Balloon Sinuplasty Literature Review: An Assessment of Clinical Studies from 2007 To 2018
Rohan Dsouza1, Jagdish Chaturvedi2*, Pooja Kadambi3, Abu Saquib Tauheed1, Ravi Jangir1, Darien Rodrigues1, Rishabh Sirdesai1 and Parul Chachra1
1Affordable Invention in MedTech (AIM) Fellow, InnAccel Technologies Pvt Ltd, s, India
2ENT Consultant, Fortis Hospital, Bangalore, India
3Lead System Designer, InnAccel Technologies Pvt Ltd, India
Submission: March 21, 2018; Published: April 26, 2018
*Corresponding author: : Jagdish Chaturvedi, Department of Otorhinolaryngology, Fortis Hospital, Bannerghatta road, Bangalore- 560 076, Tel: +91-9650928582; Email: dr.jagdishc@ymail.com
How to cite this article: Rohan D, Jagdish C, Pooja K, A Saquib T, Ravi J et al. Balloon Sinuplasty Literature Review: An Assessment of Clinical Studies from 2007 To 2018. Glob J Otolaryngol 2018; 15(1): 555905. DOI: 10.19080/GJO.2018.15.555905
Abstract
Chronic Rhinosinusitis (CRS) is a disease said to affect 1 in 7 people across the globe. It is associated with debilitating symptoms that have a significant impact economically as well as on the patient's quality of life. It results when the nasal passages and paranasal sinuses are afflicted by concurrent inflammation and infection. Currently the two key options in management include long term medical management and functional endoscopic sinus surgery (FESS). The failure rate of medical treatment ranges from 50-88% in literature, following which patients undergo endoscopic sinus surgery. FESS involves the removal of mucosal and osteoid tissue to achieve adequate disease clearance. In keeping with the principle of regaining physiological nasal clearance and ventilation, balloon sinuplasty was approved in 2005, which dilates the ostia of the diseased sinuses, allows for mucous clearance and improves ventilation. In a survey based study looking at the factors leading to delay in definitive management in patients with Chronic Rhinosinusitis in India it was concluded that there is a need for an affordable, minimally invasive solution for CRS soon after medical management fails. Balloon sinuplasty or balloon catheter dilation (BCD) is a relatively novel procedure would be a suitable option to bridge this gap. This article is a review of literature on the efficacy and safety of balloon dilation as a standalone procedure, in comparison with FESS or as a hybrid procedure with balloon sinuplasty being conducted along with FESS.
Keywords: Chronic sinusitis; Rhinosinusitis; Balloon sinuplasty; Balloon dilation; Endoscopic sinus surgery
Abbreviations: BCD: Balloon Catheter dilation; FESS: Functional endoscopic sinus surgery; CRS: Chronic Rhinosinusitis; SNOT-20: Sinonasal Outcome Test-20; SNOT-22: Sinonasal Outcome Test
Introduction
Chronic Rhinosinusitis (CRS) is defined as inflammation of the nose and paranasal sinuses for more than 12 weeks and is said to affect 1 in 7 people in the developed world with a significant economic impact coupled with a substantial impact on the quality of life [1-3]. CRS is one of the most prevalent chronic diseases worldwide with various studies reporting an affliction of 5-15% in some studies and 16% of the adult population in others and this disease has similar prevalence rates in India as well. Currently there are two key options in management, long term medical management and functional endoscopic sinus surgery (FESS) [4-8]. The failure rate of medical treatment ranges from 50-88% in various studies, following which patients undergo endoscopic sinus surgery. FESS, although functional, leads to the removal of mucosal and osteoid tissue to achieve clearance of inflamed disease tissue [3,9].
Pseudo stratified, ciliated, columnar epithelial mucosas line the nasal cavities and paranasal sinuses. These cilia trap microbes and foreign particles and through a defined mucociliary clearance path and clear them in to the nasopharynx. The 'osteomeatal complex' laterals to the middle turbinate does a common outflow tract for the maxillary, frontal and anterior ethmoid sinuses comprise the uncinate process which guards the ethmoid infundibulum. The pathogenesis of this disease is unclear but is multi factorial, involving infections, mucosal inflammation and impaired mucociliary clearances [10]. A model proposed by Timperley comprises interplay of these factors leading to a positive feedback spiral [11,12]. The treatment of CRS begins with medical management and entails a prolonged course of various combinations of topical nasal steroids, saline sprays, antibiotics, antihistamines and systemic steroids [13]. Most patients with CRS are initiated on medical therapy but the success of medical therapy is unclear in literature with reports ranging from 50% to 88% [14].
Functional endoscopic sinus surgery is reserved for those in whom medical management has failed or in cases with complications. FESS serves to open up the sinus drainage pathways, enhancing mucosal clearance. The word 'functional' emphasises the preservation of normal mucosal clearance via the natural anatomic drainage pathways [10]. Balloon Sinuplasty is a relatively new intervention in the management of chronic rhinosinusitis pivoting on the success in other surgical fields in using minimally invasive balloon dilation technology. Lanza first described this concept in 1993 and in 2005 it was approved by the US Food and Drug Administration as a minimally invasive treatment alternative for the chronic Rhinosinusitis [15-17]. Balloon sinuplasty either works on Seldinger's technique of advancement over a guide wire or direct visual confirmation technique to advance the balloon in to the ostium. Once it is positioned in the ostium a high pressure balloon is inflated to a pressure up to 12 atmospheres.
The compression of tissue along the inner circumference of the ostium causes micro fractures, thus dilating the ostium to 4-7mm without any tissue or bone excision. In doing so BCD aims to restore the physiological sinus drainage without changes to the nasal anatomy. Thus far there has been considerable scepticism in accepting this technique due to the supposed lack of global literature as well as the high cost. One of the key push backs from surgeons in the adoption of the procedure was the lack of controlled prospective studies, especially in comparison with FESS [18,19]. However, since approval there have been multiple controlled trials and meta-analyses with standalone balloon dilation, balloon sinuplasty vs FESS as well as hybrid procedures (Balloon dilation along with FESS) vs traditional endoscopic sinus surgery [20]. This editorial looks to explore the publications in the balloon sinuplasty in scientific literature looking at surgical outcomes as well as patient outcomes.
Material and Methods
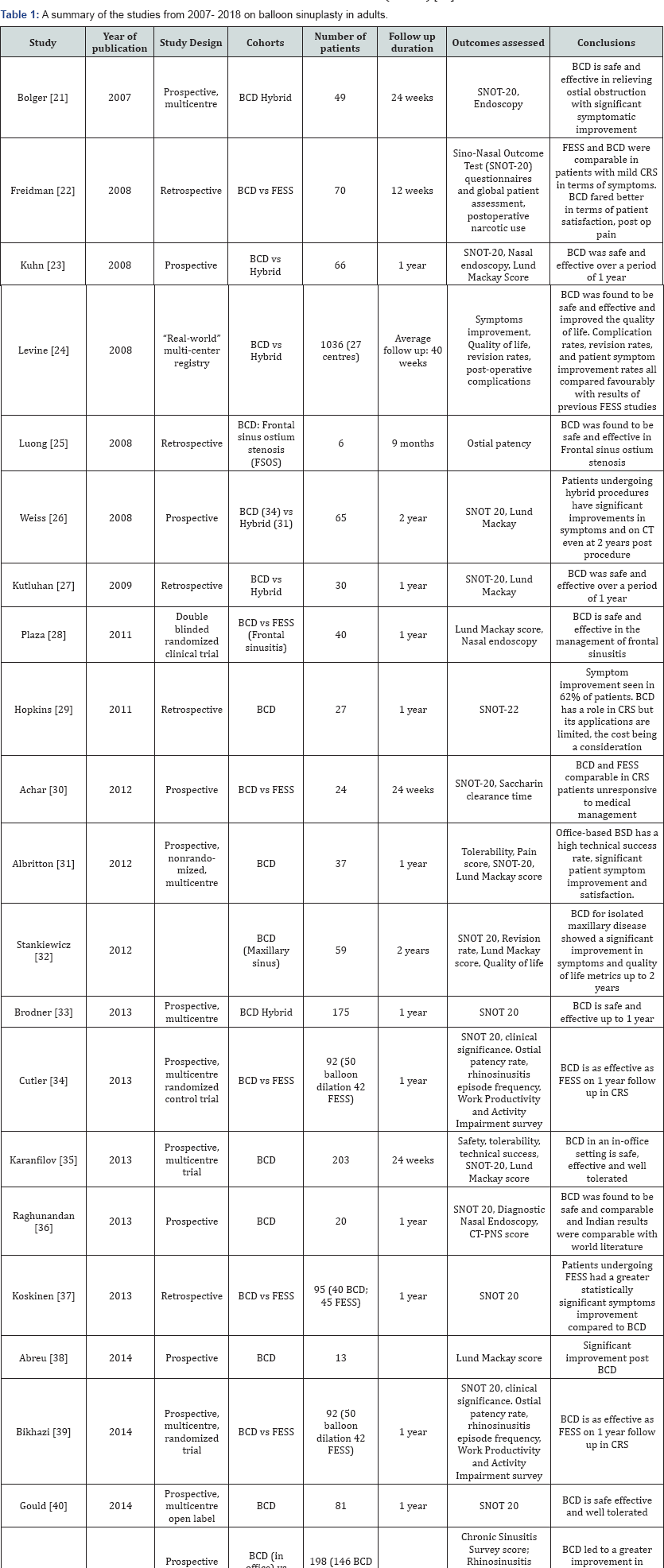
Google Scholar and Pub Med were used for the literature search from 2005 to 2018and all studies involving balloon dilation in adults with chronic rhinosinusitis were reviewed. The studies in the paediatric population were eliminated. 22 trials were included in this review along with 3 meta-analyses and 1 registry based real world evidence study. Most studies on Balloon Sinuplasty assessed outcomes such as symptom improvement (SNOT 20 or SNOT 22), nasal endoscopy score, Lund-Mackay score, safety, tolerability, revision rates, quality of life and duration of improvement post procedure. Studies from various countries, including India, were also included to look at the impact of the procedures in various patient populations.
Results & Discussion
The REMODEL (randomized evaluation of maxillary antrostossmy versus ostial dilation efficacy through longterm follow-up) was a multicentre randomized control trial examining the long term outcomes of standalone balloon sinus dilation versus FESS. In the large cohort of 135 patients treated with functional endoscopic sinus surgery (FESS) or in-office balloon dilation, 18 month data as well as 24 month follow data was studied. The investigators found that the outcomes of FESS and standalone balloon sinuplasty were found to be comparable at all time points from 6 months to 24 months. In addition they also noted that balloon dilation produced faster recovery, less postoperative pain, and fewer debridements than FESS. Koshinen et al. compared the 5 year efficacy and satisfaction in patients who underwent FESS or balloon sinuplasty for maxillary sinus diseases (Table 1) [21].
Altogether 45 patients were included in the FESS group and 40 patients in the balloon sinuplasty group. Of those followed up for an average of 6 years, both groups were satisfied with the procedure and experienced a significant improvement in symptoms. However the number of reported exacerbations was higher in the balloon sinuplasty group with 4 patients requiring revision procedures. In a prospective multicentre study by Karanfilov 203 patients with refractory chronic sinusitis underwent balloon sinuplasty treatment in an office setting under LA and were followed up at 2, 8 and 24 weeks post procedure [22]. Statistically significant clinical improvements were noted in SNOT-20 scores and LMK computed tomography (CT) scores. 82.3% of patients reported the procedure as tolerable or highly tolerable with statistically significant improvement in quality of life from baseline at various time points including 2 weeks, 8 weeks and 24 weeks (>0.8) [23].
Past published literature on efficacy was broadly limited to feasibility studies and safety profiling. One of the initial trials, The 'Clinical Evaluation to confirm safety and efficacy of sinuplasty in the paranasal sinuses' (CLEAR) study, was a multicentre trial of 115 patients demonstrated high success rate as well as both safety and efficacy of the procedure with 97% success rate. Another study by Kuhn et al. reported endoscopic patency of 85% at one year. Improvements in SNOT-20 scores were also reported in the latter. The REMODEL Meta-analysis included 358 patients, with follow up in 314 patients for at least 1 year and follow up in 74 patients for 2 years [24,25]. The SNOT-20 scores exhibited significant improvement from baseline at all time points. This meta-analysis found that the improvements in symptoms and quality of life in those who underwent standalone balloon dilation could be maintained for 2 years post dilation. The study also looked at other metrics such as long-term benefits with regard to days missed homebound days, physician/nurse visits, acute infections, and antibiotic use for acute exacerbations and concluded that balloon sinuplasty led to an improvement in all categories [21].
In a systematic review and meta-analysis by Levy et al. the investigators evaluated quality of life and sinus opacification in CRS patients who underwent balloon sinuplasty. 17 studies were evaluated. A significant improvement in self-reported quality of life was reported in five studies which also contained SNOT-20 scores up to 1 year post procedure. A significant improvement in paranasal sinus opacification was reported in 5 studies in two of the studies evaluated, in which there was a direct comparison drawn between FESS and Balloon dilation, the SNOT 20 outcomes were found to be comparable. In another meta-analysis in China by Xu et al., 7 of the prospective before-after self-controlled studies looked at improvements in SNOT-20 scores [26], Lund Mackay scores at 6 months and one year post balloon sinuplasty were statistically significant (P<0.05)and the authors concluded that the postoperative effect of balloon sinuplasty on chronic rhinosinusitis was evident [27].
A "real-world" multi-centre registry study by Levine et al. assessed the safety and effectiveness of balloon sinuplasty in of 1,036 patients in 27ENT practices. Data collected over 18 months demonstrated that balloon sinuplasty was used in 3,276 sinuses with an average follow-up up to 40 weeks. In 95.2% of subjects symptoms were found to have been improved with no major adverse events reported and a revision rate of 1.3% of the sinuses dilated. The authors concluded that balloon sinuplasty was both safe and effective with complication rates, revision rates, and symptom rates all comparing favourably with those reported in literature in traditional FESS. In India Raghunandan et al. conducted a single institute, prospective study to assess the outcomes of balloon sinuplasty [28]. A consecutive series of 20 patients with chronic rhinosinusitis underwent balloon sinuplasty and were followed up over a period of 1 year.
Dramatic relief from symptoms were found within the 1st postoperative week, demonstrated by a reduction in the SNOT 20 scores (68% to 16%) and all patients found to be symptom free during further follow up. Statistically significant improvement was also seen in the Lanza Kennedy nasal endoscopy score with a drop from an average preoperative score of 61.25% to 22.5%, 1 year post procedure. The Lund Mackay score also improved significantly from a score of 47.71% preoperatively to 16.25% one year post procedure. Antrostomies and Caldwell Luc procedures were, at a point in time, the preferred methods to treat chronic sinusitis [29]. The outlook changed tremendously when in the late 1970s, Messerligker principles on mucociliary clearance and detailing of intranasal pathologies including the osteomeatal concept led to the inculcation into functional sinus surgery by Kennedy in the 1980s. The goal of FESS is to establish normal drainage and ventilation of the paranasal sinuses by removal of diseased tissue [30].
Since FDA approval in 2005 there have been multiple studies including control trials and long term follow data with encouraging results however balloon sinuplasty has remained the topic of heated debates. The concept of opening the ostia by mucosal and bony compression, as compared to the removal of diseased mucus lining and bone has not been accepted by the Rhinologists especially since it was found that 53% of patients had underlying inflammation. The recurrence of inflammation remains a concern for most surgeons [31]. However as per literature FESS does not remove every piece of inflamed tissue either thus adding further fuel to the debate [18] Based on the aforementioned point of debate is the revision rate of the balloon sinuplasty vs. FESS is another highly contested topic [4]. A prospective national audit of sinus surgeries by The Royal College of Surgeons of England included 3128 patients who underwent FESS. In agreement with literature the rate of major complications was low and occurred in only 0.4%.
Minor complications occurred in 6.6%, such as excessive preoperative bleeding, postoperative infection, stenosis and adhesions. The revision rate of FESS in literature have found to range from 2% to 24% with revision procedures found to have a significantly higher rate of complications and failure rates [32]. One concern is that the rate of revision is Balloon dilation is considerably higher [33]. Although the revision rates have not been compared in large trials the REMODEL trial was one that compared revision rates, albeit with a small sample size, at 18 months and found that revision rate was 2.7% for balloon sinuplasty and 6.9% in FESS arms and but were not statistically significant [21]. In another trial of 65 by Weiss et. al. the revision balloon dilation were found to be necessary in 3.6% of the total number of sinuses dilated which comprised 9.2% of the total patient pool [34].
Another point of debate is the category of chronic rhinosinusitis patients in whom balloon sinuplasty is indicated. Balloon dilation cannot be used as standalone procedures in which disease clearance is of the essence, as in nasal polyposis, fungal sinusitis or neoplasm. In most studies, the inclusion criteria include patients with the presence of unilateral or bilateral maxillary, frontal or sphenoidal sinusitis unresponsive to medical management. The exclusion criteria, other than those mentioned above, included distorted osteomeatal anatomy, previous sinonasal surgery, isolated ethmoidal sinus or infundibular disease, nasal trauma, ciliary dysmotility syndrome and cystic fibrosis [35]. Although most view balloon sinuplasty as a standalone procedure to be used in lieu of FESS, multiple studies have used balloon dilation in a hybrid procedure with FESS being used along with balloon dilation. This is specifically useful for the frontal recess which is has a relatively high risk of stenosis [36].
Among the studies published on balloon dilation since its approval, they have all demonstrated statistically significant improvements in symptoms, quality of life, nasal endoscopy scores and CT-PNS scores when compared to medical management and comparable results when compared to FESS. It was also found to be both a safe and tolerable procedure. Balloon sinuplasty procedures per 10,000 beneficiaries in the US increased by 3.7% annually from 2000 to 2014 and the same metric increased from 2011 to 2014 by 59% annually [29,21]. The number of procedures in India too has risen since the technique was initiated in subcontinent in the 2000s. Despite a significant increase in the number of procedures being conducted in both India and the Western world one major obstacle in its acceptability was found to be its cost [29,36]. Bizaki et al. remarked that the high material cost of balloon sinuplasty in comparison to FESS led to lower uptake. The authors mentioned the need to bring about higher cost saving through in office procedures or the reduction of material costs to improve its acceptability among surgeons in their practice [37-51].
Conclusion
This review includes prospective and retrospective trials since 2008. Balloon sinuplasty has been used as standalone procedure as well as pitted against traditional FESS and medical management. It also includes multiple meta-analyses conducted as well as real world evidence registry based study. The results of these trials conclude that balloon sinuplasty is not only effective in patients with chronic rhinosinusitis but also safe and well tolerated. The stumbling block mentioned in multiple trials has been the high cost of the procedure. Evidence suggests that balloon sinuplasty, if made more affordable, is a valuable addition in the armamentarium of surgeons against chronic rhinosinusitis especially due to its low invasiveness, thus reserving the more invasive and radical options for severe and refractory cases.
Acknowledgement
The authors are grateful to Inn Accel Technology Pvt. Ltd for providing access to resources and infrastructure to carry out this research. We would like to thank Dr. Sunil Narayan Dutt, Director and Professor at the Department of ENT, Apollo Hospitals Bangalore for his guidance and support towards the understanding of balloon sinuplasty and its usage.
References
- Schappert SM (1992) National Ambulatory Medical Care Survey: 1991 Summary Hyattsville, Maryland: National Center for Health Statistics, USA.
- Gross CW, Schlosser RJ (2001) Prevalence and economic impact of rhinosinusitis. Current Opinion in Otolaryngology & Head and Neck Surgery 9(1): 8-10.
- Lal Devyani, Joseph M Scianna, James A Stankiewicz (2009) Efficacy of targeted medical therapy in chronic rhinosinusitis, and predictors of failure. American journal of rhinology & allergy 23(4): 396-400.
- Melroy CT (2008) The balloon dilating catheter as an instrument in sinus surgery. Otolaryngology - Head and Neck Surgery 139(Suppl 3): S23-26.
- Jagdish C, Sunil ND, Pooja K, Roma V (2016) Factors that Delay Definitive Management of Chronic Rhinosinusitis in India: A survey based study Glob J Otolaryngol 2(3).
- Melen I (1994) Chronic Sinusitis: Clinical and pathophysiological aspects. Acta Otolaryngolgica 515: 45-48.
- Adams PF, Hendershot GE, Marano MA (1996) Current estimates from the National Health Interview Survey. Vital and Health Statistics 200: 1-203.
- Blackwell DL, Collins JG, Coles R (1997) Summary health statistics for U.S. adults: National Health Interview Survey. Vital and Health Statistics 205: 1-109.
- Pleis JR, Lucas JW, Ward BW (2008) Summary health statistics for US adults: National Health Interview Survey Vital Health Stat 10(242): 1-157
- Ahmed, Jahangir (2011) Functional endoscopic balloon dilation of sinus ostia for chronic rhinosinusitis. The Cochrane Library.
- Sturgess JM, Chao J, Wong J, Aspin N, Turner JA (1979) Cilia with defective radial spokes: a cause of human respiratory disease. New England Journal of Medicine 300(2): 53-56.
- Zacharek MA, Krouse JH (2003) The role of allergy in chronic rhinosinusitis. Current Opinion in Otolaryngology & Head and Neck Surgery 11(3): 196-200.
- Timperley D, Schlosser RJ, Harvey RJ (2010) Chronic rhinosinusitis: an education and treatment model. Otolaryngology - Head and Neck Surgery 143 (5 Suppl 3): S3-8.
- Lal Devyani, Joseph M Scianna, James A Stankiewicz (2009) Efficacy of targeted medical therapy in chronic rhinosinusitis, and predictors of failure. American journal of rhinology & allergy 23(4): 396-400.
- Lanza DC (1993) Postoperative care and avoiding frontal recess stenosis. In: Abstracts of the International Advanced Sinus Symposium, Philadelphia, PA, USA.
- Bolger WE, Vaughan WC (2006) Catheter-based dilation of the sinus ostia: initial safety and feasibility analysis in a cadaver model. Am J Rhinol 20(3): 290-294.
- Brown CL, Bolger WE (2006) Safety and feasibility of balloon catheter dilation of paranasal sinus ostia: a preliminary investigation. Ann Otol Rhinol Laryngol 115(4): 293-299.
- Lanza DC, Kennedy DW (2006) Balloon sinuplasty: not ready for prime time. Annals of Otology, Rhinology and Laryngology 115(10): 789-790.
- Tomazic PV, Stammberger H, Braun H, Habermann W, Schmid C, et al. (2013) Feasibility of balloon sinuplasty in patients with chronic rhinosinusitis: the Graz experience. Rhinology 51(2): 120-127.
- Neto WC, Pinna FR, Voegels RL (2008) Balloon Sinuplasty: Literature Review. Int Arch Otorhinolaryngol 12(4): 559-564.
- Chandra RK, Kern RC, Cutler JL, Welch KC, Russell PT (2016) REMODEL larger cohort with long-term outcomes and meta-analysis of standalone balloon dilation studies. The Laryngoscope 126(1): 44-50.
- Anni Koskinen, Jyri Myller, Petri Mattila, Matti Penttila, Juha Silvola, e al. (2016) Long-term follow-up after ESS and balloon sinuplasty: Comparison of symptom reduction and patient satisfaction. Acta Oto- Laryngologica 136(5): 532-536.
- Karanfilov B, Silvers S, Pasha R, Sikand A, Shikani A, et al. (2013) Office- based balloon sinus dilation: a prospective, multicenter study of 203 patients. International forum of allergy & rhinology 3(5): 404-411.
- Bolger WE, Brown CL, Church CA, Goldberg AN, Karanfilov B, et al. (2007) Safety and outcomes of balloon catheter sinusotomy: a multicenter 24-week analysis in 115 patients. Otolaryngology-Head and Neck Surgery 137(1): 10-20.
- Kuhn FA, Church CA, Goldberg AN, Levine HL, Sillers MJ, et al. (2008) Balloon catheter sinusotomy: one-year follow-up-outcomes and role in functional endoscopic sinus surgery. Otolaryngology-Head and Neck Surgery 139(3_suppl_1): S27-S37.
- Levy Joshua M, Michael J Marino, Edward D McCoul (2016) Paranasal sinus balloon catheter dilation for treatment of chronic rhinosinusitis: a systematic review and meta-analysis. Otolaryngology-Head and Neck Surgery 154(1): 33-40.
- Xu CY, Zhu L, Zhang H, An FY, Bai MY (2017) Postoperative effects of balloon sinuplasty on chronic rhinosinusitis: a Meta-analysis. Chinese journal of otorhinolaryngology head and neck surgery 52(11): 835840.
- Levine HL, Sertich AP, Hoisington DR, Weiss RL, Pritikin J (2008) Patient Registry Study Group. Multicenter registry of balloon catheter sinusotomy outcomes for 1,036 patients. Annals of Otology, Rhinology & Laryngology 117(4): 263-270.
- Raghunandhan S, Bansal T, Natarajan K, Kameswaran M (2013) Efficacy & outcomes of balloon sinuplasty in chronic rhinosinusitis: a prospective study. Indian Journal of Otolaryngology and Head & Neck Surgery 65(2): 314-319.
- Lazar RH, Younis RT, Long TE (1993) Functional endonasal sinus surgery in adults and children. The Laryngoscope 103(1): 1-5.
- Lee JT, Kennedy DW, Palmer JN, Feldman M, Chiu AG (2006) The incidence of concurrent osteitis in patients with chronic rhinosinusitis: a clinicopathological study. American Journal of Rhinology 20(3): 278282.
- Hopkins C, Slack R, Lund V, Brown P, Copley L, et al. (2009) Long-term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusiti. The Laryngoscope 119(12): 2459-2465.
- Jiang RS, Hsu CY (2002) Revision functional endoscopic sinus surgery Annals of Otology, Rhinology & Laryngology 111(2): 155-159.
- Weiss RL, Church CA, Kuhn FA, Levine HL, Sillers MJ, et al. (2008) Long-term outcome analysis of balloon catheter sinusotomy: two-year follow-up. Otolaryngology Head and Neck Surgery 139(3 suppl1): S38- 46.
- Jones N (2006) Safety and feasibility of balloon-catheter dilation of paranasal sinus ostia: a preliminary investigation. Annals of Otology Rhinology and Laryngology 115: 300-301.
- Calixto NE, Gregg Jaymes T, Liang J, Jiang N (2017) Sinus procedures in the Medicare population from 2000 to 2014: a recent balloon sinuplasty explosion. The Laryngoscope 127(9): 1976-1982.
- Bizaki A, Taulu R, Numminen J, Rautiainen M (2014) Quality of life after endoscopic sinus surgery or balloon sinuplasty: a randomized clinical study. Rhinology 52(4): 300.
- Kutluhan A, Bozdemir K, £etin h, Yalfiner G, žalviz M, et al. (2009) Endoscopic balloon dilation sinuplasty including ethmoidal air cells in chronic rhinosinusitis. Annals of Otology, Rhinology & Laryngology 118(12): 881-886.
- Plaza G, Eisenberg G, Montojo J, Onrubia T, Urbasos M, et al. (2011) Balloon dilation of the frontal recess: a randomized clinical trial. Annals of Otology, Rhinology & Laryngology 120(8): 511-518.
- Hopkins C, Noon E, Bray D, Roberts D (2011) Balloon sinuplasty: our first year. The Journal of Laryngology & Otology 125(1): 43-52.
- Achar P, S Duvvi, BN Kumar (2012) Endoscopic dilatation sinus surgery (FEDS) versus functional endoscopic sinus surgery (FESS) for treatment of chronic rhinosinusitis: a pilot study. Acta Otorhinolaryngologica Italica 32(5): 314.
- Albritton IV Ford D, Roy R Casiano, Michael J Sillers (2012) Feasibility of in-office endoscopic sinus surgery with balloon sinus dilation. American journal of rhinology & allergy 26(3): 243-248.
- Stankiewicz J, Truitt T, Atkins J, Winegar B, Cink P, et al. (2012) Two- year results: transantral balloon dilation of the ethmoid infundibulum. International forum of allergy & rhinology 2(3): 199-206.
- Brodner D, Nachlas N, Mock P, Truitt T, Armstrong M, et al. (2013) Safety and outcomes following hybrid balloon and balloon-only procedures using a multifunction, multisinus balloon dilation tool. International forum of allergy & rhinology 3(8): 652-658.
- Cutler J, Bikhazi N, Light J, Truitt T, Schwartz M, et al. (2013) Standalone balloon dilation versus sinus surgery for chronic rhinosinusitis: a prospective, multicenter, randomized, controlled trial. American journal of rhinology & allergy 27(5): 416-422.
- Koskinen A, Penttila M, Myller J, Hammaren-Malmi S, Silvola J, et al. (2012) Endoscopic sinus surgery might reduce exacerbations and symptoms more than balloon sinuplasty. American journal of rhinology & allergy 26(6): e150.
- Abreu CB, Balsalobre L, Pascoto GR, Pozzobon M, Fuchs SC, et al. (2014) Effectiveness of balloon sinuplasty in patients with chronic rhinosinusitis without polyposis. Braz J Otorhinolaryngol 80(6): 470475.
- Bikhazi N, Light J, Truitt T, Schwartz M, Cutler J, et al. (2014) Standalone balloon dilation versus sinus surgery for chronic rhinosinusitis: a prospective, multicenter, randomized, controlled trial with 1-year followup. Am J Rhinol Allergy 28: 323-329.
- Gould J, Alexander I, Tomkin E, Brodner D (2014) In-office, multisinus balloon dilation: 1-Year outcomes from a prospective, multicenter, open label trial. American journal of rhinology & allergy 28(2): 156163.
- Payne SC, Stolovitzky P, Mehendale N, Matheny K, Brown W, et al. (2016) Medical therapy versus sinus surgery by using balloon sinus dilation technology: A prospective multicenter study. American journal of rhinology & allergy 30(4): 279-286.
- Minni A, Dragonetti A, Sciuto A, Cavaliere C, Rosati D, et al. (2018) Use of balloon catheter dilation vs. traditional endoscopic sinus surgery in management of light and severe chronic rhinosinusitis of the frontal sinus: a multicenter prospective randomized study. European review for medical and pharmacological sciences 22(2): 285-293.





























