Incidence of Nasal Foreign Body Impaction in India: Determined Using Literature Search, Interviews and Surveys
RishabhSirdesai1, Jagdish Chaturvedi2*, Ramakrishna Pappu3, Pooja Kadambi4, Vishal Prasad5, Ravi Jangir1, Darien Rodrigues1, Rohan D'Souza1, Abu Saquib Tauheed1 and Parul Chachra1
1Affordable Invention in Med Tech (AIM) Fellow, InnAccel Technologies Pvt. Ltd, India
2ENTConsultant, Fortis Hospital, India
3Business Associate, InnAccel Technologies Pvt Ltd, India
4Lead System Designer, InnAccel Technologies Pvt Ltd, India
5Design and Validation Engineer, InnAccel Technologies Pvt Ltd, India
Submission: March 21, 2018; Published: April 25, 2018
*Corresponding author: Jagdish Chaturvedi, Department of Otorhinolaryngology, Fortis Hospital, Bannerghatta road, Bangalore- 560 076,Tel: +91-9650928582, Email: dr.jagdishc@jrmail.com
How to cite this article: RishabhSirdesai, Jagdish C, Ramakrishna P, Pooja K, Vishal P, et al. Incidence of Nasal Foreign Body Impaction in India: Determined Using Literature Search, Interviews and Surveys. Glob J Otolaryngol 2018; 15(1): 555903. DOI: 10.19080/GJO.2018.15.555903
Abstract
Background: A Nasal Foreign Body (NFB) is an external object which gets lodged in the nasal cavity and may have certain risks such nasal infections, aspiration, edema etc. There exists limited literature with respect to the number of annual cases of nasal foreign body impaction in India. A survey and study was carried out to determine the incidence of nasal foreign body impaction cases in India.
Objectives: To determine the incidence of nasal foreign body impaction cases in India.
Methods: Determination of the total number of all units and sub-units in the healthcare system was carried out including community health centers and private clinics followed by calculation of the number of cases of foreign bodies seen annually in each of the units by interviews and surveys. Data was extrapolated via assumptions made by industry experts and clinicians through multiplying the cases per center with the number of centers to obtain total number of cases of impacted nasal foreign bodies.
Results: The approximate incidence of nasal foreign body impaction cases in India is 34.4 Million.
Conclusion: Despite the drawbacks of the various assumptions, the results obtained in this study through this methodology are a reasonable approximation of the total number of cases of nasal foreign body impaction occurring in India annually. This methodology can be utilised to determine incidence of similar cases in other domains. Better healthcare data infrastructure in India can reduce the need for such assumptions and result in the generation of more accurate data.
Keywords: Nasal Foreign Body; Incidence; ENT; Nose; India; children; NFB
Abbreviations: ENT: Ear, Nose & Throat (Otolaryngologist); CHC: Community Health Center; DH: District Hospital; EHR: Electronic Health Records; NFB: Nasal Foreign Body; CAGR: Compounded Annual Growth Rate
Introduction
India has a dire requirement for indigenous clinical research and it also has keen aspirants ready to pursue said research [1]. However, in India, due to the relatively nascent nature of clinical research and due to the lack of electronic health recording systems, clinical data is not readily available to pursue clinical research indigenously [1]. Despite of encouraging factors such as English-speaking health care professionals; expert western-trained clinicians growing economy; access to world- class technologies; ethnically diverse patient populations with diseases of public health relevance etc. there has not been an expected growth of clinical research in India, this is largely attributed to the lack of clinical data [1]. This paper focuses on the determination of the annual prevalence of nasal foreign bodies in India.
"In medical terms, a foreign object is something that is in the body but doesn't belong there." [2] A foreign body might get lodged in various locations. Out of the various body cavities, the Gastrointestinal (GI) tract is one of the most common locations for a foreign body. The concerned body can enter the GI tract through the mouth [3] or through the rectum [4]. Another possible location of foreign bodies is airways. Foreign bodies may enter airways and cause choking [5]. Other possible locations of foreign bodies may include eyes, skin, anus or rectum, blood vessels, ears, urethra, vagina and nose [6-13]. In younger children, the natural curiosity causes them to intentionally or unintentionally insert foreign bodies into their nose, ears and mouth [14]. Within the nose, the most common location of a foreign body is just anterior to the middle turbinate or below the inferior turbinate. Foreign bodies are found more commonly in the right side of the nasal cavity. This may be due to the higher prevalence of right-handed individuals who insert foreign bodies into their right naris [15]. Common foreign bodies found in the nasal cavity include small toys, erasers pieces, food, tissue, clay, pebbles, dirt, paired disc magnets and button batteries [16]. Due to the lack of accurate clinical data, the authors have included certain assumptions and extrapolation techniques in consultation with clinicians and industry experts to arrive at the annual number cases of nasal foreign bodies in India.
Methods
In order to determine the annual incidence of nasal foreign body cases in India, the first step was to determine the total number of hospitals in India. This includes hospitals in the public as well as the private domain. Hospitals in the public domain include Community Health Centers (CHCs), Subdivision Hospitals, District Hospitals, State Government Hospitals, Other State government or Central government Hospitals and Medical Colleges with Teaching Hospitals. Hospitals in the private domain include Hospitals, Home Clinics Practices (Otolaryngologist), Private Clinics (Paediatricians) and General Physician clinics.
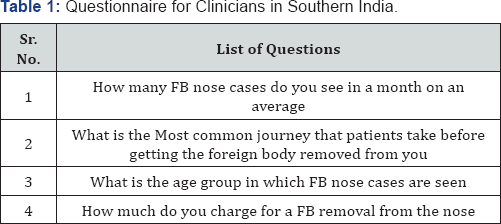
The total number of hospitals in India was obtained through a study in 2013 by a reputed health market research organisation [17]. The number of units of the various levels of healthcare in a government setup was obtained through a report published by Ministry of Health and Family Welfare, Government of India. Results obtained in 2013 were compounded using the given Compounded Annual Growth Rate (CAGR) to extrapolate for further years. Similar CAGR was assumed for Sub-divisional hospitals, other state or central government hospitals and state government hospitals. A uniform adherence to the CAGR was assumed. The number of private hospitals was obtained through a study conducted by a reputed market research firm [17]. The Number of Private Otolaryngologist clinics in the private domain were obtained through the Association of Otolaryngologists in India (AOI) [18]. The assumption made at this step was that 60% of all Otolaryngologists are registered with the AOI and that 50% of all Otolaryngologists have private practices. The Total number of general physicians in India was obtained through a study published by a reputed market research firm [19]. Assumed that 50% of all general physicians have private practices. Number of Paediatricians was obtained by assuming that number of paediatricians is twice the number of Otolaryngologists, CAGR assumed same as for general Physicians.
V(t0) = Start value
V(tt) = Finish Value
tn —t0 = Number of years
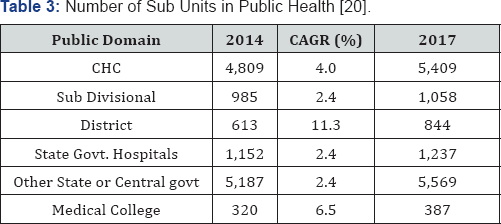
The next step was to determine the number of cases of nasal foreign bodies occurring annually at each level of healthcare both in the public and private domains. Due to the lack of clinical data on the internet, this step involved an intensive interviewing exercise conducted by the authors in Southern India. A detailed questionnaire was prepared. (Table 1) depicts the questions that were asked to doctors at various levels of healthcare in Southern India.
Assumptions made for the public domain at this stage are as follows:
a) All Medical colleges behave similarly, i.e. all medical colleges and teaching hospitals see a similar number of annual cases of nasal foreign bodies.
b) All District Hospitals behave similarly.
c) All CHCs behave similarly.
d) All State government hospitals behave similarly.
e) State government hospitals approximately see an average number of cases between CHCs and District Hospitals.
f) Assumptions made for the Private domain at this stage are as follows:
g) All Otolaryngologist clinics behave similarly.
h) All private hospitals behave similarly.
i) All General Physicians behave similarly
j) All Paediatricians behave similarly.
k) Number of cases seen by general physician and paediatricians is twice the number of cases seen by Otolaryngologists.
l) Private hospitals observed 20% of the total number of cases of public hospitals.
The average number of cases per year at each level of the healthcare system was obtained by multiplying approximate cases seen by an individual unit at each level by the number of units at that particular level of healthcare.
Total Case sCHC = Number of Cases at each CHCx Number ofCHCs
Similarly, a total number of cases were obtained for each level of healthcare both in the government and private domains and summed up to obtain the total number of nasal foreign body cases in India.
Results
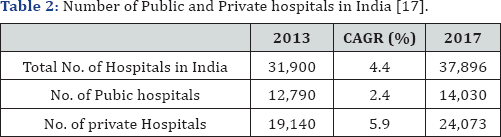
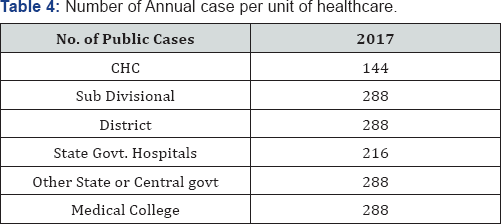
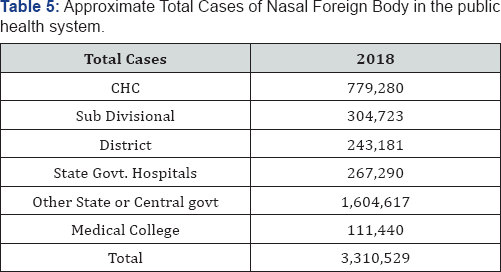
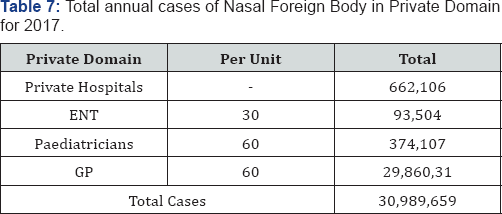
The approximate number of Public and Private Hospitals and health centers is depicted in (Table 2). Data was obtained in 2013 and has been extrapolated to 2017 using the CAGR of 4.4% for total hospitals, 2.4% for public hospitals and 5.9% for private hospitals [17]. Table 3 depicts the approximate number of sub units in public healthcare which was determined by extrapolating data published by a reputed consulting firm [20]. Table 4 represents the approximate total annual cases seen per unit of healthcare which was obtained through and intensive interviewing exercise. Table 5 represents the approximate total cases seen in all units of healthcare annually. Table 6 depicts the approximate number of sub units in public healthcare which was determined by extrapolating data published by a reputed market research firm as well as referring to the Association of otolaryngologists of India. CAGR determined through expert consultation [17-19]. (Table 7) represents the approximate total annual cases seen per unit of healthcare and total cases seen in 2017 which was obtained through and intensive interviewing exercise. Hence total annual Cases of nasal foreign bodies in 2017 is the sum of the total obtain from (Tables 5 & 7). Annual Incidence of nasal foreign bodies in India in 34.4 Million.

Discussion
Unlike the west, Clinical data in India is very rarely logged in the form of Electronic Health Records [21]. Due to this, it is very difficult to maintain clinical data on a public platform. Due to the lack of clinical data in India, countrywide incidence and prevalence is usually obtained through fieldwork, interviewing exercises, and extrapolation and expert assumptions. In this study, the number of cases of nasal foreign bodies was obtained through an extensive interviewing exercise in southern India. The authors prepared a questionnaire of four quantitative questions which was then taken in person to several hospitals, clinics, and health centers in India both in the public and private domain. Although this study gives us the fairly accurate number of nasal foreign bodies, it also has certain limitations. The assumption that all tertiary care centers and medical colleges behave the same can be challenged by the fact that population density varies throughout India and clinician density is higher in urban regions as compared to rural regions [22]. The assumption that all community health centers (CHCs) behave similarly also can be challenged on the same basis. Another factor that can challenge this assumption is the disparity in CHC infrastructure in urban and rural regions as well as the disparity between rural CHCs of various states with states like Kerala and Tamil Nadu having better healthcare infrastructure as compared to states like Uttar Pradesh (UP) and Bihar having poor healthcare facilities [23]. The assumption that all general physicians behave similarly can be challenged by the fact that some GPs prefer to refer out cases of nasal foreign bodies to Otolaryngologists rather than managing themselves. This study does not take into account the several that occur in the home environment and which are managed at home by the family member and the attending. Despite all of the challenging factors mentioned, the number 34.4 Million is one of the most accurate representations of the incidence of nasal foreign bodies in India. This study comprehensively takes into account the each and every unit in the public health system. It also takes into account the various stakeholders in the private system which includes Otolaryngologists, Paediatricians, and General Physicians. It includes calculated assumptions made by industry experts as well as experienced clinicians. In India, if there is to be a publically available database for clinical data to aid clinical research, there has to be a comprehensive change in the way the data is recorded, stored, transmitted and published. Electronic Health Records (EHR) has tremendous potential in the India market due to the sheer volumes of patients and the lack of accurate data [21]. In order to implement HER and ensure the validity of clinical data, there has to be a change at the grassroots level where the data is recorded. The adoption of EHR will provide clinical researchers with accurate incidence and prevalence data and reduce the assumptions made in various surveys and calculations.
Conclusion
Despite the lack of clinical data on the subject, the authors in consultation with industry experts and clinicians arrived at a fairly accurate approximation of the total annual cases of nasal foreign bodies in India. All assumptions were made in consultation with said experts and clinicians. And all values were calculated using the lower limits of the ranges provided. The total annual cases of foreign bodies in India in the year 2017 are approximately equal to 34.4 Million. The adoption of electronic health records and other database systems will mostly eradicate the use of assumptions and approximations and make accurate clinical data available for ingenious clinical research.
Acknowledgements
The authors would like to thank InnAccel Private Limited for supporting the AIM fellows in writing this article. Special thanks to Kolkata Medical College, Kolkata Hospital, and Rajendra Medical College for their support during this study.
References
- ISD Scotland (1998) Scottish Health Statistics. Edinburgh: Information and Statistics Division. National Health Service in Scotland.
- McCormick A (1995) Morbidity statistics from general practice. Fourth national study 1991-1992. Office of population censuses and surveys.
- Kishve SP, Kumar N, Kishve PS, Aarif SM, Kalakoti P (2010) Ear, Nose and Throat disorders in paediatric patients at a rural hospital in India. Australasian Medical Journal 3(12): 786-790.
- Witsell DL, Dolor RJ, Bolte JM, Stinnett SS (2001) Exploring health- related quality of life in patients with diseases of the ear, nose and throat: a multicenter observational study. Otolaryngology Head and Neck Surgery 125(4): 288-298.
- Njoroge GN, Bussmann RW (2006) Traditional management of ear, nose and throat (ENT) diseases in Central Kenya. Journal of Ethnobiology and Ethnomedicine 2(1): 54.
- Surapaneni H, Sisodia SS (2016) Incidence of ear, nose and throat disorders in children: a study in a teaching hospital in Telangana. International Journal of Otorhinolaryngology and Head and Neck Surgery 2(1): 26-29.
- Jha A, Unnikrishnan MK, Shanbhag R (2017) A Survey in Indian Population on Attitude to Self-Medication. Advanced Science Letters 23(3): 1983-1986.
- Alberti PW (1999) Pediatric ear, nose and throat services demands and resources: a global perspective. International journal of pediatric Otorhinolaryngology 49: S1-9.
- Newton VE, Macharia I, Mugwe P, Ototo B, Kan SW (2001) Evaluation of the use of a questionnaire to detect hearing loss in Kenyan pre-school children. International journal of pediatric Otorhinolaryngology 57(3): 229-234.
- Joshi P, Dutta S, Chaturvedi P, Nair S (2014) Head and neck cancers in developing countries. Rambam Maimonides medical journal 5(2): e0009.
- Agarwal AK, Sethi A, Sareen D, Dhingra S (2011) Treatment delay in oral and oropharyngeal cancer in our population: the role of socioeconomic factors and health-seeking behaviour. Indian Journal of Otolaryngology and Head & Neck Surgery 63(2): 145-150.
- Mahal A, Karan AK (2009) Diffusion of medical technology: medical devices in India. Expert review of medical devices 6(2): 197-205.
- Jarosiawski S, Saberwal G (2013) Case studies of innovative medical device companies from India: barriers and enablers to development. BMC health services research 13(1): 199.
- Kumar A, Jain N, Nandraj S, Furtado K (2015) NSSO 71st round: same data, multiple interpretations. Economic & Political Weekly 50(46-47): 84-87.
- Chaturvedi J, Logan A, Narayan G, Kuttappa S (2015) A structured process for unmet clinical need analysis for medical device innovation in India: early experiences. BMJ Innovations 1(3).
- Yock PG, Brinton TJ, Kumar UN, Watkins FJ, Denend L, et al. (2015) Biodesign. Cambridge University Press.
- Arun Kumar P, Sridhar S, Chaturvedi J, Deshpande RP Identification of unmet clinical needs in the field of nephrology-A modified bio-design approach.
- Backhouse A, Richards DA, McCabe R, Watkins R, Dickens C (2017) Stakeholders perspectives on the key components of community- based interventions coordinating care in dementia: a qualitative systematic review. BMC health services research 17(1): 767.
- McDermott K, Kurucz EC, Colbert BA (2018) Social entrepreneurial opportunity and active stakeholder participation: Resource mobilization in enterprising conveners of cross-sector social partnerships. Journal of Cleaner Production 183(10): 121-31.
- Deo MG (2013) Doctor population ratio for India-The reality. The Indian journal of medical research 137(4): 632-635.
- Deshpande JD, Phalke DB, Kalakoti P, Qutub D, Agrawal V (2013) Stress levels and depression amongst interns and resident doctors working in a tertiary care teaching hospital in rural area. International Journal of Health and Rehabilitation Sciences 2(1): 44-49.





























