Predictive Value of Sflt-1/Plgf Ratio for Occurrence of Preeclampsia in Singleton Pregnancies: A Retrospective Study
Tanja Milić-Radić1*, Dobriša Radić2, Branka Čančarević-Đajić1 and Bojana Popović1
1Clinic for gynecology and obstetrics, University Clinical Center of Republic of Srpska, Bosnia and Herzegovina
2Health Insurance Fund of Republic of Srpska, Bosnia and Herzegovina
Submission: March 13, 2023; Published:April 12, 2023
*Corresponding author: Tanja Milić-Radić, Clinic for gynecology and obstetrics, University Clinical Center of Republic of Srpska, Bosnia and Herzegovina
How to cite this article: Tanja M-R, Dobriša R, Branka Č-Đ, Bojana P. Predictive Value of Sflt-1/Plgf Ratio for Occurrence of Preeclampsia in Singleton Pregnancies: A Retrospective Study. Glob J Reprod Med. 2023; 9(5): 555773. DOI: 10.19080/GJORM.2023.09.555773.
Abstract
Introduction: Preeclampsia is multisystem disorder of pregnancy, characterized by endothelial and placental dysfunction. It is classified as an early onset (which occurs < 34 weeks) and late onset (which occurs ≥ 34 weeks). There is an increase of level of antiangiogenic factor of soluble form similar to tyrosine kinase 1 (sFlt-1) and decrease of level of proangiogenic placental growth factor (PlGF) at preeclampsia. High ratio sFlt-1/PlGF is connected to occurrence of preeclampsia.
Materials and Methods: There was a retrospective study of the Clinic for Gynecology and Obstetrics of the University Clinical Center of Republic of Srpska (KGA UKC RS), which was implemented in period January 1st, 2020 – December 31st, 2021 and which included 224 patients hospitalized at the Department of Perinatology for suspected preeclampsia development, from 26+0 weeks of gestation until birth. One of the key criteria for the inclusion of patients in the study is the use of the sFlt-1/PlGF ratio as a marker for the onset of preeclampsia, and the determination of protein values in 24-hour urine (biuret). The antenatal state of the fetus was also monitored by ultrasound measurement of the flow resistance ratio (Ri) through the middle cerebral artery and the umbilical artery (C/U), as well as the values of the newborn’s Apgar score in the first and fifth minute of life (AS 1 and 5). The patients included in the study were divided into two groups according to gestational age: group 1 (<33+6 NG) and group 2 (≥34NG). For the purposes of the research, data from patient protocol books for the specified period, as well as corresponding data from the Clinical Information System (KIS), were used.
Results: Calculated values for cut off 38 for group 1 are: NPV= 76.9%, PPV=72.0%, sensitivity=85.7%, specificity=58.8%, and for group 2 are: NPV= 89 ,1%, PPV=40.8%, sensitivity=72.1%, specificity=68.5%. For cut off 85, the calculated values for group 1 are: NPV= 82.4%, PPV=85.7%, sensitivity=85.7%, specificity=82.4%, and for group 2 they are: NPV= 84.9 %, PPV=70.4%, sensitivity=44.2%, specificity=94.4%. For cutt off 110, the calculated values for group 1 are: NPV= 77.8%, PPV=85%, sensitivity=81%, specificity=82.4%, and for group 2 they are: NPV= 83.5 %, PPV=72.7%, sensitivity=37.2%, specificity=95.8%. The measured value of protein in 24h urine (biuret) in comparison with the measured values of the sFlt-1/PlGF ratio have statistical significance for predicting the onset of preeclampsia. Statistical data processing obtained by examining the measured values of the sFlt-1/PlGF ratio and the antenatal and natal condition of the fetus (C/U and AS 1 and 5) showed statistical significance, except for C/U for group 2, where p=0.32.
Conclusion: Determination of the sFlt-1/PlGF ratio as well as biuret and monitoring of the antenatal and postnatal state of the fetus significantly contributes to the timely diagnostic of preeclampsia, which impacts reducing the incidence of undesirable outcomes for the mother and the fetus.
Keywords: Preeclampsia; sFlt-1; PlGF; Biuret; Apgar score; Pregnancy
Introduction
Preeclampsia is a multisystem disorder of pregnancy, characterized by endothelial and placental dysfunction [1]. The definition that originally included hypertension and proteinuria after the 20th week of gestation (NG) was expanded to include hypertension in combination with renal and hepatic dysfunction, as well as thrombocytopenia. Preeclampsia is classified as early (occurring < 34NG) and late (occurring ≥ 34NG). The clinical picture varies from mild to severe, potentially life-threatening [2]. On an annual level, it occurs in 2-8% of pregnant women and, according to available data, it is responsible for 50,000 maternal deaths worldwide [3-9]. The only known prevention is the use of Aspirin, and the only therapy is termination of pregnancy, i.e., childbirth, so it is one of the most common reasons for iatrogenic prematurity [1].
Preeclampsia is primarily caused by diseases of the blood vessels, especially the endothelium, and is considered to be caused by reduced placental perfusion, hypoxia, inflammation and oxidative stress. The balance of proangiogenic and antiangiogenic factors in the circulation is disrupted in preeclampsia. There is an increase in the level of antiangiogenic factor of soluble form similar to tyrosine kinase 1 (sFlt-1) and a decrease in the level of proangiogenic placental growth factor (PlGF). A high ratio of sFlt- 1/PlGF is associated with the occurrence of preeclampsia, which was proven before clinical use [1,10].
The current “gold standard” for preeclampsia involves measuring blood pressure and finding protein in the urine. Considering the different clinical features of preeclampsia, the specificity and sensitivity of these measurements to predict the onset of preeclampsia, eclampsia and HELLP syndrome is quite low. As a result, we often have unnecessary hospitalization and intensive monitoring of pregnant women “waiting” for preeclampsia to develop, and on the other hand, the necessary hospitalization of patients who are not clinically predicted to develop preeclampsia according to the mentioned criteria may be missed [11]. The German Association of Obstetricians and Gynecologists, as well as the Austrian and Swiss Association of Obstetricians and Gynecologists, currently recommend the use of angiogenic biomarkers as a means of diagnosis and short-term prediction of preeclampsia in patients suspected of developing this disease. The 2018 Guideline of the European Association of Cardiology recommends the use of the sFlt-1 /PlGF ratio for the treatment of cardiovascular disease in pregnancy [2].
Goals
a) to determine the specificity, sensitivity, negative predictive value (NPV) and positive predictive value (PPV) of the sFlt-1/PlGF ratio in examined patients for the onset of preeclampsia.
b) to examine the statistical significance of determining the biuret value and the sFlt-1/PlGF ratio in preeclampsia diagnostics.
c) to examine the statistical significance of the influence of the sFlt-1/PlGF ratio on the antenatal and neonatal condition of the newborn.
Material and Methods
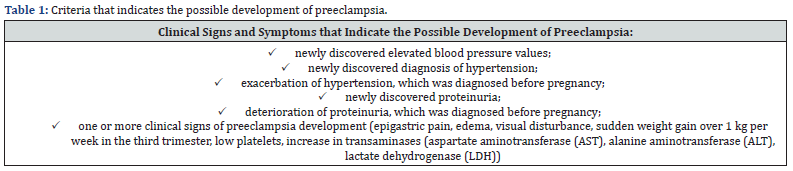
In the Clinic for Gynecology and Obstetrics of the University Clinical Center of the Republic of Srpska (KGA UKC RS), a crosssectional retrospective study was conducted for the period January 1, 2020 - December 31, 2021, which included 224 patients hospitalized in the Department of Perinatology due to suspected development of preeclampsia, from 26+0 weeks of gestation until delivery. The criteria for identifying patients suspected of developing preeclampsia are shown in table 1. One of the key criteria for the inclusion of patients in the study is the clinical use of the serum sFlt-1/PlGF ratio as a marker for the onset of preeclampsia, which was measured on the day of admission (value 1), and in some cases, depending on the value of the sFlt-1/PlGF ratio, the measurements were repeated two, three or four times at intervals of seven days, as well as the measurement of the biuret value. An ultrasound scan and C/U determination were routinely done to patients, as well as AS 1 and 5 in the Maternity Ward. For the purposes of the research, data from patient protocol books for the specified period, as well as corresponding data from the Clinical Information System (KIS), were used.
Criteria for inclusion in the study
I. pregnant women of gestational age over 26 weeks of pregnancy until delivery, who have been diagnosed with one or more criteria that indicate the possible development of preeclampsia.
Criteria for exclusion from the study
I. essential hypertension without deterioration of the clinical picture.
II. proteinuria that existed before pregnancy without deterioration of the clinical picture.
III. Twin pregnancy.
The patients included in the study were divided into two groups according to gestational age:
group 1 (<33+6 NG) i
group 2 (≥34NG).
The ꭕ2 test, Mann Whitney non-parametric test and ROC analysis were used for statistical data processing, and those with p<0.05 were considered statistically significant differences.
Results
In the observed period, 224 patients were hospitalized in the Department of Perinatology at the KGA UKCRS due to suspected development of pre-eclampsia from 26+0 weeks of gestation until delivery, who met the requirements for inclusion in the study. The results of the measured sFlt-1/PlGF ratios in the patients included in the study were divided into two groups, according to gestation, with the risk of early and late preeclampsia (<34NG and ≥34NG), and the negative predictive value (NPV) and positive predictive value (PPV), specificity, sensitivity of the sFlt-1/PlGF ratio depending on gestation and the calculated value of the marker were statistically calculated. The values of the sFlt-1/PlGF ratio were calculated on the day of hospitalization, and depending on the measured values, they were repeated two, three or four times at intervals of 2-4 days.
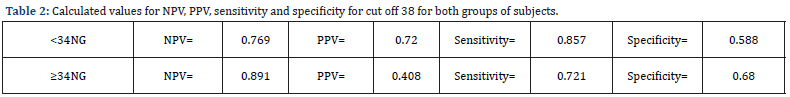
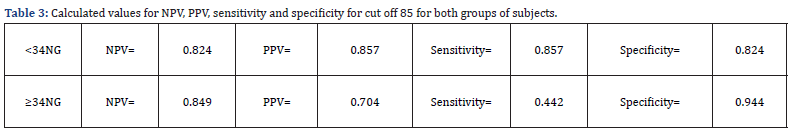
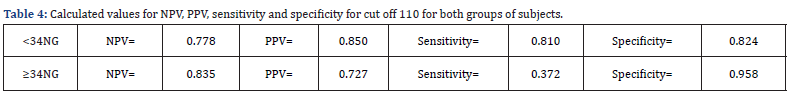
Depending on the gestational age of the pregnancy, the sFlt- 1/PlGF ratio was examined for cut offs of 38, 85 and 110 for the examined groups 1 and 2 after the first measurement, and for each cut off for both groups the calculated values for NPV, PPV, sensitivity, specificity and they are shown in tables 2-4.
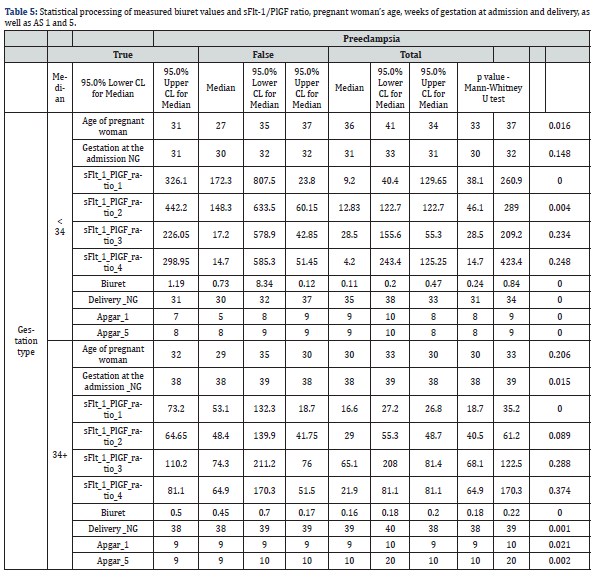
Statistical processing of the data obtained by measuring the value of the biochemical marker of preeclampsia, biuret, the sFlt-1/PlGF ratio, as well as the age of the pregnant woman, the week of gestation of the subjects at admission and at the end of the pregnancy, and AS 1 and 5, showed statistical significance in the first measurements of the sFlt-1/PlGF ration with p<0.05, and all other measurements have a statistical significance of p>0.05 for both groups. The measured biuret values, as well as AS 1 and 5, have statistical significance for the occurrence of preeclampsia in both groups. Gestation of pregnancy at the admission of the pregnant woman has no statistical significance in the first group, and in the second group it is p=0.15, while gestation of pregnancy at delivery has statistical significance in both groups. The age of the pregnant woman in the first group has statistical significance of p=0.016, while in the second group it has no statistical significance (Table 5).
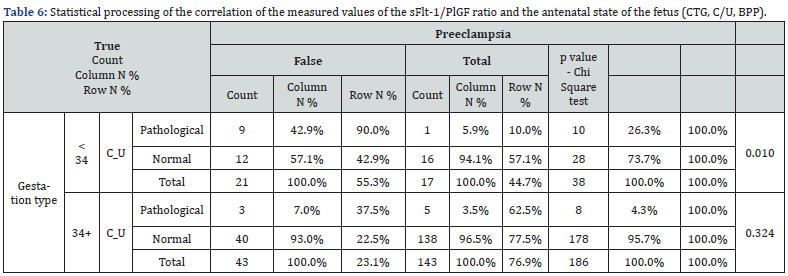
Statistical processing of the data obtained by examining the measured values of the sFlt-1/PlGF ratio and the antenatal state of the fetus (C/U) showed a statistical value of p=0.01 in the first group, while in the second group it was p>0.05 (Table 6).
Discussion
Preeclampsia is one of the most important factors affecting maternal morbidity and mortality and one of the most common reasons for iatrogenic prematurity, and it requires improvement in diagnostics and treatment. High values of blood pressure and proteinuria have little predictive value and when they are manifested in most cases they are associated with unfavorable outcomes for mother and fetus [5-8]. Proangiogenic and antiangiogenic factors are involved in the pathophysiology of the mechanism of preeclampsia, and numerous studies have proven high NPV, PPV, sensitivity and specificity of the sFlt-1/PlGF ratio in predicting the onset of preeclampsia [11,12].
The patients included in our study met the criteria listed in table 1. The values of the sFlt-1/PlGF ratio and biuret were measured and also upon admission to the Department of Perinatology, the Doppler ultrasound with the C/U ratio was routinely done in order to monitor the condition of the fetus. After delivery, AS 1 and 5 were determined in newborns by the competent gynecologist or pediatrician in the Maternity Ward and we used this as parameter for monitoring the delivery outcome.
The criteria for termination of pregnancy were initially measured extremely high values of the sFlt-1/PlGF ratio, as well as a significant increase in the value of the sFlt-1/PlGF ratio during re-measurement if the initially measured value was higher than 85. The values were re-measured at 2- 4 days, according to current guidelines. At our Clinic, biuret is routinely measured in patients suspected of developing preeclampsia, so we included these values in the study, which showed statistical significance as a parameter in predicting the occurrence of preeclampsia.
Patients who are hospitalized at the Department of Perinatology of the UKC RS have daily Doppler ultrasound measurements of the C/U ratio, as a parameter to monitor the state of the fetus. If the pathological flow values are measured, termination of the pregnancy is planned, either by induced delivery or caesarean section depending on the obstetric findings and gestation of the pregnancy, regardless of the values of the sFlt- 1/PlGF and biuret ratio. During the observed period, we had one stillborn child at 29weeks of gestation, where the measured value of the sFlt-1/PlGF ratio before delivery was 1401. I must mention that KGA UKC RS is a reference institution in our country, and we provide care for all patients with pregnancy complications sent from other institutions. Sometimes patients are not referred in a timely manner, and because of this, an undesirable outcome can occur. All patients included in the study were provided with care in our clinic after giving birth and we had no adverse outcomes.
Our study showed a fairly high NPV, PPV, as well as the sensitivity and specificity of the sFlt-1/PlGF ratio in the onset of preeclampsia, but the results are partially different compared to studies that included a significantly larger number of subjects. In Zeisler’s study, measurements of the sFlt-1 /PlGF ratio for a cutoff 38 show NPV 98.9%, PPV 40.7%, while sensitivity is 88.2%, with specificity of 80% [12]. In Hund’s study, the results for NPV, PPV, sensitivity and specificity are similar to Zeisler’s [3]. The difference in the results between our study and those mentioned is due to the smaller number of subjects included in study group 1, which produced different statistical results. In the second group, we had a significantly larger number of subjects, and we obtained results that are closer to the results in Zeisler’s and Hund’s study. Examination of the measured biuret values in correlation with the sFlt-1/PLGF ratio showed that the diagnostic of preeclampsia improves in both studied groups and this is also similar to the results of the Zeisler study and to the recommendations of the American Association of Obstetricians and Gynecologists (ACOG) [12].
By examining the statistical association of the sFlt/PlGF ratio with the antenatal condition of the fetus, which is shown by the C/U ratio, it was proven that there is statistical significance in the first group, while it does not exist in the second group. Examination of the postnatal condition of the newborn by determining the AS 1 and 5 values was found to be statistically significant in both examined groups. This confirms the main goal of the study, which is to reduce the frequency of undesirable outcomes for the mother and the fetus. Both Zeisler’s and Hudn’s study and numerous international studies dealt with this issue, and they proved that the measurement of the sFlt-1/PlGF ratio has statistical significance in the prognosis of preeclampsia, and therefore in the improvement of perinatal morbidity and mortality [3,12].
World guidelines for the management of preeclampsia in pregnancy recommend measuring of the sFlt-1/PlGF ration in the prediction of the preeclampsia occurrence, which is certainly shown by our study [3].
Conclusion
There are numerous evidence proving that preeclampsia is a systemic disease that affects multiple organs, and the isolated clinical criteria are not adequate to predict adverse outcomes. The use of markers related to angiogenesis, including the sFlt-1/PlGF ratio, to predict the occurrence of preeclampsia has found wide application in medical practice and it is recommended by certain national guidelines for obstetricians and gynecologists. Our study, with its results, which does not deviate significantly from other similar studies, showed that the determination of the sFlt-1/ PlGF ratio significantly contributes to the timely diagnostics of preeclampsia, and further contributes to reducing the frequency of adverse outcomes for the mother and fetus, including iatrogenic premature births, and thus also to reducing costs related to hospitalizations.
References
- Klein E, Schlembach D, Ramoni A, Langer E, Bahlmann F, et al. (2016) Influence of the sFlt-1/PlGF Ratio on Clinical Decision-Making in Women with Suspected Preeclampsia. PLoS One 11(5): e0156013.
- Stepan H, Hund M, Andraczek T (2020) Combining Biomarkers to Predict Pregnancy Complications and Redefine Preeclampsia: The Angiogenic-Placental Syndrome. Hypertension 75(4): 918-926.
- Hund M, Verhagen-Kamerbeek W, Reim M, Messinger D, Van der Does R, et al. (2015) Influence of the sFlt-1/PlGF ratio on clinical decision-making in women with suspected preeclampsia-the PreOS study protocol. Hypertens Pregnancy 34(1): 102-115.
- Ananth CV, Keyes KM, Wapner RJ (2013) Pre-eclampsia rates in the United States, 1980-2010: age-period-cohort analysis. BMJ 347: f6564.
- Hernández-Díaz S, Toh S, Cnattingius S (2009) Risk of pre-eclampsia in first and subsequent pregnancies: prospective cohort study. BMJ 338: b2255.
- Skjaerven R, Wilcox AJ, Lie RT (2002) The interval between pregnancies and the risk of preeclampsia. N Engl J Med 346: 33-38.
- Duley L (2009) The global impact of preeclampsia and eclampsia. Semin Perinatol 33: 130-137.
- Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371: 75-84.
- McClure JH, Cooper GM, CluttonBrock TH (2011) Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006-2008: a review. Br J Anaesth 107: 127-132.
- Hund M, Allegranza D, Schoedl M, Dilba P, Verhagen-Kamerbeek W, et al. (2014) Multicenter prospective clinical study to evaluate the prediction of short-term outcome in pregnant women with suspected preeclampsia (PROGNOSIS): study protocol. BMC Pregnancy Childbirth 14: 324.
- Stepan H, Herraiz I, Schlembach D, Verlohren S, Brennecke S, et al. (2015) Implementation of the sFlt-1/PlGF ratio for prediction and diagnosis of pre-eclampsia in singleton pregnancy: implications for clinical practice. Ultrasound Obstet Gynecol 45(3): 241-246.
- Zeisler H, Llurba E, Chantraine F, Vatish M, Staff AC, et al. (2016) Predictive Value of the sFlt-1:PlGF Ratio in Women with Suspected Preeclampsia. N Engl J Med 374(1): 13-22.






























