Identification of Unmet Clinical Needs in the Field of Otorhinolaryngology in India - A Modified Biodesign Approach
Parul Chachra1, Jagdish Chaturvedi2*, Darien Rodrigues1, Ravi Jangir1, Rishabh Sirdesai1, Abu Saquib Tauheed1, Rohan DSouza1 and Ramakrishna Pappu3
1Affordable Invention in MedTech Fellow, InnAccel Technologies, India
2ENTConsultant, Fortis Hospital, India
3Business Associate, InnAccel Technologies, India
Submission: March 21, 2018; Published: April 26, 2018
*Corresponding author: Jagdish Chaturvedi, ENT Consultant, Fortis Hospital, India, Tel: 9650928582;Email: dr.jagdishc@ymail.com
How to cite this article: Parul C, Jagdish C, Darien R, Ravi J, Rishabh S, et al. A Real-Time Sequential Phase-Shift Approach to Tinnitus Cancellation-A Pilot Study in Southern India. Glob J Otolaryngol 2018; 15(1): 555904. DOI: 10.19080/GJO.2018.15.555904
Abstract
Background: Otorhinolaryngology;Ear, Nose and Throat (ENT) related diseases are exceedingly common in India. A huge number of conditions are managed ineffectively due to various reasons. Trained personnel are not accessible uniformly in all geographies, and affordable solutions catering to Indian healthcare system are scarce. Inefficient problem identification contributes to the current poor state of treatment in healthcare ecosystem. There is a clear need for strategic problem identification in the field of Otorhinolaryngology.
Methods: A multidisciplinary team of an engineer, a product designer, a doctor and a business graduate was constructed. Following the Biodesign process, the team was immersed in the ENT department of a tertiary care hospital for 8 weeks, wherein it followed clinicians in their day-to-day activities such as out-patient clinics, surgeries and wards rounds and made detailed observations. Various pain points were identified where suboptimal treatment was delivered to the patient. Detailed observations were recorded, which were used to arrive at corresponding need statements. The needs were prioritized based on a custom made ranking scale.
Results: Through 2-month clinical immersion, 198 needs were identified in the ENT space. After applying a systematic and scientific filtering method, inspired by Biodesign process, top ten needs were identified, which were successfully cross-validated with several ENT specialists across the country.
Conclusion: A strategic method to identify problems and pain points in the ENT space led to the identification of several validated unmet clinical needs. Total of 198 needs were ranked based on criticality, prevalence and incidence, technical complexity and potential market opportunities.
Keywords: Clinical unmet needs; Otorhinolaryngology; ENT; Ear Nose Throat; Biodesign; Medtech; Innovation; Inventing medical devices
Abbreviations: ENT: Ear Nose Throat; NA: Not applicable
Introduction
In developing countries, the most common problems that warrant a visit to a doctor are related to ear nose and throat (ENT) [1,2]. ENT diseases often cause significant morbidity and lead to functional impairment of adults as well as children [3-6]. Due to paucity of corresponding numbers of ENT specialists for more than 1.2 billion population of India, patients present themselves to a general physician, get treated through community practices or self medicate [7]. ENT problems are also hugely managed in the community with home remedies. This problem gets complex since there is no training for public health Otorhinolaryngology personnel in developing countries [8,9]. This leads to mismanagement of a large number of cases thereby leading to severity of conditions, delayed treatment, and often long term negative implications on the patient's health. Most specialists are available in major urban areas of India, which leaves patients from rural areas with not enough support system in the vicinity and added costs [10,11]. Over of the medical devices used in India are imported and are therefore expensive for the doctors and hospitals, ensuing enhanced financial burden on patients. In developing countries, there is a requirement of devices that are designed to cater to their patient population, keeping affordability and accessibility in mind [12,13].
As less than of the Indian population is covered under any kind of insurance, it brings a huge burden on individual patients and families [14]. As ENT diseases lead to severe morbidity, this furthers the direct and indirect costs incurred by patients [1,3]. There is a lack of affordable and accessible solutions, providing effective management of the situation in the ENT space. This provides thrust for the innovative, frugal technology designed for Indian healthcare system in the ENT field and it is necessary to find the right needs before utilizing technology in order to make the status quo better in the ENT space. In this study, we followed a modified bio design process, originally developed by Stanford University, to identify unmet clinical needs in the field of ENT diseases. The modified bio design process is structured and thorough in its approach and provides with a priority list of unmet clinical needs.
Materials and Methods
Team and process
The process employed is a modified form of the Stanford bio-design process [15-17]. A multi-disciplinary team, including an engineer, a designer, and a Stanford Biodesign trained ENT clinician, performed clinical observations at a hospital in the ENT Department for a period of 8 weeks.
Observations to Need Statements
The observers recorded negative or undesirable outcomes in the care process of Otorhinolaryngology (ENT). These observations were made by shadowing clinicians and patients on a daily basis, observing procedures, finding out the patient history, and following up with patients as their treatment progressed. The observations were recorded in the form of dockets, each of which carried patient details, such as age, gender, patient history, observation, patient pathway, patient follow-up, and the time, date and place where the observation was made. From each observation, the negative outcome and problem was highlighted and a clinical need statement was defined.
Need Filtration Process
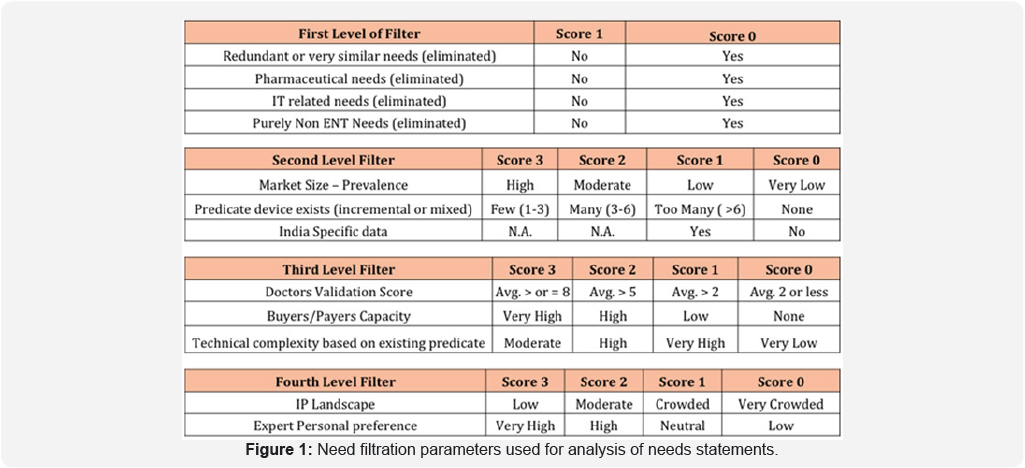
The needs were filtered through a structured process. They were prioritized using certain quantifiable metrics to obtain a robust collection of high impact and context specific needs. The filtration process was conducted in four levels (Figure 1). The first level of filtration consisted of eliminating redundant needs, and needs related to pharmaceutical, IT (Information Technology) or non-ENT spaces. This was done to exclude needs that were irrelevant or that would have no product- based solutions. The second level of filtration was based on identifying predicate devices or existing devices addressing similar problems for each need, literature review and frequency of occurrence of each need based on two factors- the clinician's multiple years of experience in the field and the observers' experience during the immersion period. Market size prevalence was scored very low (<2; of the population or if no standard reference available), low (2-5; of the population or if clinicians felt the prevalence was significant but no data was available to support), moderate (5-10; of the population) or high (10; of the population). Each need was scored and filtered based on an unbiased numerical scoring system. The third level of filtering was based upon the criticality of the need and understanding the technological feasibility of innovation for a particular need. The fourth and final level of filtering was performed by scoring every need in terms of intellectual property (IP) landscape, and through clinical feedback from multiple clinicians from various hospitals.
Results
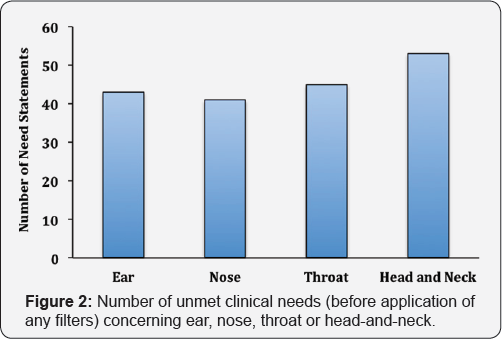
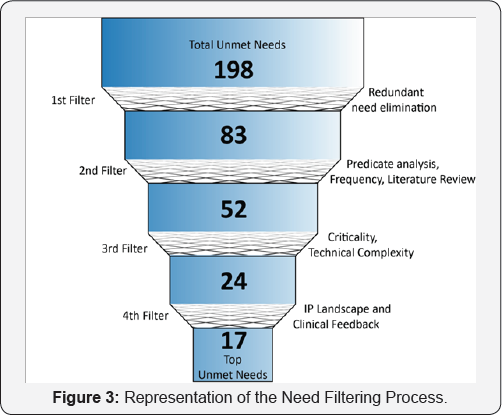
Based on detailed observations made during the clinical immersion, total of 198 need statements, spanning across different areas in ENT space, were defined. The identified needs concerned with different regions -ear, nose, throat, head-and-neck and the distribution is shown in Figure 2. Certain needs concerned more than one region. Following the first filter, in which all the redundant, pharmaceutical, IT and non-ENT needs were eliminated, 83 needs remained (Figure 3). After the second filter (frequency and predicate analysis) application, 52 needs remained and rest was eliminated. Third filter (criticality and technical complexity) further reduced the needs to 17 in number. Fourth filter included IP landscape and Clinical feedback for scoring the needs and there were 17 needs left in the docket after that (Figure 3). Top ten need statements found after the application of all four filters are listed in Figure 4.
Discussion
Our findings provide the top ten needs in the field of Otorhinolaryngology in Indian setting that could be the utilized by healthcare start-ups, giant medtech companies, funding agencies, policy makers, government agencies as well as insurance companies for their purposes. We used an improvised bio-design process that could be used in other fields of medicine to identify unmet clinical needs, as has been done before in the field of emergency medicine by a multidisciplinary group under the guidance of a clinical expert in the bio-design process [15]. This process can support the development of indigenous products, designed to cater patients and clinicians in India. Following are the advantages of using this process to identify unmet clinical needs.
Advantages of Having A Multidisciplinary Team
Identifying unmet needs in a highly specialized space such as ENT requires an extensive understanding of the epidemiology of various disease states and the various methods in existence for diagnosis and treatment. Thus, in this process a clinician's involvement ensures that the team's time is utilized efficiently and critical needs are identified. The constant involvement of the ENT specialist greatly influenced the team in finding valuable and extensive information to identify and validate clinical needs.

The designer and the engineer brought a fresh perspective to the immersion. Observations and negative outcomes that might have been overlooked by the clinician in the team due to continuous previous exposure to the setting were picked up by the non-clinical members of the team in a novel environment to them. The two-month rigorous and intensive process of spending hours in the hospital, interacting with patients, nurses and doctors, and understanding the methods of diagnosis and treatment, helped the non-clinicians significantly enhance their understanding of ENT space, thus helping them extract meaningful information from the immersion to identify unmet needs. Multi-disciplinary teams bring together multiple points of view, and aid in discussing the observations extensively before making a judgment on the criticality. Teams devoid of clinicians or non-clinicians can lead to narrowed viewpoint towards certain subjects or biased decisions thereby leading to a compromise on the importance given to the identified needs.
The Need For Clinical Validation from Other Healthcare Centers
The identification of needs over a period of two months at a super-specialty hospital was very effective and produced some pressing needs for the development of innovative solutions. However, in order to study if the process followed indeed helped identify needs that the clinical experts in the field would agree with, it was important to validate the same at other hospitals. The clinical validation session conducted in Bangalore and Delhi reinforced the needs identified earlier, and provided wider points of view of these needs and potential ways of tackling the issues. It was also important to understand treatment in other hospitals as the facilities vary from hospital to hospital, depending upon the type of funding provided, the local patient intake, and other critical factors. The above two examples have been used to exemplify the need for an extended study of ENT from other doctors and hospitals to get a wholesome, unbiased outcome in terms of needs identification and validation.
Interacting with Patients and Clinicians
For an innovative process to become successful, it is important to empathize with the stakeholders involved [1619]. Through our clinical immersion, patients' and doctors; pain points, time, privacy were given the highest regard. In order to avoid distrust between the team members and doctors/patients, stemming from the team members' non-clinical background, appropriate training in communication and interpersonal skills was given to the team. In Indian healthcare system, clinicians are often overworked due to highly disproportionate ratio of clinicians to patients [20,21]. Our team members put in the efforts to not disturb their practice at any point of time or add to their burden.
The Importance of a Systematic and Scientific Filtering Process
The 2-month long clinical immersion and the multiple rounds of rigorous filtering ensured that the most pressing matters came on top with enough information and validation to support development of innovative products. Since designing solutions for clinical needs has the power to affect biological, social and/occupational conditions of a large number of people, it is important that the most pressing needs in the system are given priority to be solved. The modified Stanford Biodesign Process provided us with the top needs in the field of Otorhinolaryngology (ENT).
Conclusion
The modified Stanford Biodesign process is a structured way to identify unmet clinical needs. It incorporates Indian healthcare context and helps create a validated database of clinical needs for future innovation and invention of medical devices and diagnostics for the Indian Market. The Stanford Biodesign process had to be altered significantly to obtain an output of ten compelling clinical needs in the field of Otorhinolaryngology (ENT). The negative outcomes were well understood through four rounds of rigorous filtering that successively eliminated redundant and low-impact needs. The filtering parameters also ensured better insights into the disease space through predicate device analysis using a technical feasibility and buyer capacity study, and literature data on incidence and prevalence of the negative outcomes. Modified Biodesign process is a scientific and data driven approach that allowed objective evaluation, leading to the ten most compelling needs in the ENT space. The team is currently continuing its work towards creating affordable and innovative tools to make healthcare more accessible and suited for the Indian market in the ENT space. This methodology can be used effectively across various healthcare specialties, settings and geographies to identify critical problems that need innovative solutions in the developing countries.
Acknowledgements
The authors are grateful to All India Institute of Medical Sciences (AIIMS) India, Apollo Hospital (Bannerghatta Road, Bangalore) and Fortis Hospital (Vasant Kunj, Delhi) for providing access for clinical observer ship. The authors acknowledge Stanford Biodesign for providing the process on unmet need analysis. The authors also acknowledge InnAccel Technologies for providing the observers with the opportunity to conduct the clinical immersion guide the observers through the process and equip them to contribute to the MedTech Innovation space in India.
References
- ISD Scotland (1998) Scottish Health Statistics. Edinburgh: Information and Statistics Division. National Health Service in Scotland.
- McCormick A (1995) Morbidity statistics from general practice. Fourth national study 1991-1992. Office of population censuses and surveys.
- Kishve SP, Kumar N, Kishve PS, Aarif SM, Kalakoti P (2010) Ear, Nose and Throat disorders in paediatric patients at a rural hospital in India. Australasian Medical Journal 3(12): 786-790.?
- Witsell DL, Dolor RJ, Bolte JM, Stinnett SS (2001) Exploring health- related quality of life in patients with diseases of the ear, nose and throat: a multicenter observational study. Otolaryngology Head and Neck Surgery 125(4): 288-298.
- Njoroge GN, Bussmann RW (2006) Traditional management of ear, nose and throat (ENT) diseases in Central Kenya. Journal of Ethnobiology and Ethnomedicine 2(1): 54.
- Surapaneni H, Sisodia SS (2016) Incidence of ear, nose and throat disorders in children: a study in a teaching hospital in Telangana. International Journal of Otorhinolaryngology and Head and Neck Surgery 2(1): 26-29.
- Jha A, Unnikrishnan MK, Shanbhag R (2017) A Survey in Indian Population on Attitude to Self-Medication. Advanced Science Letters 23(3): 1983-1986.
- Alberti PW (1999) Pediatric ear, nose and throat services demands and resources: a global perspective. International journal of pediatric Otorhinolaryngology 49: S1-9.
- Newton VE, Macharia I, Mugwe P, Ototo B, Kan SW (2001) Evaluation of the use of a questionnaire to detect hearing loss in Kenyan pre-school children. International journal of pediatric Otorhinolaryngology 57(3): 229-234.
- Joshi P, Dutta S, Chaturvedi P, Nair S (2014) Head and neck cancers in developing countries. Rambam Maimonides medical journal 5(2): e0009.
- Agarwal AK, Sethi A, Sareen D, Dhingra S (2011) Treatment delay in oral and oropharyngeal cancer in our population: the role of socioeconomic factors and health-seeking behaviour. Indian Journal of Otolaryngology and Head & Neck Surgery 63(2): 145-150.
- Mahal A, Karan AK (2009) Diffusion of medical technology: medical devices in India. Expert review of medical devices 6(2): 197-205.
- Jarosiawski S, Saberwal G (2013) Case studies of innovative medical device companies from India: barriers and enablers to development. BMC health services research 13(1): 199.
- Kumar A, Jain N, Nandraj S, Furtado K (2015) NSSO 71st round: same data, multiple interpretations. Economic & Political Weekly 50(46-47): 84-87.
- Chaturvedi J, Logan A, Narayan G, Kuttappa S (2015) A structured process for unmet clinical need analysis for medical device innovation in India: early experiences. BMJ Innovations 1(3).
- Yock PG, Brinton TJ, Kumar UN, Watkins FJ, Denend L, et al. (2015) Biodesign. Cambridge University Press.
- Arun Kumar P, Sridhar S, Chaturvedi J, Deshpande RP Identification of unmet clinical needs in the field of nephrology-A modified bio-design approach.
- Backhouse A, Richards DA, McCabe R, Watkins R, Dickens C (2017) Stakeholders perspectives on the key components of community- based interventions coordinating care in dementia: a qualitative systematic review. BMC health services research 17(1): 767.
- McDermott K, Kurucz EC, Colbert BA (2018) Social entrepreneurial opportunity and active stakeholder participation: Resource mobilization in enterprising conveners of cross-sector social partnerships. Journal of Cleaner Production 183(10): 121-31.
- Deo MG (2013) Doctor population ratio for India-The reality. The Indian journal of medical research 137(4): 632-635.
- Deshpande JD, Phalke DB, Kalakoti P, Qutub D, Agrawal V (2013) Stress levels and depression amongst interns and resident doctors working in a tertiary care teaching hospital in rural area. International Journal of Health and Rehabilitation Sciences 2(1): 44-49.





























