Spontaneous Rupture of Splenic Artery Aneurysm Reported cause of Post-Partumcollapse
AL Mulla AA*1,2, Nazim AL Rifai3, Abdul Kareem S1 and S S Sreenisha4
1Laifa Hospital, Dubai
2Dubai Fertility Centre, UAE
3Rashid Hospital, DHA, UAE
4AL KhorHospital, Qatar
Submission: June 20, 2017; Published: July 28, 2017
*Corresponding author: AL Mulla AA, Consultant OBSGYN, Laifa Hospital, Dubai Fertility Centre, Dubai Health Authority, Dubai, United Arab Emirates, Tel :+971551110221; Email: aaalmulla@dha.gov.ae
How to cite this article: AL Mulla AA, Nazim A R, Abdul K S, S S Sreenisha. Spontaneous Rupture of Splenic Artery Aneurysm Reported cause of Post-Partumcollapse. Glob J Reprod Med. 2017; 2(1): 555579. DOI: 10.19080/GJORM.2017.02.555579
Abstract
Splenic artery aneurysm (SAA) is a rare condition, with a prevalence of 1% [1]. However, potentially fatal .The importance of splenic artery aneurysm lies in the risk for rupture and life threatening hemorrhage, which occurs in 10%of cases with a mortality rate of 10-25% in non-pregnant patient and up to 70% during pregnancy [2]. It accounts for about 60% of all splanchnic arterial aneurysms. It only follows aortic and iliac arteries aneurysms as the third most common intra-abdominal aneurysm [1]. We report a case of rupture SAA at Latifa Hospital, a government tertiary hospital, Dubai Health Authority, Dubai, UAE, where 5586 deliveries was registered in the year 2014. Hospital Authority obtained ethical Clearance for this case report.
Case Presentation
34 years old Grand Multi para gravida 13, para 10, 38 weeks pregnant, admitted to the Labor ward aiming for spontaneous vaginal delivery with unremarkable past medical or surgical history, and no history of previous hospitalization. Labor course was observed and as per protocol failure to progress documented, thus caesarean section was carried on in the first stage of labor , with uneventful intra operative course , and outcome of a healthy male baby weighing 4.1Kg. The patient sent to the observation room, where she collapsed in the first hour, showing signs of shock, with elements of intra abdominal bleeding, bedside ultrasound proved this finding. Uterus contracted well and there was no vaginal bleeding.
Decision for immediate exploratory laparotomy and performed by the senior team; meanwhile resuscitation was running adequately by blood and blood products replacement. Intra operative findings revealed a massive haemo peritoneum, sucked, calculated and replaced adequately. The uterus found to be adequately contracted, normal in shape with normal adnexa , intact suturing sites and no bleeding from down.
We observed profuse bleeding running from upper abdomen. Liver is normal in shape, bleeding run from spleen site which packed with abdominal gauze waiting for the surgeon input, who discovered that the bleeding came from splenic artery, which was ligated immediately, followed by splenectomy, upon proper dissection it was proved that a rupture splenic artery aneurysm was the cause of the hemorrhage (Figure 1).
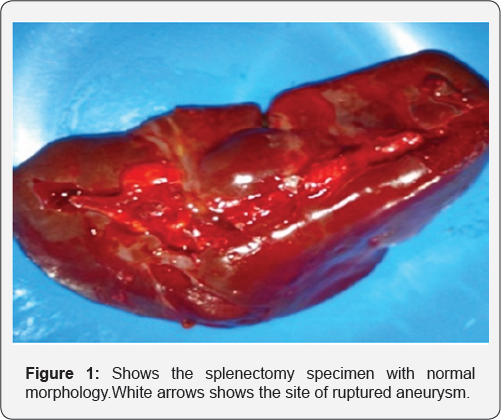
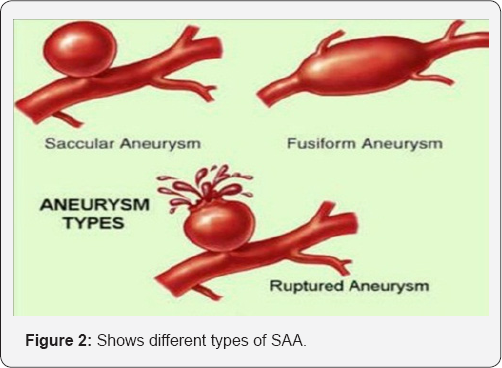
We cannot identify the type of this ruptured aneurysm (Figure 2).
The patient picked up vitally and became more stable, all organs were explored again, no bleeding confirmed.
Closure of anterior abdominal wall done in layers, the patient tolerated the anesthesia and post-operative period with no complications. Antibiotics, thromboprophylaxis were given. Further management was planned for future vaccinations for pneumococcal, meningococcal, and hemophilus influenza vaccines.
Discussion
The vast majority of SAA, being smaller than 2 cm, remains asymptomatic and is generally encountered as an autopsy finding [3]. Nevertheless, up to date, more than 400 cases of ruptured SAA have been reported in the international literature, with approximately 30% of these during pregnancy. Moreover, almost all cases of ruptured SAA in pregnancy have occurred during the third trimester. Thus, it is evident that the physical history of pregnancy gradually increases the risk of rupture of SAA. Apart from the late stage of pregnancy, other risk factors include multipart, portal hypertension, atherosclerosis, and fibro dysplasia [4]. One of the mechanisms promoting the vascular defect in splenic arteries during the late stages of pregnancy seems to be the escalating increase of the circulating estrogens and progesterone during pregnancy [5]. The elevation of the levels of these hormones has been associated with promotion of various structural alterations in the arteries, such as the disruption of the internal elastic lamina, fragmentation of elastic fibers, degeneration of smooth muscle fibers, and failure of elastin formation. Additionally, it appears that the elevated levels of relaxin throughout the third trimester of pregnancy may affect the elasticity of the splenic artery wall [3,6,7]. Especially in case of multiparity, the repeated exposure to these hormonal shifting could explain the increased incidence of rupture of SAA in this group of pregnant women. It is also assumed that hemodynamic changes which occur during the late stages of pregnancy are implicated in the etiology of SAA ruptures during this period. More specifically, due to the fact that the increased size of the uterus tends to compress the aorta and the iliac arteries, resulting in higher flow in the splenic artery, the development of the SAA is enhanced; moreover, the increases of blood volume and cardiac output, along with the relative portal congestion, can definitely contribute to the formation of SAAs [3].
In terms of clinical manifestations, the rupture of SAA is undoubtedly presented as an acute abdomen, with localization of pain more frequently in the epigastrium or the left hypochondrium, accompanied by vomiting and derangement of the vital signs, compatible with developing hemodynamic shock. There are no physical signs that reliably indicate the presence of an SAA. In the early stages of rupture, diffuse tenderness in the upper abdomen or over the uterine fundus may be elicited. In severe cases, and with significant blood loss, signs of peritoneal irritation, hypotension, and shock are present.
The physical course of the rupture of SAA can either consist of one stage, leading to dramatic collapse as a result of inability of self-containment of bleeding, or it can present in a two-stage sequence, when hemorrhage would be initially tamponated in the lesser sac by clots blocking the foramen of Winslow [8]. Even in the latter case, when the physician may have an advantage in terms of time availability, the gradual increase of pressure in the lesser sac would be suddenly followed by a rupture into the greater sac and lead to massive intra peritoneal bleeding. Rupture of SAA in pregnancy is difficult to diagnose because it shares signs and symptoms with other condition such as placental abruption, uterine rupture, perforate dulcer, or rupture of other arterial aneurysms. Often the diagnosis is made only at surgery In a suspected unruptured SAA the gold standard for diagnosis is arteriography, although ultra sonography and pulsed Doppler are preferable in pregnancy. Computed tomography is also useful. When a patient with a ruptured SAA has acute abdominal pain, an emergency ultra sound scan may reveal free fluid in the upper abdomen, and the diagnosis is subsequently confirmed at laparotomy. More common obstetric differential diagnostic considerations that should always be monitored among pregnant women are uterine rupture, placental abruption, amniotic fluid embolism, and ruptured ectopic pregnancy [9-11].
The diagnosis of splenic artery aneurysm can be made by Ultrasound, pulsed Doppler, CT, MRI and abdominal aortic arteriography, which is the gold standard [12]. It is reported that up to 74-87% of the aneurysms are located in the distal third ofthe splenic artery, 22% in the middle third and the remaining in the proximal third [13] Indications of treatment include symptoms, aneurysms >2cm, pregnancy and patients having major upper abdominal surgery [14]. Surgical options includes; excision, ligation or revascularization, with or without splenectomy. This could be achieved by either an open or a minimally invasive approach depending on the expertise [15] the endovascular treatment is usually considered for those who are not candidate for surgery and those in elective settings. It includes different techniques such as coil embolization, placement of covered stents, plug deployment, gluing, and injection of endoluminal thrombin, polyvinyl alcohol, particles, or gelfoam. However, surgical intervention is considered the conventional option of treatment in most centers especially in case of rupture [1].
Conclusion
Splenic artery aneurysm rupture is a challenging diagnosis that needs to be considered in any peripartum collapse, which carries high mortality rate reaching up to 70%, in which immediate intervention is crucial and will prevent maternal death, which is a catastrophe.
Acknowledgement
We expressed our special thanks to Dr. Amin, Dr. Doaa' from Anesthesia department, blood bank, operation theater, intensive care unit teams and Latifa hospital's staff for their appreciated effort in case management.
References
- Habbal AY, Christophi C, Muralidharan V (2010) Aneurysms of the splenic artery - a review. Surg J R Coll Surg EdinbIrel 8(4): 223-231.
- Abdulrahman A, Shabkah A, Hassanain M, Aljiffry M (2014) Ruptured spontaneous splenic artery aneurysm: A case report and review of the literature. Int J Surg Case Rep 5(10): 754-757.
- Parangi S, Levine D, Henry A, Isakovich N, Pories S (2007) "Surgical gastrointestinal disorders during pregnancy,” American Journal of Surgery vol 193(2): 223-232.
- Lang W, Strobel D, Beinder E, Raab M (2002) "Surgery of a splenic artery aneurysm during pregnancy,” European Journal of Obstetrics Gynecology and Reproductive Biology 102 (2): 215-216.
- Abbas MA, Stone WM, Fowl RJ, Gloviczki P, Oldenburg WA, et al. (2002) "Splenic artery aneurysms: two decades experience at Mayo Clinic,” Annals of Vascular Surgery 16(4): 442-449.
- Dave SP, Reis ED, Hossain A, Taub PJ, Kerstein MD, et al (2000) "Splenic artery aneurysm in the 1990s,” Annals of Vascular Surgery 14(3): 223229.
- Groussolles M, Merveille M, Alacoque X, Vayssiere C, Reme JM, et al, (2011) "Rupture of a splenic artery aneurysm in the first trimester of pregnancy,” Journal of Emergency Medicine41(1): e13-16.
- Chookun J, Bounes V, Ducasse JL, Fourcade O (2009) "Rupture of splenic artery aneurysm during early pregnancy: a rare and catastrophic event,” American Journal of Emergency Medicine 27(7): 898.
- Nincheri Kunz M, Pantalone D, Borri A, Paolucci R, Pernice LM, et al. (2003) "Management of true splenic artery aneurysms. Two case reports and review of the literature,” Minerva Chirurgica 58(2): 247256.
- Henrich W, Surbek D, Kainer F, Grottke O, Hopp H, et al. (2008) Diagnosis and treatment of peripartum bleeding. J PerinatMed 36 (6): 467-478.
- Ha JF, Phillips M, Faulkner K (2009) Splenic artery aneurysm rupture in pregnancy. Eur J Obstet Gynecol Reprod Biol 146(2): 133-137.
- Ousadden A, Ibnmajdoub KH, Elbouhaddouti H, Mazaz K, Aittaleb K, et al. (2009) Intragastric rupture of a splenic artery aneurysm - a case report. Cases J 2: 202.
- Yadav R, Tiwari MK, Mathur RM, Verma AK (2009) Unusually giant splenic artery and vein aneurysm with arteriovenous fistula with hypersplenism in a nulliparous woman. Interact Cardiovasc Thorac Surg 8(3): 384-386.
- Cordova AC, Sumpio BE (2013) Visceral artery aneurysms and pseudo aneurysms-should they all be managed by endovascular techniques? Ann Vasc Dis 6(4): 687-693.
- Kim Y, Johna S (2013) Laparoscopic excision of splenic artery aneurysm. J SocLaparoendoscSurg/SocLaparoendoscSurg: JSLS 17(1):132-134.






























