention at the endline. Figure 3 shows a dramatic rise in the uterine evacuation caseloads following the onset of intervention in a period of 18 months at the three intervention sites. Similarly, Figure 4 shows a comparison of SA request at facility and non facility based intervention sites within the 18 months period.
Results from Interviews
Sexual and Reproductive Health Services Provision in Communities
Post-abortion care and sterilization method of family planning were for referral in public health facilities as at baseline. However at endline, project participating private clinics/hospitals on the other hand can provide such services. An informant reported that <‘we attend to cases of complicated self induced abortions, we first do scan to know if the baby is still there and if not we administer misoprostol and then do manual evacuation of the retained product. We hardly do referral now’. Apart from the on site safe abortion services provided by private health facilities, an informant added that the health providers monitored their clients through follow up and counselling on contraceptives to prevent future occurrence of unwanted pregnancy. Also, informants from pharmacy and patient medicine store reported that the service provided is mainly counselling on contraception and safe abortion using misoprostol, sale of products and commodities as well as referral linkage to higher level providers. “I only counsel on family planning and medication abortion and sell products and commodities. “If they require the more services, I refer them to the nearest provider in our partnership map”.
Family Planning Method Mix in Project Communities
Contraceptive method mix was provided freely in the public health facilities. However at the endline, there were some private clinics offering almost all of the methods ranging from condom, oral pills, injectables, implants to IUDs except sterilization making it easier to access post procedure contraceptives from private clinics. The contraceptive method with the highest uptake at endline was the injectables (40.0%) while implants were a close second at 20.0%. This was the same at the baseline survey. The reason for the high uptake rate for injectables as reported by the respondents at the endline was consistent with the baseline; it was so because it is short term and does not require daily dosage as oral pills which could easily be forgotten thereby losing its efficacy.
Safe Therapeutic and Post Abortion Care in Participating Clinics/Hospitals
Following the baseline study, intervention approach which included capacity building, supply of Misoprostol and contraceptives as well as Information, Education and Communication (IEC) Materials were provided in the participating clinics/hospitals. At baseline, majority of the participants reported request for safe abortion among clients with unwanted pregnancy but were refused service. However at endline, the informants from private clinics reported the use of misoprostol for SA.
Discussion
Findings from this study has shown that targeted trainings of community health providers, supply of essential commodities, mentoring and monitoring on safe therapeutic abortion and modern contraceptives has the capacity to increase knowledge of these services and its practice in the targeted urban slums. Results from this study were consistent with other studies in Nigeria that found positive impact of training on providers’ knowledge [18]. Table 1 confirms earlier studies by Eremutha and Gabriel [20] on recommendations for improving SRH uptake for young people in health facilities within communities to include Community-based facilitated education sessions and Multi-component and multisectoral approaches as potential indicators for increasing youth access to SRH.
Table 2 demonstrates that provision of capacity building in addition to IEC materials on contraceptive types/counselling and monitoring/mentoring of service providers has the capacity to improve the knowledge of providers on modern contraceptive and safe abortion as evident from the endline data. Similarly, involvement of AGYW in female focused vocations in the design of the intervention and their training as peer influencers as reported in the survey, improved family planning sales among non-facility based providers (PPMV’s) as seen in Figure 1 within targeted slums. AGYW through the provision of peer to peer counseling encouraged and made referrals for the uptake of contraceptive options in the different slums. This further revealed that task shifting and sharing can help in expanding access to essential health care services to meet the set SDG targets. This finding is in line with the goal statement in the Nigeria Task shifting and Task Sharing (TSTS) policy documents (2014) [21].
Figure 2 and 3 demonstrates a sharp increase in self induced medication abortion following capacity building of facility based providers in participating clinics and hospitals. These findings suggest a relatively high level of autonomy for abortion care seeking among women and indicate the important role that community health care providers play as trusted sources of information and providers of MA as a good harm reduction method in the avoidance of clandestine and unsafe abortion in undeserved settings as slums and restrictive environment as Nigeria. In other studies have also concluded using misoprostol for abortion is a good harm-reduction method in restrictive settings [22-23]. Similarly, Figures 4, 5 and 6 indicate the important role that PPMVs play as trusted sources of information and providers of MA in undeserved slums. However, the appropriateness of the drug prescriptions and the quality of information provided to women by PPMVs as documented in other studies [24], were not evaluated by this study.
Analysis of the qualitative data indicates the benefits of capacity building, monitoring and the distribution of IEC materials were significantly associated with achievement of the four outcome measures reported in this survey. These findings are consistent with other studies that found improved outcomes with health worker supervision, audit and feedback, components that were part of the post-training support offered to the providers [25]. Furthermore, there is a remarkable improvement in Knowledge and attitudinal scores for the provision of family planning and therapeutic safe abortion post training (endline) compared to pre-intervention (baseline) study. Results from this study are consistent with other studies that found positive impact of training on providers’ knowledge [26,27]. This finding is promising for the strategy of task shifting task sharing in undeserved settings by expanding the role of non - traditional health workers in FP and MA service delivery in view of the major shortage of skilled providers for delivering these services.
WHO recommends that professionals such as health care workers must learn to separate their personal beliefs and values from their professional practices and treat all women equally and with empathy, regardless of their reproductive behaviours and decisions [17]. Participants in this study has demonstrated same approach in the provision of sexual and reproductive health services post intervention in line with the WHO (2012) recommendation.
Conclusion
This study has demonstrated that community healthcare providers can be trained to offer FP and safe therapeutic abortion services largely as a harm reduction efforts towards lowering incidences of unsafe and clandestine abortion among AGYW and most importantly as a task shifting and task sharing practice towards meeting the successful implementation of the policy. Their knowledge can be supported through mentoring/ monitoring, IEC materials and commodity support, for the provision of accurate information and quality services. Similarly, there is need for intense advocacy for the lifting of the ban on free access to safe therapeutic abortion in the country, training of more health providers especially at the community levels and regular supply and prioritization of the essential commodities to especially private ensure the quality provision of safe abortion services.
References
- United Nations, Department of Economic and Social Affairs. World Family Planning; New York: UN. 2017.
- Singh S, Remez L, Sedgh G, Kwok L, Onda T (2017) Abortion worldwide 2017: uneven Progress and unequal access. New York: Guttmacher Institute.
- Bearak J, Popinchalk A, Ganatra B, Moller A-B, Tunçalp Ö, et al. (2020) Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990-2019. Lancet Global Health 8(9): e1152-1161.
- WHO et al. (2014) Trends in Maternal Mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division, Geneva.
- PMA2020 Abortion Survey Result: Nigeria. April-May 2018.
- FE Okonofua, E Odimegwu, H Ajabor (1999) Assessing the prevalence and determinants of unwanted pregnancy and induced abortion in Nigeria. Stud Family Plan 30(1): 67-77.
- Unsafe abortion (2007) Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003. Fifth edition. Geneva, World Health Organization.
- Unsafe Abortion (2005) Facts and Figures. Population Reference Bureau.
- Ezegwui HU, Onoh RC, Ikeako LC, Onyebuchi A, Umeorah J, et al. (2013) Investigating Maternal Mortality in a Public Teaching Hospital, Abakaliki, Ebonyi State, Nigeria. Ann Med Health Sci Res 3(1): 75-80.
- Singh S, Remez L, Sedgh G (2018) Abortion worldwide 2017: uneven progress and unequal access. Guttmacher Institute.
- World Health Organization (2018) Medical management of abortion. Geneva.
- World Health Organization (2008) Task shifting: Global recommendations and guidelines. Geneva.
- Federal Ministry of Health (2014) Task-shifting and task sharing policy for essential health care services in Nigeria.
- Stanback J, Spieler J, Shah I, Finger WR (2010) Community-based health workers can safely and effectively administer injectable contraceptives: conclusions from a technical consultation. Journal of Contraception 81(3): 181-184.
- Dawson A J, Buchan J, Duffield C, Homer CSE, Wijewardena K (2014) Task shifting and sharing in maternal and reproductive health in low income countries: a narrative synthesis of current evidence Journal of Health Policy and Planning 29(3): 396-408.
- Emdin C, Millson P (2012) A systematic review evaluating the impact of task shifting on access to antiretroviral therapy in Sub-Saharan Africa. Afr Health Sci 12(3): 318-324.
- World Health Organization (2012) Safe Abortion: Technical and Policy Guidance for Health Systems. Second ed., Geneva.
- Ujuju C, Adebayo SB, Anyanti J, Oluigbo O, Muhammad F (2014) An assessment of the quality of advice provided by patent medicine vendors to users of oral contraceptive pills in urban Nigeria. Journal of Multidisciplinary Healthcare 7: 163-171.
- Eremutha, Awasighe Francis, Emmanuel Okpetu (2022) Exploring the Task Shifting Potentials of Non-Health Community Based Providers of Comprehensive Maternal Health Services in Urban Slums in Federal Capital Territory, Nigeria: Community Survey. IOSR Journal of Humanities and Social Science (IOSR-JHSS) 27(01): 37-47.
- Eremutha, Francis, Gabriel, Veronica Chizoba (2018) Community Survey on Barriers Limiting Youth Access to Reproductive Health Services by Primary Health Care (PHC) Facilities in Nigeria. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) 17(11): 35-41.
- Federal Ministry of Health (2014) Task-shifting and task sharing policy for essential health care services in Nigeria.
- Hyman, Alyson, Kelly Blanchard, Francine Coeytaux, Daniel Grossman, Alexandra Teixeira (2013) Misoprostol in Women's Hands: A Harm Reduction Strategy for Unsafe Abortion. Contraception 87(2): 128-130.
- Harvey Phil (2015) Medical Abortion: The Hidden Revolution. Journal of Family Planning and Reproductive Health Care 41(3): 193-196.
- Katharine Footman, Katherine Keenan, Kate Reiss, Barbara Reichwein, Pritha Biswas, et al. (2018) Medical abortion provision by pharmacies and drug sellers in low- and middle-income countries: a systematic review. Stud Fam Plann 49(1): 57-70.
- Alexander K Rowe, Don de Savigny, Claudio F Lanata, Cesar G Victora (2005) How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet 366(9490): 1026-1035.
- Rama Rao S and Mohanam R (2003) The quality of family planning programs: concepts, measurements, interventions, and effects. Studies in Family Planning 34(4): 227-248.
- Costello M, M Lacuesta, S Rama Rao, A Jain (2001) A client-centered approach to family planning: the Davao project, Studies in Family Planning. 32(4): 302-314.






























