How Much Inconvenience and Discomfort does Modern IVF Treatment Cause?
James Esposito1,2, Sharon Qin1,2 and Gab Kovacs2,3*
1University of Melbourne, Australia
2Epworth Healthcare, Australia
3Department of O & G, Monash University Clayton, Australia
Submission: March 15, 2017; Published: May 05, 2017
*Corresponding author: Kovacs G, Department of O & G, Monash University Clayton, Epworth Health care, Australia, Tel: + (61)409-632-753; Fax: +(61)39-890-1866; Email: gkovacs@monashivf.com
How to cite this article: Sharon QIN, James ESPOSITO, Cheers G. How Much Inconvenience and Discomfort does Modern IVF Treatment Cause?. Glob J Reprod Med. 2017; 1(2): 555557. DOI: 10.19080/GJORM.2017.01.555557
Abstract
IVF is widely practiced, however, data on the degree of discomfort and inconvenience experienced by women undergoing treatment is nonexistent. We surveyed women being treated at Monash IVF, undergoing oocyte collection in stimulated cycles at Epworth Hawthorn Day Surgery. One hundred and eighteen women were recruited to the study during a five week period from August to September 2014 and underwent a five minute telephone interview asking ten questions. Women were asked to rate the inconvenience and pain associated with the blood tests, injections and oocyte collection procedure using a numeric rating scale of zero to ten. Data on analgesic usage and the time taken to return to work and normal activity was also recorded. The median number of oocytes was nine. The mean pain score immediately post operation was 4.6, and at 24 hours 3.9, on a scale of 1 to 10. Most women returned to normal activity and work within two days (mean 1.7, SD1.5days and mean 1.8 SD1.5 respectively).Immediate post operative discomfort was not found to be correlated with the number of oocytes collected. However the number of oocytes collected positively correlated with the quantity and duration of analgesics consumed and the time taken to resume work and normal activity.
Keywords: IVF-oocyte collection-discomfort-convalescnece
Lay of Summary: The women were all patients of Monash IVF, undertaking stimulated cycle IVF with oocyte collection at Epworth Hawthorn Day Surgery. They were surveyed to assess the amount of inconvenience and discomfort they experienced. During the pre-operative consultation, permission was obtained for follow up contact. The information was obtained by a telephone survey, seven days post operation. The study was completed during a five week period from August to September 2014, and all 142 women undergoing oocyte collection were requested to partake in the study, with 118 (83%) women completing the survey. The median number of eggs collected was nine. The mean pain score immediately post operation was 4.6, and at 24 hours 3.9, on a scale of 1 to 10. Immediate postoperative pain correlated with the ongoing discomfort and analgesic use. Most women returned to normal activity and work within two days (mean 1.7, SD 1.5 days and mean 1.8 SD 1.5 respectively). The amount of post operative discomfort was not related to, the number of eggs collected, but it did correlate with the quantity and duration of analgesics consumed, and with the time taken to resume work and normal activity.
Introduction
IVF has become a common procedure, with more than 3% of babies born in Australia being conceived by this technique. However, data on the degree of discomfort and inconvenience experienced by women undergoing treatment is nonexistent [1].
Materials and Methods
The women were all patients of Monash IVF, undertaking oocyte collection at Epworth Hawthorn Day Surgery. During a five week period from August to September 2014, all 142 women undergoing oocyte collection (VPU) in stimulated cycles were recruited to the study. Just prior to undergoing oocyte collection they were asked to partake in a post operative telephone survey one week after the oocyte collection. One ofthe researchers (JE or SQ) attended in theatre with the patient and established rapport. All 142 women undergoing oocyte collection during this period agreed to partake in the study. A five minute telephone interview asking ten questions was undertaken by 118 women (83%).
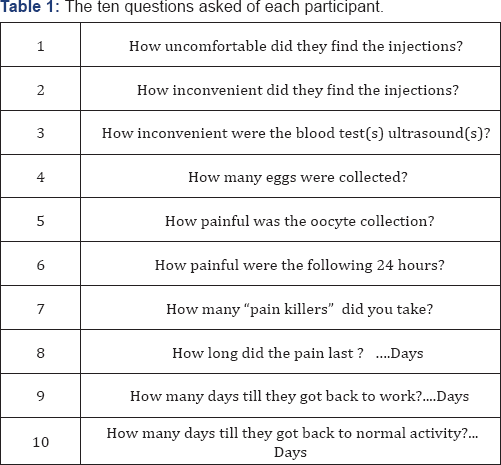
Table 1, the remaining 24 were women were not able to be contacted. The women were questioned about their experience with injections, blood tests, and the oocyte collection. Symptoms were graded on a numeric rating scale of one to ten, where higher numbers reflected worse pain or greater inconvenience. Data on analgesic usage and the time they took to get back to work and normal activity were also recorded. The number of oocytes collected was compared with the degree of inconvenience of injections and blood tests, pain immediately post operatively and later, the amount and type of analgesic use, and the time taken to return to “normal”
All statistical analysis was performed using STATA version 12 (Stata Corp. 2011. Stata Statistical Software: Release 12. College Station, TX: Stata Corp LP). The statistical tests used are described with the relevant results. All P values were two tailed and statistical significance defined as P ≤ 0.05.
Results
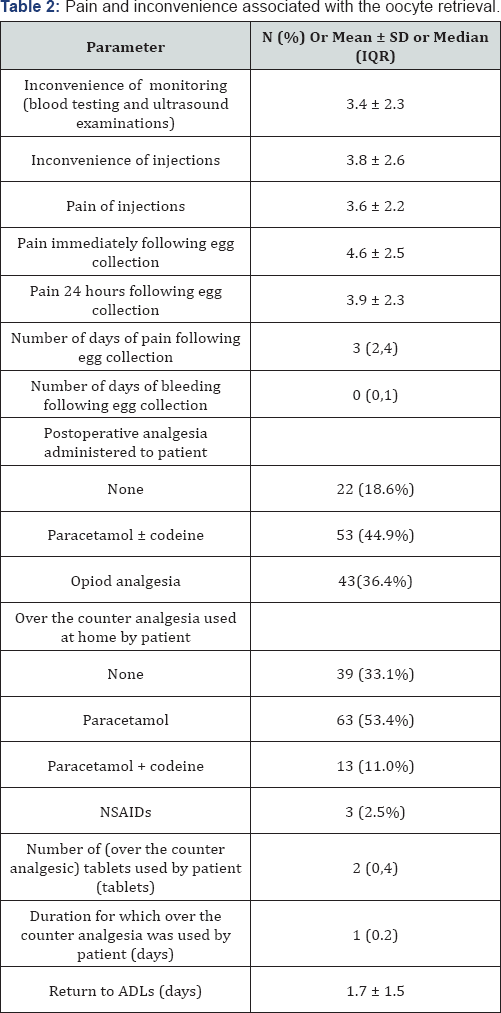
The median number of oocytes collected on this cycle was 9. Embryo transfer was successful in 89 (75.4%). Among women undergoing IVF, 53 (44.9%) were transferred at the blastocysts stage and 36 (30.5%) were transferred at the cleavage stage. The pain and inconvenience associated with the stimulation and oocyte retrieval is summarized in Table 2. The inconvenience of blood and ultrasound imaging was reported as 3.4±2.3 and the inconvenience associated with the injections was 3.8±2.6. Pain scores for the injections was reported as 3.6±2.2 whilst pain immediately following egg collection was 4.6±2.5 and at 24 hours post procedure was 3.9±2.3. The median number of days for which pain was experienced following oocyte retrieval was 3 and median number of days for which light bleeding was experienced was 0. In terms of postoperative analgesia 39 (33.1%) required none, 63 (53.4%) required simple analgesia (paracetamol with or without codeine) and 43(36.4%) required opiod analgesia (oxycodone or fentanyl). Most women returned to work and normal activity within two days (1.7±1.5 and 1.8±1.5 respectively).
Pair wise correlations were performed between the various variables measured from the telephone interview and pearson correlation coeffients subsequently computed. These results are shown in Table 3. Maternal age correlated negatively with the number of oocytes collected (r = -0.19, p<0.05) and the total days of pain (r = -0.19, p<0.05) Although the number of oocytes collected did not correlate with immediate or delayed pain, nor the duration of pain, it did correlate with the number of over the counter analgesic tablets used (r = 0.20, p<0.05),and the number of days they were used following egg collection (r = 0.21, p<0.05). It also correlated with the return to activities of daily living (r = 0.31, p<0.05) and return to work (r = 0.22, p<0.05).
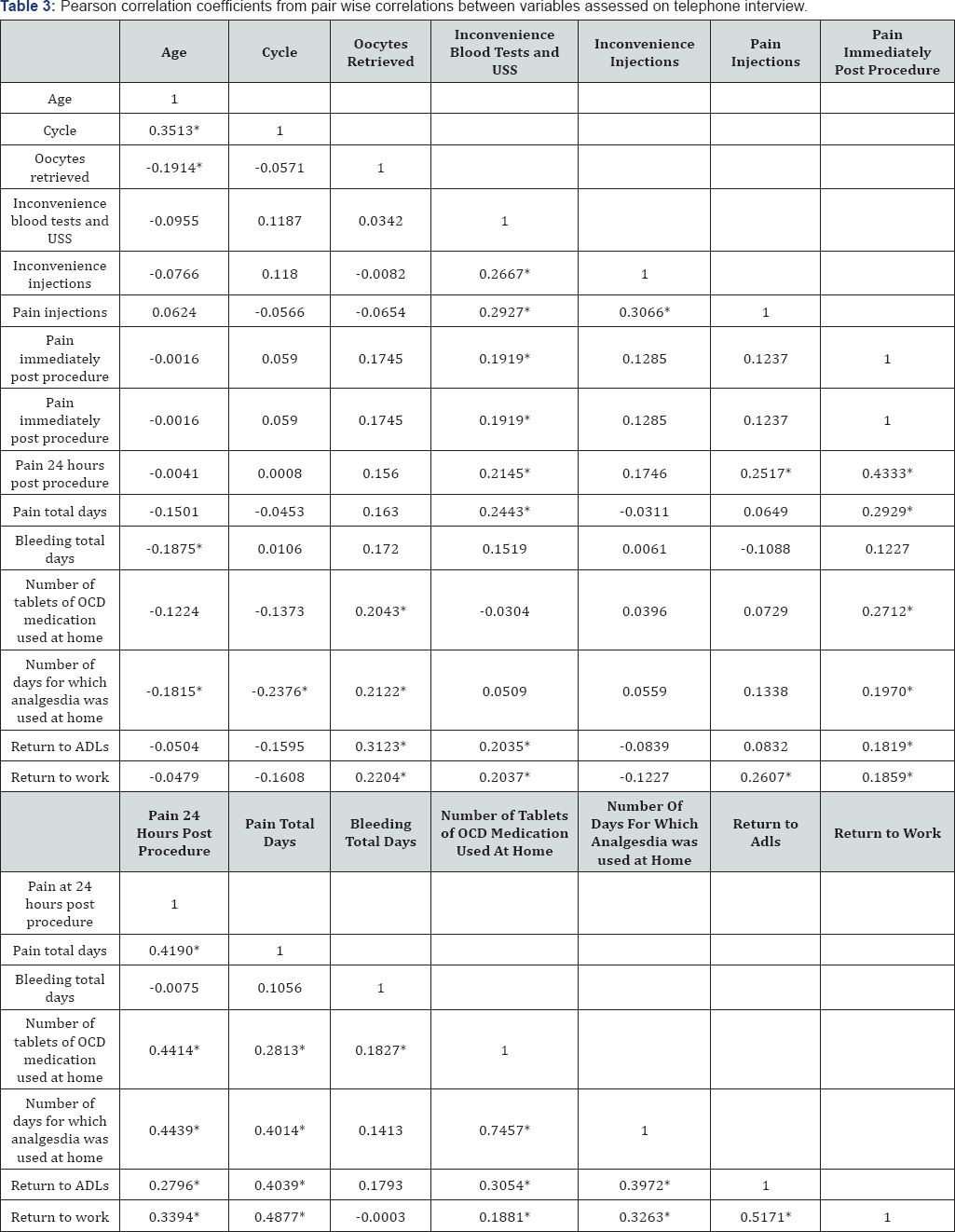
In addition the inconvenience associated with blood and ultrasound testing positively correlated with patients reporting greater levels of inconvenience associated with injections (0.27, p<0.05), greater levels of pain associated with injections (0.29, p<0.05), greater levels of pain immediately after the procedure (0.20, p<0.05), at 24 hours (0.21, p<0.05) and greater number of total days of pain (0.24, p<0.05). Inconvenience of blood and ultrasound testing was also positively correlated with longer periods of time to return to ADLs (0.20, p<0.05) and work (0.20, p<0.05)
A comparison between pain scores and analgesia prescription was also undertaken. We found that ninety-five percent of patients who were given simple analgesia had pain scores between 3.6 and 4.9 immediately after egg collection, whereas 95% of patients who were given opiod analgesia had pain scores between 6.0 and 7.0. Pain at 24 hours following egg collection and total pain duration in days were not different between patients receiving either simple or opioid analgesia.
Discussion
The most important role of the clinician is to set patients realistic expectations about the inconvenience and discomfort of their forthcoming treatment. This study enables clinicians to more accurately provide such information to women undergoing IVF, and in turn will result in greater overall patient satisfaction. The more a patient finds the preoperative blood testing and USS imaging inconvenient, the more likely they are to find the injections inconvenient and the more likely they are to experience more pain (immediately after the procedure, 24 hours after the procedure and total duration of pain in days). These patients also take longer to return to ADLs and work. Patients given opiod analgesia immediately after egg collection were found to take longer to return to ADLs (1.5±1.0, 2.2±1.7, p = 0.019) but did not take longer to return to work.
There is not a lot of information reported in the literature on the discomfort associated with VPU. Ludwig [2] recorded prospectively the complications experienced by over 1000 women who underwent VPU. They reported that although most patients tolerated the OR well, 3% of patients experienced severe to very severe pain, and 2% of patients were still suffering from severe pain two days after the VPU procedure. In contrast to our findings, they reported that the pain level increased with the number of oocytes retrieved. Aaragona [3] reported a 0.06% post operative bleeding rate after VPU, but did not comment on discomfort. Bodri [4] recorded a "severe pain” rate of 2/4052 amongst young ovum donors, but gave no detail of discomfort experienced.
Seyhan [5] compared complication rates and pain scores after oocyte pickup (OPU) in in vitro maturation (IVM) and IVF cycles, and found no difference.The absolute rate of post operative bleeding was 6/288 (2.1%). Six patients reported severe post operative pain, and the mean pain scores were 3.4 for IVF and 3.8 for the IVM group.
This study provides actual real-life treatment experience of a significant group of women undergoing stimulation and oocyte collection for IVF, and records the degree of discomfort experienced. We conclude that the level of pain is reported by women as "mild to moderate” and in the majority of women can be managed with simple, non-opiod analgesia.
References
- Kovacs G (2012) Oocyte Collection. In: Gardner et al. (Eds.), Textbook of Assisted Reproductive Techniques: Clinical Perspectives.
- Ludwig AK, Glawatz M, Griesinger G, Diedrich K, Ludwig M (2006) Perioperative and post-operative complications of transvaginal ultrasound-guided oocyte retrieval: prospective study of >1000 oocyte retrievals. Hum Reprod 21(12): 3235-3240.
- Aragona C, Mohamed MA, Espinola MS, Linari A, Pecorini F, et al. (2011) Clinical complications after transvaginal oocyte retrieval in 7,098 IVF cycles. Fertil Steril 95(1): 293-294.
- Bodri D, Guillen JJ, Polo A, Trullenque M, Esteve C, et al. (2008) Complications related to ovarian stimulation and oocyte retrieval in 4052 oocyte donor cycles. Reprod Biomed Online 17(2): 237-243.
- Seyhan A, Ata B, Son WY, Dahan MH, Tan SL (2014) Comparison of complication rates and pain scores after transvaginal ultrasound- guided oocyte pickup procedures for in vitro maturation and in vitro fertilization cycles. Fertil Steril 101(3): 705-709.





