Influence of Social Isolation on Quality of Life and Symptoms of Hormonal Deficit in Clamatorial and Menopause Women: A Comparison Pre, During and After Social Restriction Due Covid-19
Camila Oliveira Serra1, Paula Mara Gomes Leite1, Lucas Veras3, Andréa Beatriz Bezerra3, Ariane Flores2, Giorjines Fernando Boppre2, Ana Verena Calmon Almeida2, Walderi Monteiro Silva Junior3, Jader Pereira de Farias Neto3 and Leonardo Yung dos Santos Maciel1,3*
1Postgraduate Nursing program, Federal University of Sergipe, Brazil
2Research Centre in Physical Activity, Health, and Leisure (CIAFEL), Faculty of Sport, University of Porto, Portugal
3Department of Physical Therapy, Federal University of Sergipe, Brazil
Submission: May 15, 2023; Published:June 22, 2023
*Corresponding author: Leonardo Yung dos Santos Maciel, Department of Physical Therapy, Federal University of Sergipe, Brazil, Email: yung_maciel@hotmail.com
How to cite this article: Camila Oliveira S, Paula Mara Gomes L, Lucas V, Andréa Beatriz B, Ariane F, et al. Influence of Social Isolation on Quality of Life and Symptoms of Hormonal Deficit in Clamatorial and Menopause Women: A Comparison Pre, During and After Social Restriction Due Covid-19. Glob J Reprod Med. 2023; 10(2):8055779. DOI: 10.19080/GJORM.2023.10.555783.
Abstract
Introduction: A major concern reinforced by the COVID-19 pandemic was the quality of life of women who experienced social isolation, with the drastic reduction in this public’s contact with health systems, the comprehensiveness and continuity of care were impaired, mainly for those who were in the climacteric and menopause period.
Objective: To analyse the influence of social restriction caused by the COVID-19 pandemic, on quality of life and climacteric and menopause symptoms Before Social Isolation, During Social Isolation and Post Social Isolation.
Method: This is a cross-sectional study. Data collection was carried out from January 2020 to December 2022. The Women’s Health Questionnaire and the Menopause Rating Scale and a semi-structured interview script were used to assess climacteric symptoms and quality of life. for sociodemographic and clinical information.
Results: The sample consisted of 406 women, divided into three groups: Before Social Isolation (n=62), During Social Isolation (n=282) and Post Social Isolation (n=62). Age, race and level of education showed insignificant statistical difference between groups (p<0.005). In the Menopause Rating Scale scores, only the somatic symptoms domain showed relevant differences (p=0.005), as well as the Women’s Health Questionnaire sexual function domain (p=0.004).
Conclusion: The social isolation caused by the COVID-19 pandemic did not affect most of the self-reported symptoms, quality of life and self-care attitudes of the analyzed women.
Keywords: Climacteric; COVID-19; Menopause; Self-care; Indicators of quality of life
Abbreviations: ANOVA: Analysis of Variance; PNAISM: National Policy for Integral Attention to Women’s Health; BSI: Before Social Isolation DSI: During Social Isolation; PSI: Post Social Isolation; CEP/UFS: Ethics Committee of the Federal University of Sergipe; ICT: Informed Consent Term; MRS: Menopause Rating Scale; WHQ: Women’s Health Questionnaire
Introduction
During the SARS-COV-2 (COVID-19) pandemic, an increase in social inequality was observed, which mainly affected vulnerable populations, especially about access to and provision of health services. In this sense, a major concern that the pandemic reinforces is about the quality of life of women who have experienced social isolation, especially those who are in the climacteric and menopause period [1-3].
Notably, the offer of health care for women in the nonreproductive phase is incipient in Brazil, historically the identification of this gap only occurred in 2002, with the implementation of actions aimed at this public from the year 2004, with the creation of the National Policy for Integral Attention to Women’s Health (PNAISM). The update of this policy only occurred thirteen years later, in 2017, with its application, exclusionary and medicalizing forms of care that understood women exclusively in their reproductive role were overcome [4].
This deficiency in the health system reflects how women in the climacteric and menopause period were little noticed by society and how fragile the assistance aimed at them can still be. With the establishment of the social restriction brought about by the new corona virus, fragments of an old scenario once again permeated the assistance provided, with the drastic reduction of this public’s contact with the health systems, the comprehensiveness and continuity of care were impaired [5-7]. The term climacteric comes from the Greek Kilometer and is characterized as a transitional period between the reproductive and non-reproductive phases of a woman’s life. Menopause is the motto of this phase, representing the last menstrual cycle, being identified only after one year of amenorrhea, which usually happens around 48 to 50 years of age. Many women go through these transformations without complaints or need for interventions, while others experience a variety of symptoms that vary mainly in intensity. In both cases, comprehensive care is required aimed at promoting health and preventing harm [6].
Women with symptoms related to the climacteric and menopause, such as hot flashes, irritability and night sweats were evaluated and half of them reported symptoms of moderate intensity, and approximately 20 to 30% indicated them as of severe intensity [8]. In addition, in this period surrounded by hormonal changes, the female quality of life can be negatively affected, which often predicts an increase in self-care actions, such as the search for medical follow-up and the use of medication to relieve symptoms [9,10]. The term quality of life can be defined as the individual’s perception of their position in the cultural context and in the value system in which they live, however, with regard to the biological face, each woman experiences the climacteric according to her uniqueness. A study carried out with 646 Afro-Colombian women states that the levels of quality of life in menopausal women is closely associated with their symptomatology [8,11].
Approximately one billion women experience these symptoms worldwide and it is expected that by the year 2050 this number will increase by approximately 236 million women [10]. Despite being a physiological process, climacteric symptoms can be influenced by social, cultural and economic factors to which women are subjected [10,11]. Due to the stereotype inherited from the biomedical model, the negative perception that associates climacteric and menopause with aging and loss of value is still common in our society [12].
The non-reproductive phase is an important and inevitable period in women’s lives and should be seen as a natural and physiological process, and not as a disease. After menopause, women still have a third of their lives ahead of them, which can and should be lived in a healthy and productive way. However, most women are unaware of alternative measures to reduce symptoms and prevent injuries. Faced with the limitation of conventional treatments and the side effects that often do not outweigh the riskbenefit, it becomes a challenge for health services to incorporate complementary and safe techniques to provide a better quality of life for this public, especially during the COVID-19 pandemic [6,13].
This study is justified by the impact of the pandemic on the health system. Its realization was motivated by the researcher’s questioning about the impact of social restriction on the way women in the non-reproductive phase deal with the signs and symptoms of this period during isolation. Thus, the objective of the present study was to analyze the influence of social restriction caused by the COVID-19 pandemic, on quality of life and climacteric and menopause symptoms Before Social Isolation (BSI), During Social Isolation (DSI) and Post Social Isolation (PSI). It is intended, therefore, to contribute to a better understanding of the effects of social isolation on women in the post-reproductive phase, in addition to encouraging the implementation of measures that increasingly encourage their self-care.
Materials and Methods
Study design and participants
This is a cross-sectional study, carried out between January 2020 and December 2022. Data collection took place in three evaluation moments, forming three study groups: BSI Group, composed of 62 women who were interviewed in person from January to March 2020 by the researcher at Basic Health Units in the city of Aracaju, Brazil; The DSI group, made up of 282 women, residing in different regions of Brazil, invited to participate in the survey through an electronic form between June and September 2020, and the PSI group, made up of 62 women, were invited to participate in this survey in the period from June to December 2022, in the same way as the DSI group. The entire sample consisted of 406 women and had its sample based on the work of Leyte et al. [13].
Ethical aspects
This study was carried out in accordance with the principles of the Helsinki Declaration and was submitted to the Research Ethics Committee of the Federal University of Sergipe (CEP/UFS), via Plataforma Brazil. And the collection was carried out only after approval by the referred committee, with Certificate of Presentation for Ethical Assessment (CAAE): 16299419.7.0000.5546 and opinion: 4.023.073. In order to participate in this investigation, the sample had to present the inclusion criteria, as well as the consent for the research confirmed by the Informed Consent Term (ICT).
Inclusion and exclusion criteria
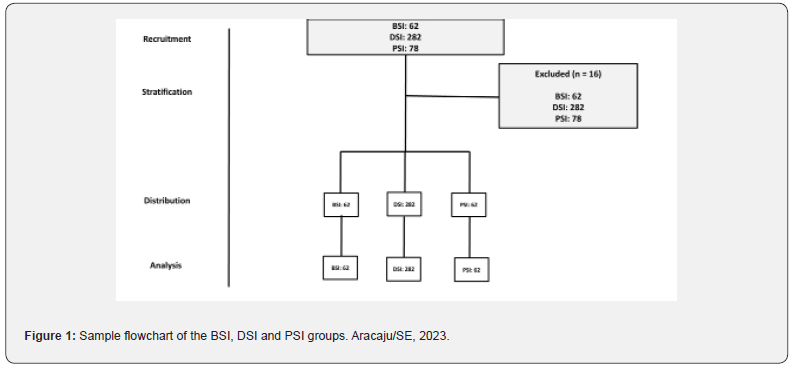
Inclusion criteria included women between 40 and 65 years old, with menstrual irregularity in the last 12 months or a maximum menstrual period of two times in the last 12 months; affected by any of the following symptoms - hot flashes (at least three episodes per day), diaphoresis, insomnia, migraine, irritability, vaginal dryness and dyspareunia. Exclusion criteria were inability to respond to the interview for any reason, such as illness and schedule incompatibility; lack of access to the Internet and inability to use the means of accessing the research link. For women who did not meet the inclusion criteria or who did not accept to participate in the research, a thank you was issued, and, at this moment, the questionnaire/interview was closed. Questionnaires with incomplete and/or duplicated information were excluded and the cases in which participants answered the questionnaire more than once, the first complete answer was considered valid, as shown in figure 1.
Data collection instruments
For data collection, a semi-structured interview script developed by the authors was used, divided into three sections, covering information on: (i) age (at the time of the interview, in complete years) and marital status (with or without a partner); (ii) education (as reported by the woman and according to the classification of Criterion Brazil (2019) and (iii) ethnicity/ race (self-declared) defined as white, brown, black, yellow or indigenous, and the clinical aspects described in the criteria of inclusion and exclusion. In addition, the Menopause Rating Scale (MRS) and the Women’s Health Questionnaire (WHQ), in the translated and validated versions for Brazilian Portuguese, were applied to measure health-related quality of life and the degree of climacteric and menopause symptoms. reported by the woman. Both instruments are recommended and used in studies with the same purposes as this study, to establish consistent parameters for the analysis of results [14-16].
The MRS is approached in eleven questions, related to climacteric symptoms and complaints, and composed in the following three domains of symptoms: (i) vegetative soma to, shortness of breath, diaphoresis, hot flashes, cardiac discomfort, sleep disorders and muscle problems and joints; (ii) psychological, including depressed mood, irritability, anxiety, physical and mental exhaustion and (iii) urinary tract symptoms, such as bladder problems, sexual problems and vaginal dryness. Each symptom is associated with a severity score, ranging from zero to four points (0, absent; 1, mild; 2, moderate; 3, severe; 4, very severe). Consequently, the total MRS score is obtained by the total scores of each domain, the higher it is, the more severe the symptoms are and the worse the quality of life. The maximum score is 44 points, and the general intensity of the reported climacteric symptoms can be categorized according to the severity of the climacteric symptoms into: (i) absent or occasional (0-4 points); (ii) mild (5-8 points); (iii) moderate symptomatology (9-16 points) or (iv) severe (≥ 17 points) [16].
The WHQ aims to assess nine domains related to physical and emotional health through 36 question items where participants marked the symptom presented: (i) 1 (yes, definitely); (ii) 2 (yes, sometimes); (iii) 3 (no, rarely) and (iv) 4 (not at all). In addition, the questions included an open-ended form in which women with symptoms could describe what they did to relieve them. The questionnaire domains reflect a relatively independent disaggregation of symptoms and are: (i) depressed mood; (ii) somatic symptoms; (iii) anxiety/fears; (iv) vasomotor symptoms; (v) sleep problems; (vi) sexual behavior; (vii) menstrual symptoms; (viii) memory/concentration and (ix) the “attractiveness” scale. The memory/concentration subscale assesses subjective memory, and the sexual subscale includes items related to vaginal dryness (causing sexual discomfort), sexual interest, and sexual satisfaction. Items referring to vaginal dryness and satisfaction were framed in the context of a current sexual relationship, so women who were not sexually active could skip and consequently omit the item. WHQ is scored on a fourpoint scale (1=yes definitely, 2=yes sometimes 3=no, not really, 4=no, not at all), these are reduced to binary options (0 - no /1 - yes) and subscale items are divided by the number of items in each domain. Higher scores represent more suffering and dysfunction.
Statistical analysis
Comparisons of socioeconomic variables between the groups assessed before, during and after the pandemic were performed using analysis of variance (ANOVA) for continuous variables and the chi- square test for categorical variables. To assess the effect of the time of assessment (before, during and after the pandemic) on the scores of each domain of the applied questionnaires, analysis of covariance (ANCOVA) was used. In these models, scores were defined as the response variable and the time of assessment as the explanatory variable. The covariates included in the model were those that presented statistically significant differences between the evaluation moments. Statistical analyzes were performed using the statistical software R (version 4.2.1, R Foundation for Statistical Computing, Vienna, Austria). The statistical significance value was defined as α = 0.05.
Results
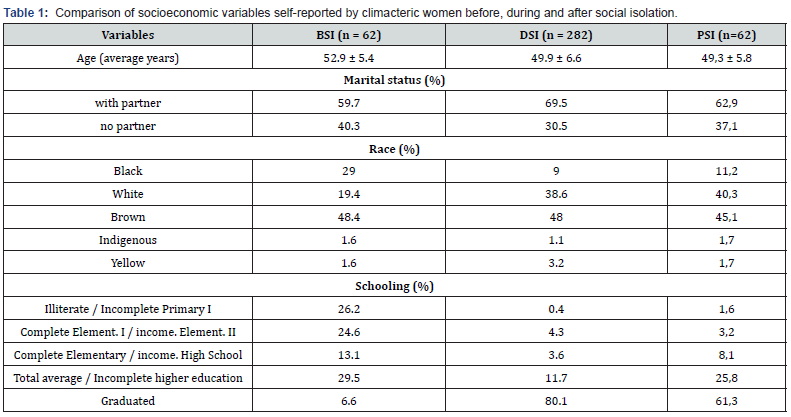
Four hundred and six women participated in the research, being divided into the BSI (n=62), DSI (n=282) and PSI (n=62) groups. After analyzing the self-reported socioeconomic variables, a mean age of 50.7 years was observed between the groups, a predominance of the self-declared brown race and a higher level of education in the DIS and PIS groups, these variables showed statistically significant differences (p <0.005). As explained in table 1.
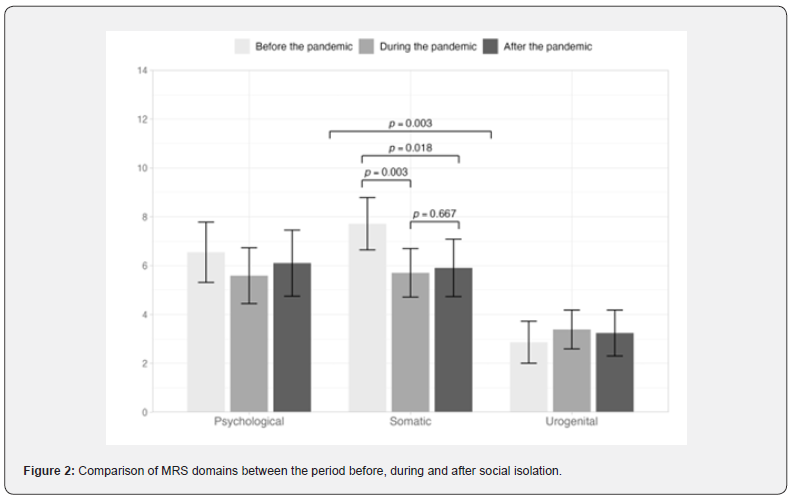
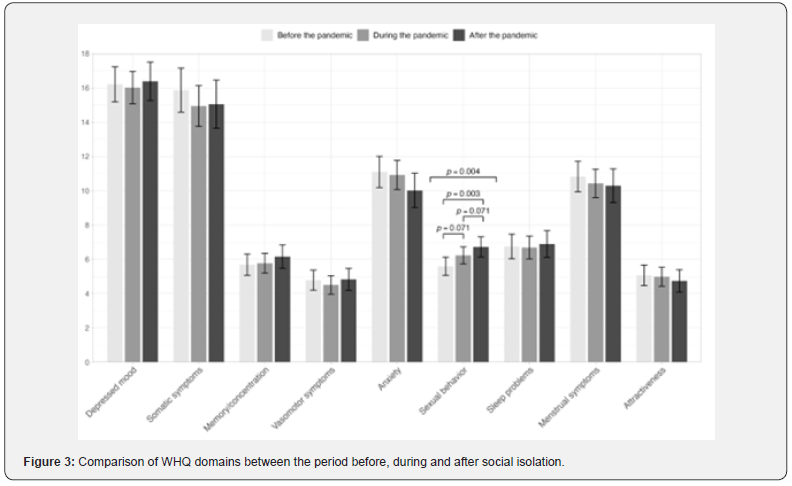
In the MRS scores, the only domain that showed a significant difference was somatic symptoms (p = 0.003). This difference occurred between the BSI and DSI (p = 0.003) and BSI and PSI (p = 0.018) periods, as observed in figure 2. There was no significant difference between the symptoms observed in the periods during and after social isolation in this domain (p=0.667). Regarding the domains referring to psychological and urogenital complaints, no significant differences were found (p > 0.005) in any of the analyzed periods. In figure 3 we can observe the WHQ scale scores and in them we highlight the sexual function domain, as being the only one to present a significant difference between the groups (p = 0.004). After statistical treatment, there was a difference between the BSI and PSI groups (p = 0.003), while in the comparison between the BSI and DSI (p = 0.071) and DSI and PSI (p = 0.071) groups, there was no significant difference.
Discussion
The climacteric is a period of strong impact on women’s quality of life, the symptomatology, and social stigmas regarding this phase of life can have repercussions on women’s self-care, especially considering the changes faced during the COVID-19 pandemic. The aim of this study was to analyze and compare climacteric and menopause symptoms, quality of life indices and self-care attitudes before, during and after social isolation. It was observed that the somatic symptoms were lower in the PIS period and the others were similar, with a tendency towards a decrease in psychological symptoms. Quality of life indices and self-care attitudes were similar before, during and after isolation. Age was not shown to be an indicator of climacteric and menopause symptoms in any of the evaluated groups, as has been demonstrated by other authors [17,18].
During the analysis of the MRS scale domains, it was possible to conclude that somatic symptoms (shortness of breath, diaphoresis, hot flashes, heart discomfort, sleep disturbances, muscle and joint problems) appeared in smaller numbers with the end of social restriction, if compared the women evaluated in the BSI and PSI periods. In part, this data may be related to the greater amount of information available regarding the prevention and ways of controlling the COVID-19 pandemic, which may have led to lower rates of stress among the women studied.
This lower index is also related to the trend towards a decrease in psychological symptoms in the PSI period compared to the BSI period. A Serbian study carried out with women in the climacteric and menopause period, also using the MRS scale, found that social isolation is a factor that worsens psychological symptoms [17]. A relevant statistical difference was also demonstrated regarding the improvement in symptoms of anxiety and depression in the post-pandemic period [18]. There was a trend towards a greater number of complaints belonging to the urogenital domain during social isolation, this increase is in line with a multicenter study carried out with 2500 women during the pandemic in Spain, in which 74.3% of them had some gynecological-related symptom. urological [19]. Still in corroboration, the studies [20], also found high levels of symptoms related to the urological system in postclimacteric women.
Regarding the data analyzed from the WHQ, a slight increase in sleep problems was observed in the PSI period, which may be related to the return-to-work activities such as work, study, among others, leading to a greater burden of stress [2]. Other Brazilian studies using the WHQ instrument also demonstrated a greater predominance of somatic symptoms and sleep disturbances [4,15,21]. Sleep disorders suffered from the increased frequency of undertreatment and its consequent worsening during the COVID-19 pandemic, thus requiring the application of preventive measures, identification of conditioning factors and active listening [21]. According to [22] the high rate of poor sleep quality is a factor of great impact on the worsening of other climacteric and menopause symptoms, including sexual problems.
Hormonal decline is not always the main cause of sexual dysfunction, sometimes it already exists and only in this period of life does the exacerbation of symptoms make the woman relate them to the climacteric. Coinciding with this, we observed many urogenital symptoms during social isolation, which may have been caused by the greater frequency of sexual intercourse, due to the longer period of time in contact with the partner, causing symptoms related to performance in the gender are in evidence [1,23]. The population studied during the DSI period also showed the highest rates of marital relationships, which reinforces this idea [22].
In corroboration, a survey carried out with 2661 Finnish women showed that sexual dysfunction during the climacteric presents higher levels in women aged close to 46 years, coinciding with what was observed in the DSI group in this study. However, other studies claim that the greater the sexual activity, the lower the intensity of climacteric symptoms and the greater the quality of life [4,15,21]. In addition to sexual symptoms, the urogenital domain also addresses urinary problems, a Turkish study carried out with 256 climacteric women showed that one in every two women evaluated presented symptoms of urinary incontinence [23]. The domain related to depressive symptoms of the WHQ scale remained stable during the analyzed periods, showing a trend towards an increase in the number of complaints after the end of social isolation. In contrast to this, studies point out that the social restriction brought about by the COVID-19 pandemic increased the rates of depressive mood, with age as an aggravating factor for psychological illnesses in a pandemic context [24-26].
Adherence to remote work and reconciling this with changes in daily routine are potential factors for worsening mental health and reducing self-care tools [27]. After analysis during the restriction period, climacteric women in the southwest of the United States found an increase in psychological and somatic symptoms correlated with their lower purchasing power [28]. Other international studies that also used the WHQ point out that depressed mood is among the most affected domains [7,28]. It is likely that the high levels of inequality and marginalization suffered by women who occupy the lowest social strata, affect these symptoms, thus making it even more difficult to face them, given the bidirectional relationship between social isolation and the emergence of psychological pathologies [21,29].
Social isolation aggravated the burden already faced by the female public, symptoms such as memory loss, low concentration and/or forgetfulness became increasing complaints, as observed in the present study, when comparing the BSI and DSI groups. The culprits for this increasingly stressful scenario should not be restricted to hormonal changes in the climacteric, but to the entire social environment aggravated by the social restriction experienced [30]. In the period after social isolation, smaller numbers of psychological symptoms belonging to the domains of anxiety and attractiveness were observed, which may be closely linked to the return of extra-family social relationships. As a result of the consolidation of social restrictions, the rates of domestic and sexual violence showed an ascending pattern, justified by the greater coexistence of these women with their spouse, which directly impacts their mental health [21].
Conclusion
The data from the present study allow us to state that the social isolation caused by COVID-19 did not impair the quality of life and self-care attitudes of women in the climacteric and menopause when compared before, during and after social restriction. There was a greater number of complaints related to urogenital symptoms during social isolation and after its end, in addition to the reduction in somatic symptoms, observed in the SIP group. The other symptoms did not have a significant impact.
Final Considerations
The COVID-19 pandemic brought great challenges to humanity, both about adaptations to restrictions aimed at protecting the spread of the virus, as well as the emotional and physical impacts caused by social isolation, and the way humanity finds itself after the removal of these restrictions. It is hoped that the findings of the present study will help to elucidate where we were during the pandemic and where this population is, encouraging actions and research that can better support climacteric and menopausal women. Strengthening self-care and health care measures to understand the real influence of the COVID-19 pandemic on climacteric and menopause.
It is reasonable to assume that the present study has some limitations, such as the comparison of different groups of women in three different evaluation moments, divergent number of populations between the groups that, even treated statistically, is a factor that we would like to better control, lack of physical characteristics of the sample, the separate grouping of climacteric and menopausal women and the implementation of different methodology in the sample groups.
Declarations
The authors declare that no funding, subsidy, or other support was received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose. All authors contributed to the conception and design of the study. The preparation of the material, data collection and analysis were carried out by all authors. The first draft of the manuscript was written by Camila Oliveira Serra and all authors have commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical Approval Proof
This study was carried out in accordance with the principles of the Helsinki Declaration. Approval was granted by the ethics committee of the Federal University of Sergipe (09/04/2020 – nº1629941970005546).
References
- Antunez-Garcia V, Munoz-Mendoza CL (2019) Sexual function and health related quality of life in climacteric women with genital prolapse in Family Health Centers of the Ñuble region Rev chil obstet Ginecol 84(5): 346-354.
- Ferreira VC, Ferreira da Silva MR, Montovani EH, Necklaces LG, Ribeiro AA, et al. (2020) Saúde da mulher, gênero, políticas públicas e educação médica: problemas no contexto da pandemia. Revista Brasileira de Educação Médica 44:1.
- Schneider HPG, Birkhäuser M (2017) Qu alidade de Vida em mulchers climaté Climatério 3: 187-194.
- Souto K, Moreira MR (2021) Política Nacional de Atenção Integral À Saúde da Mulher: protagonismo do movimento de mulheres. Saúde Debate 45(130).
- Benetti IC, Lia da Silva Sales, Ana Paula da Rosa Deon, Fernanda Ax Wilhelm, Joao Paulo Roberti (2019) Climatério, enfrentamento e repercussões no contexto de trabalho: vozes do Extremo Norte do Brasil. Revista Kairós-Gerontologia 22(1): 123-146.
- (2008) Brasil. Ministério da Saú Manual de Atenção à Mulher no Climatério / Menopausa.
- Maciel JBL (2021) Vivência e concepção da mulher acerca do climatério: Uma revisão bibliográ Research, Society and Development 10: 6.
- Lima AM, Josiane Santos Brant Rocha, Viviane Margareth Chaves Pereira Reis, Marise Fagundes Silveira, Antônio Prates Caldeira, et al. (2019) Perda da qualidade do sono e fatores associados entre mulheres climaté Ciência e Saúde Coletiva 24(7): 2667-2678.
- Tossin B, Souto Valquíria Toledo, Terra Marlene Gomes, Siqueira Daiana Foggiato de, Mello, Amanda de Lemos, et al. (2016) Educational practices and self-care: evidence in the scientific production of nursing / Educational practices and self-care: evidence in scientific production of nursing. REME rev min enferm 20: 940.
- OMS (2016) The Global strategy and action plan on ageing and health.
- Piecha VH (2018) Percepções das mulheres sobre o climaté Res Encontrado, 10.
- Garcia RMC, Garcia IC (2017) Concepção sociocultural do climatério no Ocidente. Cult cuid 21: 108-114.
- Leite PMG, Serra CO, de Souza KOC, Silva JRS, Santos ES, et al. (2022) COVID-19: Climacteric symptomatology and quality of life. Mediterranean Nursing and Midwifery 2(2): 62-68.
- Caçador MS (2003) Questionário de Saúde da Mulher (QE): Perguntas Frequentes (FAQ). Resultados de Saúde e Qualidade de Vida.
- Filho CRS, Edmundo Chad Baracat, Lucieni de Oliveira Conterno, Mauro Abi Haidar, Marcos Bosi Ferraz (2005) Sintomas climatéricos e qualidade de vida: validade do questionário de saúde da mulher. Rev Saúde Pública 39(3).
- Heinemann LAJ, Potthoff P, Schneider HPG (2003) Versões internacionais da Menopause Rating Scale (MRS). Health Qual Life Outcomes. 1:28
- Gazibara T (2022) Um estudo comparativo dos sintomas do climatério entre duas populações de mulheres de meia-idade. Revista de Obstetricia e Ginecologia 42(6): 2178-2184.
- El-Fatah ANK, Abdalsalam Abdullah Alshehri, Fatma H Alsulami, Norah Alasmari, Nermin A Osman (2022) Association Between Mental Health Outcomes and Changes in Lifestyle Behavior Index Among Saudi Adults 16 Weeks After COVID-19 Pandemic Lockdown Release. Front Public Health 4(9): 728117.
- Mainar BL (2021) Conhecimento das mulheres sobre a síndrome geniturinária da menopausa: adesão aos seus tratamentos na era COVID-19 em uma amostra delas: estudo COMEM-GSM. BMC Women's Health 21: 398.
- Trento SRSS, Madeiro A, Rufino AC (2021) Funções sexual e fatores associados em mulheres na pós- menopausa. Revista Brasileira de Ginecologia e Obstetrícia 43(7).
- Souza ASR, Souza GFA, Praciano GAF (2020) A saúde mental das mulheres em tempos de COVID-19. Revista Brasileira de Saúde Materno Infantil 20(3).
- Xiong A (2022) Associações longitudinais entre a qualidade do sono e os sintomas da menopausa entre mulheres climatéricas residentes na comunidade: um estudo multicê Sleep Medicine 100: 198-205.
- Yuksel B, Ozgor F (2020) Effects of the COVID-19 pandemic on female sexual behavior. International Journal of Gynecology e Obstetrics 150(1): 98-102.
- Costa JG (2017) O treinamento físico combinado reduz os sintomas climatéricos sem os efeitos aditivos da suplementação de isoflavonas: um estudo clínico, controlado, randomizado, duplo-cego. Revistas SAGE 23(4).
- Blanco M, Cstar M, Sequetle M (2021) Avaliação on-line da percepção da solidão e fatores associados em mulheres climatéricas colombianas durante a pandemia de COVID-19: um estudo transversal. Perspectiva da promoção da saúde 11(2): 230-239.
- Kułak-Bejda A (2023) Avaliação de risco de depressão entre mulheres durante a menopausa antes e durante a pandemia de COVID-19. J Int de Pesquisa Ambiental e Saúde Pública 20(1): 596.
- Schmidt B, Maria Aparecida Crepaldi, Simone dill Azeredo Bolze, Lucas neiva-silva, Lauro miranda demenech (2020) Saúde mental e intervenções psicológicas diante da pandemia do novo coronavírus (COVID-19). Estud Psicol p .37.
- Mello A (2021) Sintomas da menopausa no sudoeste dos Estados Unidos: uma pesquisa transversal de mulheres de áreas com diferentes recursos socioeconô Menopausa e saúde a longo prazo em populações vulneráveis 154: 7-12.
- Yoeli H, Macnaughton J, Mclusky S (2021) Menopausal symptoms and work: A narrative review of women’s experiences in casual, informal, or precarious jobs. Maturitas 150: 14-21.
- Rodrigues MAH (2021) Menopausa, cognição, ondas de calor e COVID-19: o estrogênio é uma peça fundamental no quebra-cabeça? Mulheres & saúde 61: 393-394.






























