SRH and HIV/AIDS Interventions in Higher Education Institutions
Zekariyas Sahile1, Abenezer Yared2*, Mulugeta Mekuria1 and Bekele Tassew3
1Department of Public Health Officer, Ambo University, Ethiopia
2Department of Sociology, Ambo University, Ethiopia
3Department of Cooperatives, Ambo University, Ethiopia
Submission: April 10, 2017; Published: May 24, 2017
*Corresponding author: Abenezer Yared, Department of Sociology, Ambo University, Ethiopia, Email: abeneither@gmail.com
How to cite this article: Zekariyas S, Abenezer Y, Mulugeta M, Bekele T. SRH and HIV/AIDS Interventions in Higher Education Institutions : Lessons from Ambo University, Oromia, Ethiopia. Glob J Reprod Med. 2017; 1(1): 555559. DOI: 10.19080/GJORM.2017.01.555559
Abstract
Background: Most of the students in higher education institutions are young, aged 19-24, who are often sexually active, and among the most vulnerable and at risk of HIV infection and other sexual and reproductive health problems. Taking this in to account HIV/AIDS and SRH intervention has been taking place in Ambo University. With the expectation that it will help the program manager to improve the intervention, this study was aimed to monitor the intervention of HIV/AIDS and SRH program in the University.
Methods: A qualitative study using in-depth interview and document review were used to collect primary and secondary data, respectively. A total of 13 study participants constituting the university's HIV/AIDS prevention and control office focal person, campus clinic officer, guidance and counseling officer and 10 students from different departments were purposely selected for the in-depth interview. The interviews were audio-taped digitally, transcribed verbatim, and thematically analyzed. Two years' retrospective document was reviewed to investigate the level of HIV/AIDS and SRH intervention in the university. Ethical approval and verbal consent were obtained before data collection.
Results: Findings of the study indicated that structural, behavioral and biomedical interventions were implemented in the university's main campus. Services like condom promotion and provision and HIV counseling and testing were accessible to students. On the other hand, guidance and counseling, youth dialog or conversation, STI prevention, diagnosis and treatment, male circumcision promotion for HIV/STI prevention, and unwanted pregnancy prevention and comprehensive abortion care were unavailable.
Conclusion: Although structural, behavioral and biomedical interventions existed in the campus, each component of the intervention was not implemented in accordance with the full package of the service. Therefore, program staff, managers and partners should give emphasis to the mobilization of resources as well as trainings geared toward improving HIV/AIDS and SRH interventions in Ambo University.
Keywords: SRH; HIV/AIDS; Intervention; HEIs; Ethiopia
Background
HIV infection in Ethiopia was recognized in early 1980s with the first AIDS cases reported in 1986 and became one of the major public health as well as developmental problem in the country since the mid 1980 [1,2]. The number of Higher Education Institutions (HEIs) in Ethiopia has been dramatically increasing in the past ten years. In 2010/11, the total enrolment (undergraduate and postgraduate) of the HEIs in all programs (regular, evening, summer and distance) was 467,843 [3]. Most of the students in HEIs were young, aged between 19 and 24, who are often sexually active, and among the most vulnerable and at risk of HIV infection and other Sexual and Reproductive Health (SRH) problems [4].
Previously, researches have shown that students' SRH needs received little attention in HEIs. Even the available SRH care was not youth friendly to and known by many students [5]. Current trends, however, show that the HEIs are making the necessary efforts to working toward expanding and consolidating their interventions and programs in a systematic and workable ways. This has contributed a lot in reducing new infections and addressing SRH needs of students. However, programs and interventions within many HEIs and among partners are not coordinated and complementary, and programs' effectiveness has not routinely been monitored and evaluated [1,5]. Hence, this study aimed to investigate the availability and level of HIV/ AIDS and SRH intervention implementation in Ambo University (AU), Oromia, Ethiopia .[6]
Methods
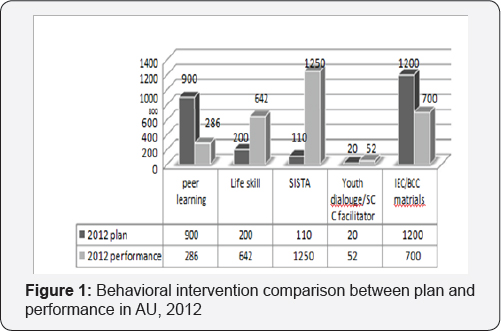
With the aim of monitoring HIV/AIDS and SRH intervention in Ambo University, in-depth interview and document review were carried out to collect primary and secondary data, respectively Two years' (from 2011/12 to 2012/13) retrospective document was reviewed to identify the availability and the level of HIV/ AIDS and SRH intervention implementation using checklist. Higher education strategic plan and minimum package of HIV/ AIDS and SRH prevention were used as a standard to compare the performance and to check available services. Furthermore, the performance level is discussed by comparing performances with planned activities. A total of 13 study participants constituting the university's HIV/AIDS Prevention and Control Office (HAPCO) focal person, campus clinic officer, guidance and counseling officer and ten students (four female and six male) from different year and fields of study were purposely selected for in-depth interview. Ethical approval and verbal consent were obtained before data collection. In preparing the qualitative data for analysis, all digitally audio-taped interviews which were conducted in Amharic were translated into English and transcribed verbatim, producing over sixty pages of transcripts. After data transcription, categorization and reduction, the in-depth interview generated qualitative data was analyzed thematically. Quotes illustrating rich information were retrieved from coded data to support the data analysis and illustrate major themes Figure 1.
Result
Behavioral intervention
The document review showed that except Modeling and Reinforcements to Combat HIV/AIDS (MARCH), all behavioral component interventions were implemented in AU. As to the depth interview of HIV/AIDS coordinator, "MARCH is not implemented in this university because training and manual were not provided so far.” He also added that he was aware "other universities like Addis Ababa University perform MARCH but not here in AU yet.” The document review showed that there was no annual plan document for 2011 while activity report for the same year was available. For the year 2012, however, both plan and recorded document were found. The following subsections discuss the implementation status of the components of the behavioral interventionTable 1.
Peer learning: In 2011, a total of 230 students were trained on peer education, of which 50 of them were trained as facilitator and 180 of student were trained in peer learning education by cascading. In 2012, the university was planned to train 900 students on peer education, but only 280 (31.1%) of them were trained, of which 26 (12.1%) of them were trained as a facilitator and 260 (87.9%) of them were trained by cascading. Through in-depth interview, the university HIV/AIDS focal person explained that: "Even though peer learning intervention was implemented well in 2012, it is still a major challenge because its manual is not up to the standard as it is not designed to fit the level and needs of students in HEls.” However, the indepth interview with students showed that junior students did not even know the existence of peer learning in the campus. A female English language and literature student in this category even wondered and questioned back, "is it available here at all?!” On the other hand, senior participants of the interview knew and have participated in peer learning, albeit in a limited manner. A second year male civics and ethical studies supported that the coverage of peer learning in the main campus was inadequate when he said, "I have taken training, but it is difficult to say that it exists widely” Figure 2.
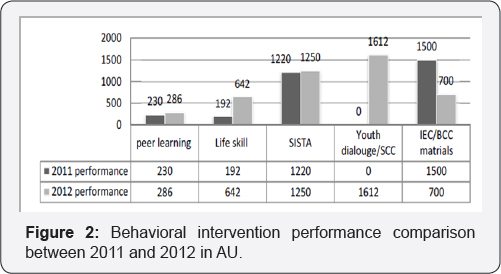
SISTA: Sisters Informing Sisters about Topics on HIV/AIDS (SISTA) is the other behavioral intervention that was implemented for the two years. In 2012, it was planned to train 1,100 students through SISTA program and 1,250 female students were trained.Among these, 50 of them were trained as facilitator and 120 of them were trained by cascading. When compared to the performance of 2011, the number of female students trained by SISTA cascading was lower but the number of facilitators trained was higher. In 2011, a total of 1,220 of students were trained, of which 1,145 were reached by cascading and 75 of them were trained as facilitators. In this regard, the focal person disclosed that "there was an assigned SISTA coordinator previously but there is none currently” and added that "SISTA was established but not functioning.”
In line with this and acknowledging its multidimensional benefits that range from self-confidence and independence in interactions to protection of oneself from STDS including HIV/AIDS and other SRH problems and complications, female student respondents confirmed SISTA was operational in the main campus. Although these interviewees also reported that SISTA ceased to exist currently and that it had limited coverage, an anti-HIV/AIDS club member and SISTA participant female student said, "SISTA used to provide trainings on HIV and STDs, although these services did not reach each female student.”
Life skill training: Two hundred life skill and sex education was planned in 2012 and 642 students were trained in life skill education. Of the total trained, 107 of them were trained as facilitators and 535 of them were trained in life skill and sex education by cascading. Compared to 2011, this is higher performance in both training of facilitators and those trained by cascading, as only 32 and 160, respectively were trained in 2011. Similarly, the focal person confirmed that "this intervention component was the well-organized one in 2012.” Students who took part in the qualitative interview said that life skill training was given, but only to some group of students. For instance, a fourth year female interviewee from the school of law said: "Life skill training is provided. But, it is only to those of us who are members of clubs that these trainings are repeatedly given. I, for example, have taken all the three trainings mentioned so far: Peer learning, SISTA and life skill training.”
Guidance and counseling: According to the guidance and counseling officer, counseling was provided to students on problems related to depression, insomnia, stress, homesickness, romantic relationships, HIV/AIDS and SRH. The officer reported that, in 2012, 11 students with such problems benefited from these services and 3 students "who could not pursue their study in AU due to family and economic problems were transferred to other universities of their preference.” Telling that she started working as guidance and counseling officer in the university in 2012, the officer revealed that there was no document and plan handed over to her from the year 2011. Neither was a full-fledged plan for the year 2012. The officer further added, "although the office planned to have a billboard and additional human resource by the year 2012, these are not accomplished yet.” According to the guidance and counseling officer, her office works in collaboration with the campus clinic. She claimed that the clinic sent students with various psychosocial problems to the office. Despite the above effort by guidance and counseling center, none of the student interviewees reported the availability of guidance and counseling in AU main campus. It was also disclosed that there was no linkage between HAPCO and the guidance and counseling center
Youth dialogue (community conversation): Regarding school community conversation, in 2012, though it was planned to train only 20 students as facilitators, 52 were trained and 1,560 were trained by cascading. However, there was no activity in this regard in 2011. The coordinator explained by stating that "there is no manual for the implementation of youth dialogue or community conversation.” Similar to guidance and counseling, none of the student interviewees reported the existence of youth dialog or conversation as a means of addressing SRH issues among students of AU main campus.
IEC/BCC: The University had a plan of disseminating 1,200 printed HIV/AIDS IEC/BCC materials (brochures, banners, posters and bill board) by the year 2012 and practically distributed 700 materials. This was lower performance when compared to the total of 15,000 IEC/BCC materials distributed in 2011. Generally, under the behavioral component of the SRH intervention, except for the dissemination of IEC/BCC materials, all other activities like peer learning, life skill and sex education, SISTA, and school community conversation showed a slight progress.
Biomedical intervention
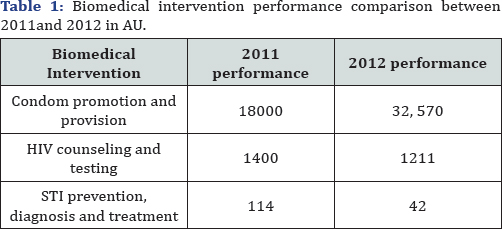
Under biomedical intervention the reviewed document showed that condom promotion and provision, HIV counseling and testing service, sexually transmitted infection diagnosis and treatment service and referring and facilitating timely entry to pre-ART and ART services were among the services implemented in AU. However, referring and facilitating voluntary medical male circumcision and provision of family planning and comprehensive abortion care were services that were unavailable. Details are presented under the subsections below.
Condom promotion and provision: Condom promotion and provision campaigns were undertaken twice in 2011 and three times in 2012. Even though 8 condom outlets were availed in 2011, only 2 were functional at the time of the assessment. A total of 18,000 and 32,570 condoms were distributed in 2011 and 2012, respectively Higher number of condom promotion and provision was made in the year 2012 as compared to 2011. The focal person asserted that "promotion was made on consistent and proper utilization of condom using model penis.” In practice, however, in-depth interview with the clinic officer revealed that there was inappropriate utilization of condom even if large proportion of condoms were distributed. He reported, "we see a lot of condoms on the road which were not utilized and the condom outlets are damaged by students.” All students acknowledged the availability and accessibility of condom provision service. According to the interviewees, condoms can especially be accessed at the campus clinic and some other centers. For example, a first year electrical engineering student indicated that "condom is provided for free at the campus clinic and at the HIV/AIDS center at the main gate of the campus.”
HIV Counseling and Testing (HCT): In the years 2011 and 2012 the university conducted 3 HCT campaigns. A total of 1,400 and 1,211 students in 2011 and 2012, respectively obtained the service. The HAPCO focal person indicated that "shortage of kit is the reason for not conducting more HCT campaigns” This might be the reason for the decline in HCT in 2012 as compared to 2011. All student interviewees reported that HIV testing service was provided in the campus. Not sure of the associated counseling, they reported HIV testing can be acquired from the service rendered as a campaign. The respondents uncovered that HIV testing service in the main campus was irregular and occasional. In this regard, a first year male interviewee from the department of electrical engineering stated, "since I came here (AU), I think it is once that I heard about HIV testing as a campaign.” A fourth year respondent similarly revealed that "HIV testing is rarely made once in a while. For example, I am a fourth year student but it was only twice that there were programs to make students get tested for HIV.” Admitting that HIV testing programs felt behind schedule, a fourth year male interviewee compromised, "I think the test campaign is said to be held every three months in our strategy, but it is often undertaken within every four months in our campus.”
STI prevention, diagnosis and treatment: In the year 2011,a total of 114 students and in the year 2012, 42 students who had STDs were treated in AU. Only one person from campus clinic was trained in syndromic STI case management. However, none of the student in-depth interviewees were able to tell the availability of services geared towards STI prevention, diagnosis and treatment in AU.
Voluntary medical male circumcision: This activity was not performed at all in campus clinic. According to the clinic health care provider "it is not conducted here because training was not given on this issue.” Similarly, all student interviewees reported that they have heard nothing about the promotion of male circumcision in HIV/STI prevention. For instance, a first year female English language and literature student, surprised by the question itself, quested whether it is for youths. Recognizing that uncircumcised males have increased exposure to HIV/AIDS, a second year male civics and ethical studies student interviewee also responded, "I have not heard about it and I know nothing whether or not it is promoted.”
Family planning and comprehensive abortion care: According to the clinic focal person "the demand for HCG test and emergency contraceptive by female students is increasing from day to day.” However, there was no contraceptive method in the university clinic, except condom. In the year 2011, out of 21 students tested, 6 were positive for pregnancy test and in 2012, 21 out of 47 had pregnancy test positive. Responses of in-depth interview participant students similarly revealed that there were no contraceptive methods (such as pills, emergency contraceptives, etc.). Comprehensive abortion care in the campus was no exception to the interviewees' position regarding the unavailability of services and efforts to address SRH problems in the university. Analysis of the in-depth interview revealed that there was no evidence to ascertain the accessibility of comprehensive abortion care for female students of the campus in need of the service.
Structural intervention
SRH and HIV/AIDS Mainstreaming: According to the HAPCO focal person "there was neither standardized separate course manual nor SRH and HIV/AIDS-integrated curriculum, except for the medical and health sciences.” He added that "there was no training given for academic staff on HIV/AIDS curriculum development and integration.” But as per the strategic plan for intensifying HIV/AIDS response at higher education institution in Ethiopia recommended that all higher education institutions should develop at least one standardized alone course manual and integrate HIV/AIDS in the existing curriculum. According to the coordinator there was "no orientation and clear guidelines are there on integration of HIV/AIDS and SRH issues in the curriculum.”
Capacity building: To build the capacity of the university in the implementation of HIV/AIDS programs, one HIV/AIDS program coordinator was available during assessment and one ARC and three clubs called anti HIV/AIDS, SISTA and art clubs were established. However, according to the focal person "the established clubs were not strengthened."
Addressing gender inequalities: According to the strategic plan, all HEIs should develop one code of conduct on Gender Based Violence (GBV) and at least 6 advocacy sessions should be conducted. The university had anti-sexual harassment policy or code of conduct. In addressing gender inequalities issues, two sessions of awareness creation were conducted in the years 2011 and 2012.
Conclusion
All behavioral intervention performances showed improvement in AU, except IEC/BCC distribution. Modeling and reinforcement was not totally implemented. There was poor linkage of HAPCO office with guidance and counseling service center. Also, unavailability of recorded plan and performance document was revealed. According to the in-depth interview with students, except for condom promotion and provision and HIV counseling and testing at the campus clinic, students denied the existence of other SRH intervention services including guidance and counseling, youth dialog or conversation, STI prevention and treatment, male circumcision promotion, unwanted pregnancy prevention and comprehensive abortion care at AU. However, senior students additionally knew and participated in peer learning, SISTA, and life skill training. Moreover, these interviewees also explained that art club and anti-HIV/AIDS club 0077ere operational in the effort directed towards preventing HIV/AIDS in AU.
On biomedical intervention, there was no service of contraceptive methods, except condom promotion and provision, comprehensive abortion care and promotion of male circumcision. However, from record review and survey result indicate students suffer from unwanted pregnancy and abortion. Large number of condom was distributed in the year of 2012 as compared to 2011. All the activities under structural component of the intervention were implemented but each activity was not implemented in accordance with the strategic plan.
In order to improve effectiveness and efficiency of SRH and HIV/AIDS intervention, program staffs and managers should mobilize HIV/AIDS and SRH intervention packages continually, harmonize and align plan and report, avail services like MARCH, contraceptive method, comprehensive abortion care and referral linkage, strengthen HCT service, and keep up the promotion and provision of condom and avail additional condom outlets.
References
- Lester FT, Ayehunie S, Zewudie D (1988) Acquired immunodeficiency syndrome: seven cases in an Addis Ababa hospital. Ethiop Med J 26(3): 139-145.
- HAPCO & World Bank (2008) HIV/AIDS in Ethiopia: an epidemiological synthesis.
- Education Management Information System (2010) Education Statistics Annual Abstract. p. 56.
- Ministry of Education and UNESCO (2012) Education sector response to HIV and AIDS: Learning from good practices in Ethiopia.
- Higher Education Institutions' Partnership Sub-Forum against HIV/ AIDS in Ethiopia (2013) HIV/AIDS and sexual reproductive health intervention package. Higher education institutions in Ethiopia.






























