An Antenatal Diagnostic of Laparoschisis: Case Report
Mariam Mahtate*, Khaoula Lakhdar, Soukaina cherradi, Najia Zeraidi, Amina Lakhdar and Aziz Baydada
Department of Gynecology Obstetrics and Endoscopy, University Mohammed V, Morocco
Submission: March 13, 2023; Published:March 23, 2023
*Corresponding author: Mariam Mahtate, Department of Gynaecology Obstetrics and Endoscopy, Mohammed V of Rabat, Morocco
How to cite this article: Mariam Mahtate, Khaoula Lakhdar, Soukaina cherradi, Najia Zeraidi, Amina Lakhdar and Aziz Baydada. An Antenatal Diagnostic of Laparoschisis: Case Report. Glob J Reprod Med. 2023; 9(5): 555771. DOI: 10.19080/GJORM.2023.09.555771.
Abstract
The laparoschisis is a parietal anomaly that is part of the meteoric coelosomies. It is characterized by an enlargement of the right lateral-umbilical level of the viscera. Its frequency is estimated at 1 in 2700 births and its final prognosis is excellent, depending on the ischemic lesions, for which therapeutic management is often limited. No genetic cause is currently incriminated in the genetics of laparoschisis apart from its association with syndromic groups. The diagnosis is suspected prenatally allowing a better therapeutic approach. Its management is essentially surgical in the absence of irreversible ischemic lesions. Here we illustrate the case of a young couple in whom the antenatal diagnosis highlighted the antenatal diagnosis of laparoschisis at 35 SA .in which the cesarean section allowed the extraction of a newborn male with a good Apgar and who immediately underwent an operation to reintegrate the viscera and to close the abdominal defect by the pediatric surgeons. The baby is doing well without any complications; good psychomotor development with a follow-up of 1 year.
Keywords: Laparoschisis; Congenital malformation; Pregnancy; Antenatal diagnosis
Introduction
The laparoschisis is a rare congenital malformation, it is a parietal anomaly that is part of the meteoric coelosomies like omphalocele; characterized by an eversion at the right lateral-umbilical level of early embryonic development, gastroschis is the most common cause of a vascular defect during the development of the abdominal wall at the 12th week of pregnancy [1].
Laparoschisis has an incidence of 1:2000 live births. The sex distribution is male: female = 1.5:1 in omphaloces, 1:1 in gastroschises, respectively. Its frequency in the general population is estimated at 1 in 2700 births; the prevalence of gastroschisis has increased, leading some to call it a pandemic [2].
No risk factors have been identified nor has a genetic cause been suggested apart from its association with other congenital malformations such as prune belly syndrome. Prognosis is linked to the functional quality of the intestinal loops but is excellent in more than 90% of cases. Our case allows us to highlight the importance of antenatal diagnosis allowing better care in adequate health centers with the necessary technical platform.
Case Report
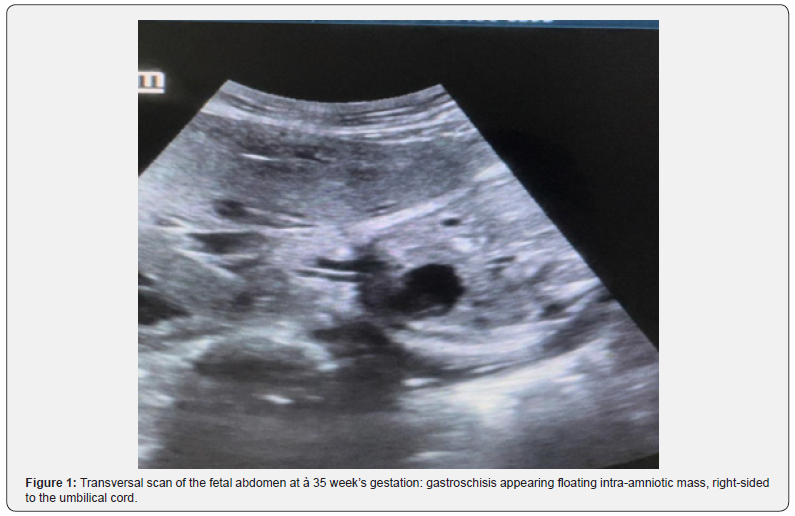
It is the case of a young couple, the father 28 years old with no particular history, no notion of tobacco or cocaine or amphetamines consumption, the mother 26 years old with no particular history, no notion of toxic consumption, no notion of family antecedents, it was her first pregnancy not followed by 35 weeks of amenorrhea; never an obstetrical ultrasound until now. she consulted for regular uterine contractions; the obstetrical examination found an unfavorable bishop; and the ultrasound revealed a monofetal pregnancy with laparoschisis (Figure 1) without signs of fetal malformations or associated digestive complications. We carried out a bacteriological assessment (endocervical, exocervical sample and urinary cytobacteriological examination) were negative. The inflammatory assessment is slightly disturbed: CRP at 11 mg/l and hyperleukocytosis at 13.3 G/l. The fetal heart rate was normal.
Since it was a non-monitored pregnancy, we preferred to perform a caesarean section at 36 weeks after fetal lung maturation and after consulting the pediatric surgeons. The caesarean section allowed the extraction of a male newborn with a birth weight of 3000 g; Apgar 10/10; with an exteriorization of the viscera (Figure 2), who was immediately transferred to the operating room for an immediate parietal repair by the pediatric surgeons. The duration of hospitalization was 10 days. The newborn has no complications to this day with good psychomotor development.

Discussion
Laparoschis is a rare, complex pathology associated with an important morbimortality, hence the interest of antenatal diagnosis which remains easy if the antenatal ultrasound followup is well done. With an incidence according to European statistics Eurocat 1.92 per 10,000 births with an upward trend in this frequency [3], which can be explained by the improvement of ultrasound resources, access to care and the improvement of pregnancy monitoring and ultrasound prenatal screening.
This congenital anomaly is defined by the exit of free viscera in the amniotic liquid through an orifice in the abdominal wall, constituted by the gall and or colonic anses [4], which is the case of the newborn baby of this case report, the exit of the gall and colonic anses, as the images show, as well as other organs as the stomach or the liver. The only differential diagnosis is omphalocele which is more frequent, occurs earlier in embryonic development, and is associated in half of the cases with other malformations.
In the majority of the described cases, it is about an isolated malformation without genetic anomalies [5,6], also several cases mention recurrent obstetrical factors not yet labelled as risk factors: young maternal age, primiparity, smoking, taking of drug [7]. In our case we find the young maternal age, primiparity and notion of passive smoking. This gives all the importance to the neonatal ultrasound screening allowing the rapid surgical management thus allowing the decrease of the mortality rate around 10% [7], if not others digestives lesions are associated such as digestive ischemia, volvulus, and digestive atresia’s. However, these lesions are difficult to assess in the prenatal period and do not allow to anticipate neonatal evolution; hence the need to transfer these patients to structures with adequate technical facilities. All this is only possible thanks to neonatal ultrasound screening.
The timing and route of delivery remain controversial. Some authors as Dixon, who observes up to 12.5% perinatal mortality, recommends delivery at 35 weeks. Avoiding the late aggravation of digestive lesions would be preferable to the potential complications of prematurity [8]. Gastroschisis is a surgical emergency. Primary abdominal closure is not always possible and different techniques of delayed management may be resorted to. This is the situation of our case, the antenatal diagnosis allowed the rapid surgical management of the newborn, which allowed a good prognosis for the newborn.
Conclusion
Laparoschisis is a common pathology in pediatrics and is life-threatening. The treatment is surgical. and the prognostic depend essentially on the extent of the defect and any associated complications. Antenatal diagnosis followed by a careful survey for other fetal anomalies results in optimal antenatal management and planned delivery at a facility capable of providing necessary neonatal support.
Guarantor of Submission
The corresponding author is the guarantor of submission.
Funding
There are no funding sources to be declared.
Availability of Data and Materials
Supporting material is available if further analysis is needed.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics Approval and Consent to Participate
Ethics approval has been obtained to proceed with the current study. Written informed consent was obtained from the patient for participation in this publication.
References
- Langman J, Sadler TW (2007) Embryologie medicale, 8e, Edn, Pradel.
- Yazdy MM, Werler MM, Anderka M, Langlois PH, Vieira VM (2015) Spatial analysis of gastroschisis in Massachusetts and Texas. Ann Epidemiol 25: 7-14.
- Dolk H (2005) Eurocat: 25 years of European surveillance of congenital anomalies. Arch Dis Child Fetal Neonatal Ed 90(5): F355-F358.
- Japaraj RP, Hockey R, Chan FY (2003) Gastroschisis: can prenatal sonography predict neonatal outcome? Ultrasound Obstet Gynecol 21[4]: 329-333.
- Brun M, Maugey-Laulom B, Rauch Chabrol F, Grignon A, Diard F (1998) Diagnostic Echographique antenatal des malformations de la paroi anterieure du fœtus. J Radiol 79: 1461-1468.
- Foucher C, Herve P, Lardy H, Perrotin F (2008) Disparition prenatale spontanee d’un laparoschisis: une evolution de mauvais pronostic. J Gynecol Obstet Biol Reprod 37(3): 302-307.
- Alfaraj MA, Ryan G, Langer JC, Windrim R, Seaward PGR, et al. (2011) Does gastric dilation predict adverse perinatal or surgical outcome in fetuses with gastroschisis? Ultrasound Obstet Gynecol 37(2): 202-206.
- Moir CR, Ramsey PS, Ogburn PL, Johnson RV, Ramin KD (2004) A prospective trial of elective preterm delivery for fetal gastroschisis. Am J Perinatol 21: 289-294.






























