Transoral Laser Microsurgery for Isolated Uvula & Soft Palate Malignancy-A Single Centre Experience
Deepak Verma*, Naveen Sharma and Uma Garg
Department of Otorhinolaryngology, BPS Government Medical College for Women, India
Submission: March 27, 2018; Published: April 06, 2018
*Corresponding author: Deepak Verma, Senior Resident, Department of Otorhinolaryngology, BPS Government Medical College for Women, Khanpur Kalan, Haryana, HUDA sector-7, H.No 312, Gohana, India, Tel: +919899068672; Email: dpkvrm20@gmail.com
How to cite this article: Deepak V, Naveen S, Uma G. Transoral Laser Microsurgery for Isolated Uvula & Soft Palate Malignancy-A Single Centre Experience. Glob J Oto 2018; 14(4): 555891. DOI: 10.19080/GJO.2018.14.555891
Abstract
Objectives:To demonstrate the role and advantages of transoral laser microsurgery (TLM) in the treatment of isolated uvula & soft palate malignancy.
Methods: Prospective review at a tertiary center between 2014 and 2016 included 10 diagnosed and previously untreated patients of isolated uvula & soft palate malignancy. Preoperative evaluation protocol included thorough local examination of oral cavity and oropharynx, 90° laryngeal endoscopic examination and contrast enhanced CT scan (CECT) neck with axial & coronal view to see the extent of growth and cervical nodal metastasis. All biopsy proven patients underwent transoral micro-surgery with CO2 laser under general anesthesia. Tumours were excised taking adequate margins aided by intraoperative frozen section analysis. All patients were sent for postoperative radiotherapy. Patients were kept in regular follow up for a period of 1 year and end points analyzed were local control, locoregional control and overall survival of the patient.
Results: We obtained local control rate of 80% at completed 1 year follow up period. 1 patient refused for radiotherapy and had regional nodal metastasis at 8th postoperative follow up month but still maintaining good local control without any recurrence at primary site. While another patient didn't turn up for follow up so we didn't know the status of recurrence and survival of that patient.
Conclusion: TLM can be an effective approach for the management of oropharyngeal cancer with advantages of low morbidity, short hospital stay, better functional outcomes and disease control which make this an attractive therapeutic strategy of choice these days.
Keywords: Transoral laser microsurgery; CO2 laser; Oropharyngeal cancer; Chemoradiotherapy; Uvula; Soft palate
Introduction
With the advances in new screening and imaging modalities in this era, early diagnosis and treatment of oropharyngeal cancers is done with improved locoregional control and thus survival of patients.
Clinical Relevant Anatomy of Oropharynx
The oropharynx extends from plane of hard palate above to the plane of hyoid bone below. It is bounded anteriorly by the circumvallate papillae and posteriorly by valleculae, lateral walls are composed of the tonsillar fossae with tonsils and muscular pharyngeal wall forms the posterior limits of the oropharynx. For the purposes of management of oropharyngeal tumors, the oropharynx is divided into different subsites: the posterior pharyngeal wall, the soft palate & uvula, the tonsillar complex (i.e. tonsil, tonsillar fossa, and pillars), and the base of the tongue [1]. There are two clinically important potential spaces for tumor invasion surrounding the oropharynx: posteriorly retropharyngeal space and laterally parapharyngeal space.Both of these spaces have significance in treatment implications during surgery or radiotherapy. Extension of disease to the retropharyngeal space increases the chances of contralateral regional metastatic involvement of the neck. Thus in addition to primary site and neck, these potential areas should be included for radiation therapy during management of these cancers [2,3].
Epidemiology and Histological Aspect of Oropharyngeal Tumor
Although majority of primary oropharyngeal tumors are squamous cell carcinomas (SCCs), minor salivary gland tumors (adenomas or adenocarcinomas), primary lymphoid tumors, undifferentiated tumors, sarcomas and mixed cellularity neoplasms are also seen in the oropharynx. Majority (60%) of oropharyngeal SCCs have been found to be moderately differentiated, 20% well differentiated, and 20% poorly differentiated [1]. The incidence of oropharyngeal SCC is closely correlated with dose-dependent use of tobacco and excess alcohol which potentiate the carcinogenic potential of tobacco smoke in the oropharynx. This contributes to the reason that oropharyngeal carcinoma which was earlier seen in people over the age of 45 years, there is an increasing incidence of the disease in people less than 45 years of age [4]. The role of HPV in the oncogenesis of oropharyngeal SCC has also been explained in the literature and majority of HPV-associated head and neck cancers are found to be associated with HPV-16 only. Some authors have also suggested that HPV associated oropharyngeal cancers may be less aggressive and confer better survival than non HPV oropharyngeal cancers [5-7]. The roles of diet and nutritional status in the development of oropharyngeal carcinoma has also been explained, diet high in fruits and vegetables appears to confer a protective effect while malnutrition may increase the risk of oral cancers [4].
Evaluation and Staging of Oral Pharyngeal Tumors
The first step in evaluating protocol is a comprehensive history and detailed local and neck examination, followed by endoscopy and biopsies of suspicious areas. The roles of advanced imaging techniques is very well known in the diagnosis and staging of oropharyngeal cancers. Contrast enhanced computed tomography (CT) scans of the head, neck, and chest region is very beneficial to evaluate local extent of disease, regional and distant metastases and for the assessment of response to therapy and disease recurrence. Another advanced technology is PET scan which has more efficacy than CT scan in the screening of patients of unknown primary with neck secondaries in locating the primary tumor site. MRI is also used in both the staging of oropharyngeal cancers and in surveillance for recurrence with advantages of superior soft-tissue contrast, superior resolution of bone marrow involvement and perineural spread [8,9].
Uvula & soft-palate carcinomas are relatively uncommon (10 times less often than laryngeal and up to 5 times less common than tonsillar carcinomas) but are diagnosed at early stages because of the direct visual inspection and manual palpation of the lesion [9]. These carcinomas are usually asymptomatic until the time of diagnosis. Extent of tumor spread is clinically important regarding overall survival rate, 70.8% for unilateral lesions and this falls to 51% for bilateral or midline crossing lesions. Due to lack of any barriers, these tumors can cross midline or may extend to the tonsillar complex. Despite ipsilateral nodal spread being common, bilateral nodal metastases has been seen in 50% cases in some series of T3 and T4 lesions [10]. Prognoses of soft- palate & uvula carcinomas are directly related to the presence of nodal metastasis, which in turn is related to T stage of the tumor. According to literature, only 20% of T1 and T2 lesions present with nodal metastasis in comparison to 60-70%, seen in T3 and T4 lesions at the time of presentation.
Early T1 and T2 lesions have shown equal rates of local control when treated primarily with either surgery or radiation therapy, being 91-100% for T1 and 70-75% for T2 lesions. In contrast, T3 and T4 tumors appear are best managed by multimodal therapy, surgical resection followed by chemoradiation including chemoradiation in advanced soft-palate & uvula tumors [1]. The attempt at organ preservation by marginal surgery with the use of new technologies such as transoral laser microsurgery (TLM) has emerged these days as a minimally invasive surgical technique for the management of oropharyngeal and laryngeal carcinomas. Contraindications to TLM include inadequate access to the primary site (e.g. trismus), large vessel proximity or involvement (e.g. tumour adjacent to the carotid bulb or internal carotid artery), and oncologic contraindications including T4b cancers, unresectable neck disease or distant metastases. Despite all these limitations, TLM offers potential advantages over open surgery including fewer complications, shorter recovery time and better functional outcomes [11-14]. We thus present here our experience of transoral laser excision of isolated uvula & soft palate malignancy changing the trend of management of these tumors.
Methods
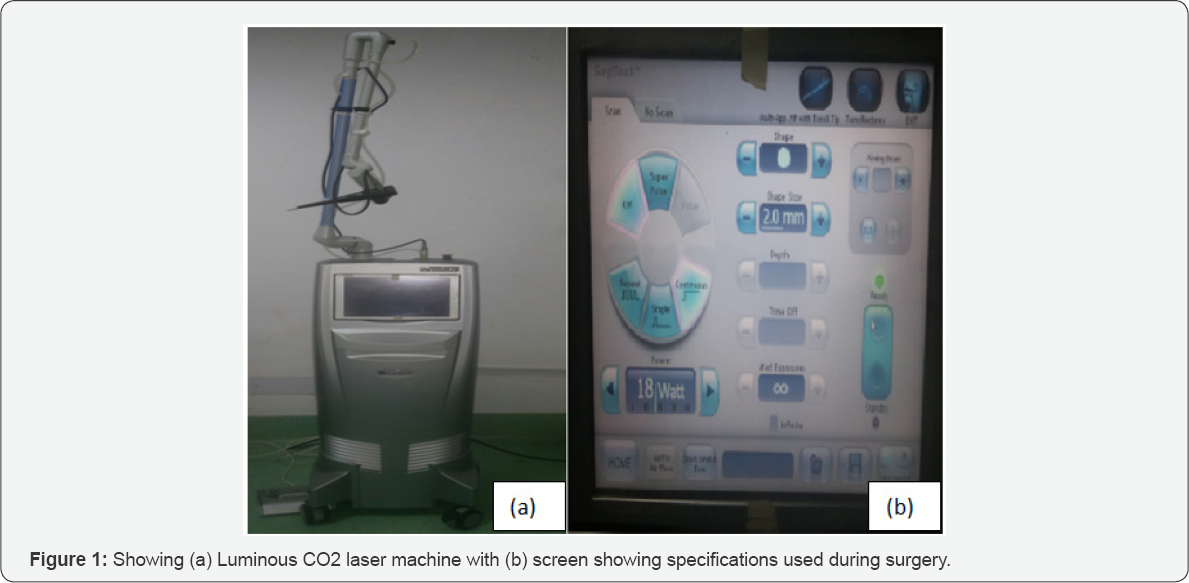
Prospective review at a tertiary center between 2014 and 2016 included 10 diagnosed and previously untreated patients of isolated uvula & soft palate malignancy in age group of 45-95 years. A written informed consent was obtained from all patients before surgery explaining the various available treatment options, possible outcomes and complications. Preoperative evaluation protocol included thorough local examination of oral cavity and oropharynx including digital palpation, 90° laryngeal endoscopic examination, contrast enhanced CT scan (CECT) neck with axial & coronal view to see the extent of growth and cervical nodal metastasis. All patients underwent biopsy from the growth for the confirmation of malignancy. After confirmation, all patients underwent transoral -microsurgery with CO2 laser under general anesthesia with oral intubation using laser endo tracheal tube. Tumours were excised taking adequate margins with CO2 laser (using 18 Watt power, continuous beam with 2mm depth) under all recommended safety precautions (Figures 1-4). The status of margin was determined intraoperative through frozen section analysis and positive margins were subsequently resected until negative margins were obtained. The final resected specimen was sent in toto for histopathological characterization of the tumor. Neck dissection was not done in any of the patient and all were sent for postoperative radiotherapy. Patients were kept in regular follow up for a period of 1 year and end points analyzed were local control, locoregional control, and overall survival of the patient.


Results
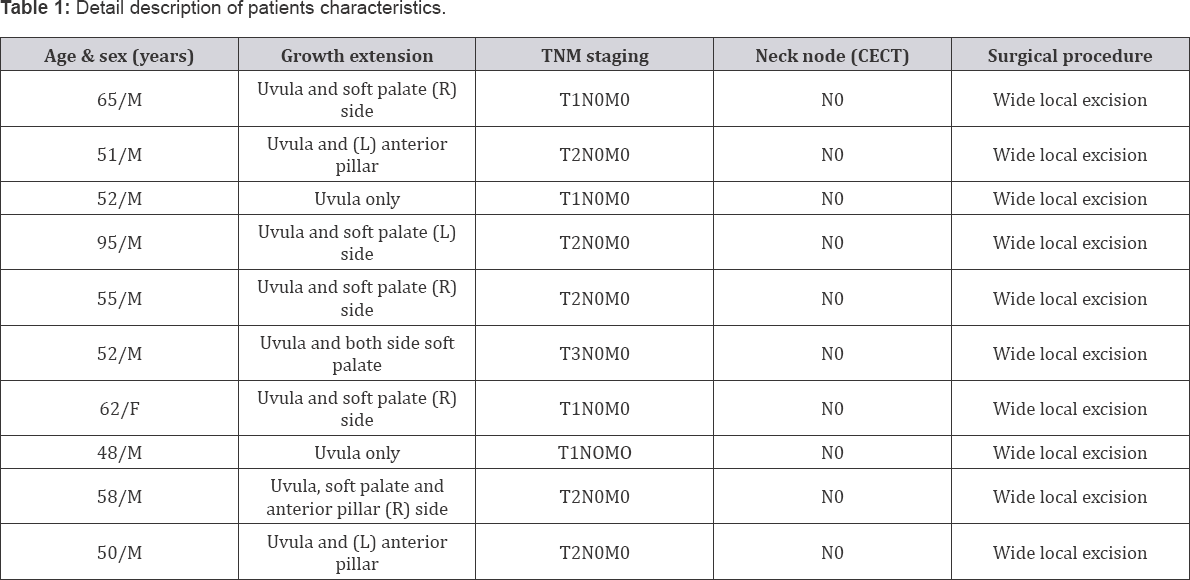
The study included 10 diagnosed patients of isolated uvula and soft palate malignancy in the age group of 45-95 years with mean age of 58.8 years. Out of 10 patients 9 were males and only 1 was female. Patients with trismus, distant metastasis, and poor general condition and with prior history of any form of treatment (surgery or radiotherapy) for aerodigestive tract malignancy were excluded from the study. Contrast enhanced CT scan was done in all patients prior to biopsy for the assessment of extent of growth and cervical nodal metastasis. Clinical staging was done according to TNM staging. Description of patient's data is shown in (Table 1). All patients underwent tumor excision using CO2 laser taking adequate margins. Patients were kept nil per oral for 1 day followed by clear fluids and betadine mouth gargles. All patients were kept for 3 days in the ward except for 1 patient who was 95 years old and was kept under observation in the ward for another 2 days because of intraoperative bleeding, postoperative pain and general condition of the patient.
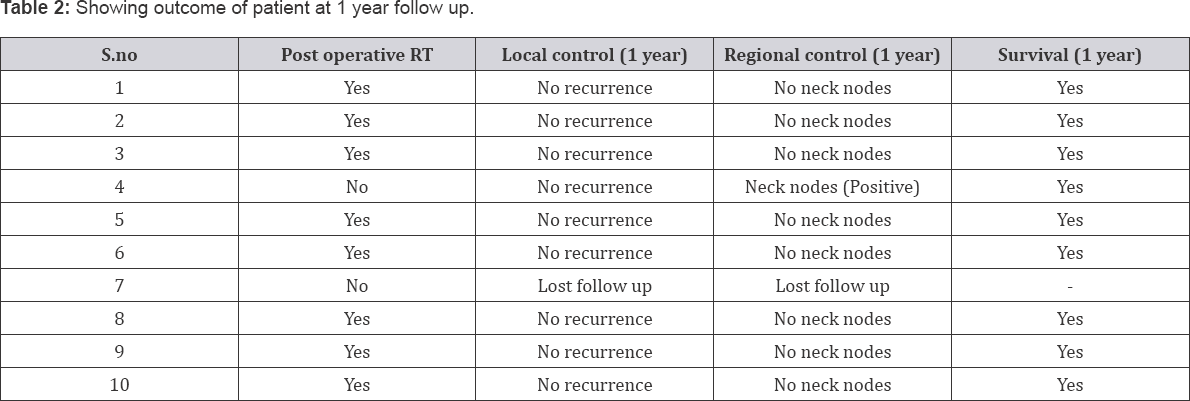
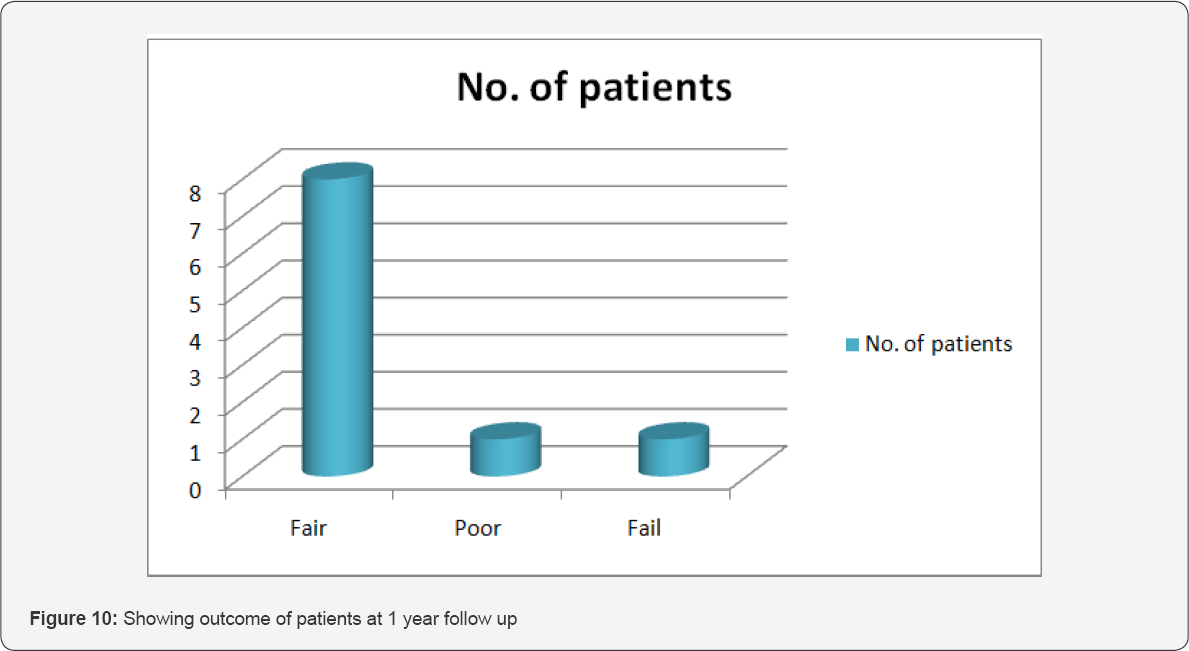
8 out of 10 patients had nasal regurgitation of fluids in postoperative period. The patients were advised to take semisolid or solid foods at home and were educated regarding swallowing techniques to combat the problem of nasal regurgitation. All patients were sent for postoperative radiotherapy and followed up for a period of 1 year at regular intervals for local control, locoregional control, and overall survival of the patient (Table 2). 1 patient refused for radiotherapy and came with unilateral neck nodes at 8th postoperative follow up month which on fine needle aspiration cytology came out as metastatic but still maintaining good local control without any recurrence at primary site. While another patient didn't turn up for follow up so we didn’t know the status of recurrence and survival of that patient. All other remaining patients (success rate of 80%) had good local and locoregional control at completed follow up of 1 year as depicted in Table 2 (Figure 4).
Discussion
The soft palate & uvula are subsites of the oropharynx which allow an individual to perform various functions such as swallowing, speech and breathing by preventing the passage of air or food entry into the nasal cavity. This anatomical barrier and dynamic physiology is altered by the malignant lesions which may develop as space occupying masses altering the normal activity of these structures. The malignancies of these subsites are diagnosed at early stages because of the advantages of direct visual inspection and manual palpation of the lesion. Primary tumors of the soft palate and uvula are rare as com-pared to other oropharyngeal tumors. Earlier, surgical management of these tumors was a matter of debate because of the marked dysfunction resulting from surgical excision of these structures. But in the recent years the availability of new technologies like laser microsurgery has changed the concept of management of these tumors, as reported by Grant, et al. [15] who used laser resection in the treatment of tumors of the oropharynx with encouraging results.
This study found Transoral laser microsurgery as an effective surgical modality for the treatment of T1 to T3 oropharyngeal malignant lesions. In their study, TLM controlled the disease at the primary site in 66 of 69 patients while 3 remaining patients who developed recurrence at the primary site were successfully salvaged with revision TLM. The overall local control rate for T1 and T2 tumors was 90% and 94%, respectively. In the present study we obtained local control rate of 80% for T1- T3 lesions with TLM which is comparable to other similar studies. They have shown in their study that careful tumor assessment, excision with clear surgical margins facilitated with intraoperative frozen sections, can provide improved local control rates for primary site without any dependence on RT as experienced by us also in the present study. Although transoral laser microsurgery has gained popularity these days, literature has reported its implementation in early 1990's with the aim of organ preservation and thus expecting a better quality life [16].
Another study by Rich et al. documented the role of TLM for the treatment of oropharyngeal cancer with improved survival and functional outcomes. The proposed role of TLM in the study was to completely excise the oropharyngeal malignant disease to a negative microscopic margin, so that adjuvant therapy could be directed later on to the high-risk patients. Thus, TLM was found to be a better surgical option for the treatment of primary disease with significant negative margins on survival [17]. Although various studies are available in the literature on the different options for the management of oropharyngeal malignancy, data is lacking on comparison between surgery and other treatment modalities, like chemo or radiotherapy. Concurrent chemoradiotherapy carries significant morbidity in contrast to TLM which carries minimal morbidity and maximal preservation of functions postoperatively [18, 19].
Transoral laser microsurgery with or without neck dissection for oropharyngeal squamous cell cancer has considerable advantages over RT or concurrent CRT including lower morbidity, short hospital stay and acceptability of patient. Transoral laser microsurgery render local and regional disease control as it allows for the precise assessment of tumor depth and infiltration, and the careful margin analysis helps to preserve normal healthy tissue and organ function [20-22].
Conclusion & Recommendations
Transoral laser surgery is a minimally invasive surgical technique for complete resection of the primary tumor with maximum organ preservation of surrounding healthy tissue. This objective is achieved with the use of magnifying microscope and intraoperative frozen section analysis which allow focused and precise excision of the tumor by visualizing the interface between healthy and cancerous tissue, instead of wide field exposure and significant toxicity to surrounding healthy tissues due to high levels of radiotherapy or systemic chemotherapy. To conclude, TLM can be an effective approach for the management of oropharyngeal cancer (particulary soft palate & uvula) with advantages of low morbidity, short hospital stay, better functional outcomes, and better disease control which make this an attractive therapeutic strategy of choice these days.
References
- Osborne RF, Brown JJ (2004) Carcinoma of the oral pharynx: an analysis of subsite treatment heterogeneity. Surg Oncol Clin N Am 13: 71-80.
- Lin DT, Cohen SM, Coppit GL, Burkey BB (2005) Squamous cell carcinoma of the oropharynx and hypopharynx. Otolaryngol Clin North Am 38: 59-74.
- Douglas WG, Rigual NR, Giese W, Bauer J, Wiseman SM, et al. (2005) Advanced soft palate cancer: the clinical importance of the parapharyngeal space. Otolaryngol Head Neck Surg 133: 66-69.
- Gillison ML (2007) Current topics in the epidemiology of oral cavity and oropharyngeal cancers. Head Neck 29: 779-792.
- Puscas L (2005) The role of human papilloma virus infection in the etiology of oropharyngeal carcinoma. Curr Opin Otolaryngol Head Neck Surg 13(4): 212-216.
- Fakhry C, Gillison ML (2006) Clinical implications of human papillomavirus in head and neck cancers. J Clin Oncol 24: 2606-2611.
- Monk BJ, Tewari KS (2007) The spectrum and clinical sequelae of human papillomavirus infection. Gynecol Oncol 107: 6-13.
- Scully C, Bagan JV (2008) Recent advances in oral oncology 2007: imaging, treatment and treatment outcomes. Oral Oncol 44(3): 211215.
- Jamerson RE, White JA (1991) Carcinoma of the soft palate and uvula. J La State Med Soc 143(2): 7-9.
- Weber AL, Romo L, Hashimi S (2003) Malignant tumors of the oral cavity and oropharynx: clinical, pathologic, and radiologic evaluation. Neuroimaging Clin N Am 13: 443-464.
- Rich JT, Milov S, Lewis Jr JS, Thorstad WL, Adkins DR, et al. (2009) Transoral laser microsurgery (TLM) +/- adjuvant therapy for advanced stage oropharyngeal cancer: outcomes and prognostic factors. Laryngoscope 119(9): 1709-1719.
- Weinstein GS, O'Malley BW Jr, Rinaldo A, Silver CE, Werner JA, et al. (2015) Understanding contraindications for transoral robotic surgery (TORS) for oropharyngeal cancer. Eur Arch Otorhinolaryngol 272(7): 1551-1552.
- Sinha P, Hackman T, Nussenbaum B, Wu N, Lewis Jr JS, et al. (2014) Transoral laser microsurgery for oral squamous cell carcinoma: oncologic outcomes and prognostic factors. Head Neck 36(3): 340-351.
- Williams CE, Kinshuck AJ, Derbyshire SG, Upile N, Tandon S, et al. (2014) Transoral laser resection versus lip split mandibulotomy in the management of oropharyngeal squamous cell carcinoma (OPSCC): a case match study. Eur Arch Otorhinolaryngol 271(2): 367-372.
- Grant DG, Hinni ML, Salassa JR, Perry WC, Hayden RE (2009) Oropharyngeal cancer: a case for single modality treatment with transoral laser microsurgery. Arch Otolaryngol Head Neck Surg 135: 1225-1230.
- Sutter R, Grossenbacher R (1990) Resection of palatal tumours with the CO2 laser. J Laryngol Otol 104: 20-23.
- Rich JT, Milov S, Lewis JS Jr, Thorstad WL, Adkins DR, et al. (2009) Transoral Laser Microsurgery (TLM) ± Adjuvant Therapy for Advanced Stage Oropharyngeal Cancer: Outcomes and Prognostic Factors. The Laryngoscope 119(9): 1709-1719.
- Nguyen NP, Vos P, Smith HJ, Nguyen PD, Alfieri A, et al. (2007) Concurrent chemoradiation for locally advanced oropharyngeal cancer. Am J Otolaryngol 28(1): 3-8.
- Urba SG, Moon J, Giri PG, Adelstein DJ, Hanna E, et al. (2005) Organ preservation for advanced respectable cancer of the base of tongue and hypopharynx: a southwest oncology group trial. J Clin Oncol 23(1): 88-95.
- Steiner W, Fierek O, Ambrosch P, Hommerich CP, Kron M (2003) Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue. Arch Otolaryngol Head Neck Surg 129(1): 36-43.
- Grant DG, Salassa JR, Hinni ML, Pearson BW, Perry WC (2006) Carcinoma of the tongue base treated by transoral laser microsurgery, part one: untreated tumors, a prospective analysis of oncologic and functional outcomes. Laryngoscope 116(12): 2150-2155.
- Thomas L, Jones TM, Tandon S, Carding P, Lowe D, et al. (2009) Speech and voice outcomes in oropharyngeal cancer and evaluation of the University of Washington Quality of Life speech domain. Clin Otolaryngol 34(1): 34-42.





























