Malignant External Otitis-Case Report
Cristina Otilia Laza Mostafa Sarv*
ENT /OMF Clinic Scju, Sf Apostol Andrei Constanta, Romania
Submission: March 26, 2018; Published: April 06, 2018
*Corresponding author: Cristina Otilia Laza Mostafa Sarv, ENT /OMF Clinic Scju, Sf Apostol Andrei Constanta, Romania, Email: cristinaotilia@gmailjCom
How to cite this article: Cristina O L M S. Malignant External Otitis-Case Report. Glob J Oto 2018; 14(3): 555889. DOI: 10.19080/GJO.2018.14.555889.
Abstract
The purpose of this paper work is to share our attitude and results in the diagnosis and treatment of external malignant otitis by presenting a case diagnosed and treated. In our clinic .We have a typical case of malignant external otitis, a severe bacterial infection, caused by Pseudomonas aeruginosa, in an elderly diabetic patients with renal failure also .We start with a complete ENT clinical exam, with otoscopy-endoscopy, microscopic exam, also with lab test to evaluate the general status of our patient, microbiology to identified the germ and his response to antibiotics [1]. Also is recommended to check for osteomyelitis of the temporal bone ,best it's to start with a CT scan to see the extension of the process, abscess locations, endocranial complications .But most evident, inflammation of the connective tissue , muscles, fat, bone, cartilage are visible on MRI.
We treat our patient with long-term courses of antibiotics, general and local, every day local treatment with aspiration of puss from de EAC, lavage with peroxide, or betadine. Also on the microscope we remove the polyps from the EAC, also we drain peri auricular abscesses and a temporal epicranial abscess .Step by step with the help of the currant nephrologist, and diabetologist the process start to heal, with no complications .After a period of 3 months we repeat MRI and the patient was completely cured. The rest of the paper work we compare this case with others and we review the literature.
Keywords: Malignant external otitis; Diabetes mellitus; Renal failure; Immuno suppression; osteomyelitis al the skull base; Epicranial abscess
Case Report
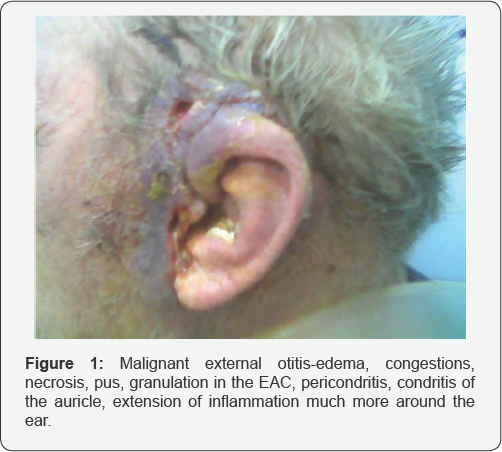
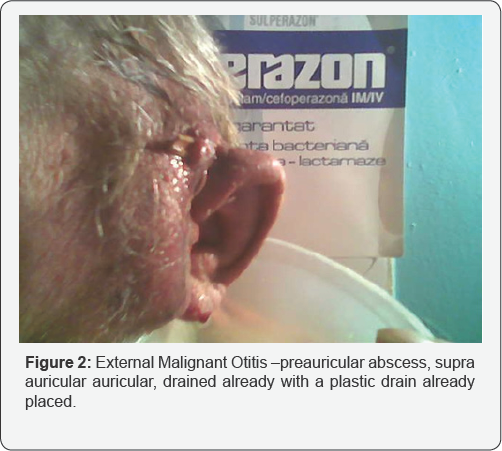
An 85 years old man , was admitted in our Clinic for severe pain in the left ear extended temporal and retroauricular in the -mastoid area and preauricular, starting 3 weeks ago ,after a trauma of the EAC -with a pointed instrument-toothpick for a chronic pruritus accused by the patient but neglected by the family. Suddenly starts otalgia, pain more and more intense, edema, congestion of the meatus of EAC but rapidly the entire auricle became thick ,enlarged red ,very painful (Figure 1). The process also extend posterior on the mastoid and occipital area, superior temporal, anterior tumefaction of the TMJ and parotid gland area. The discharge from the ear became green, purulent fetid ,areas of red-violet portions of the skin appear in a few areas .On that time general status of the patient deteriorate with fever low, asthenia , insomnia, lying in bed (Figure 2).
At the presentation we examine a febrile, confuse, dezoriented old men, with a pale suffering face, responded late to verbal stimuli. His anturaj, describe the debut and his actual status, also chronic illness like diabetes, renal failure., arterial hypertension, Atrial Fibrilation. On the right side of the head entire temporo-mastoid-parotid area was bulging edematous,red, the auricle is very thick because of an edematous perichodritis. External acoustic meatus is almost inexistent because of the inflammation of the walls of the channel [2]. The same lesion are on the internal surface of the auricle but also with extension posterior on the mastoid process till the occipital, superior temporal anterior -preauricular, quite in the parotid gland area. Palpation-the entire area was very painful and lymph nodes enlarged and sore. Retroauricular on the mastoid process there is an area of bulging with auricle pushed anterior .On small area there is a purple area with a fistula 1mm diameter and a purulent thick, fetid, yellow-green discharge, stained with blood.
Laboratory Test
a) CBC neutropenia, anemia -PCR high level
b) Fibrinogen, erythrocyte sedimentation rate (ESR) high
c) Exploring metabolism- glucose level -was very high ,liver ,kidney function-high Creatinine, reveal the important dezechilibriium
d) Microbiological exam of the pus -before topical or systemic antibiotic therapy is started, ear secretions should be cultured, and antibiotic sensibility tested.
e) Biopsy of the granulation from the EAC -differential diagnosis with cancer -Rx thorax
f) Rx cranium profile
g) Rx mastoid -views Schuller , Stenvers, Chause III
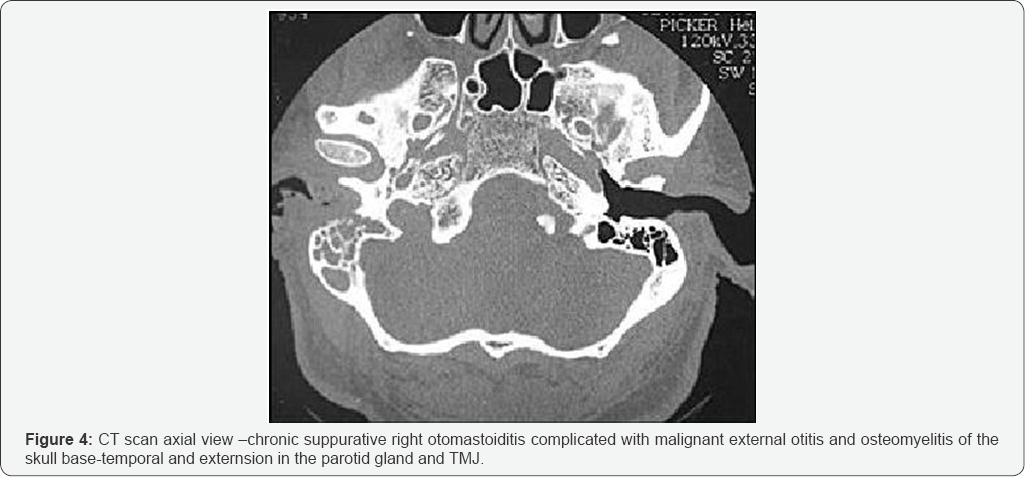
h) CT scan -extension of the inflammatory process, abscesses, and of the EAC, no osteomyelitis or endo-cranial lesions visible.
Treatment
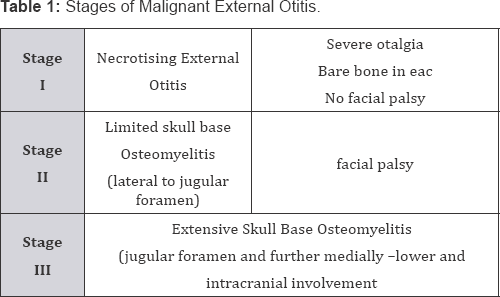
Medical treatment -complex general for all the diseases ,and antibio-therapy with cephoperasone plus sulbactam and netromycine with low doses initial because of poor kidney function Surgical treatment-every day aspiration of pus from EAC ,washout the pus with peroxide, small dressing soaked in sol with local antibiotic like ciprophloxacine, to bramycine or betadine and local drops 3 times on the day Also we drain all the abscesses ,explore the cavity ,but the periosteal layer was intact ,washout with peroxide and saline, also we place drains [3-6]. Step by step after 5 weeks of intense treatment the ear was clean, large, all the surrounding infected tissues clean and incision healed. We discharge the patient with all the recommendation required, for nutrition, way of life, and strict treatment, of diabetes and renal failure with local treatment for otomycosis and recommendation for follow-up. The evolution was good, at 3 month an MRI for control infirm osteomyelitis of the temporal bone (Table 1).
Malignant external otitis or necrotizing external otitis is a life threatening, progressive bacterial infection of the external auditory canal, mastoid and skull base. It most commonly occurs in elderly diabetics or in an otherwise immune-compromised host Osteitis of the temporal and adjacent bones was initially described in 1959 by Meltzar and Kelemen. Because of the high mortality rate (46 %) in early series, this condition is often referred to as "malignant otitis external otitis. It is also called "necrotizing external otitis," a term sustained by Chandler in 1968 that emphasizes the destructive nature of the infection.
"Osteitis of the base of the skull," the most recent but less popular name for this condition, stresses the involvement of bone and the strategic location of the infection.Because of significant differences in natural course and treatment, it is crucial to differentiate severe external otitis and necrotizing external otitis. Involvement of structures beyond the soft tissues of the auditory canal occurs only in necrotizing external otitis [7-9]. Osteitis of the base of the skull usually follows external otitis but also may begin with a middle-ear infection. Although necrotizing external otitis can occur in immune-competent persons, it typically develops in persons with diabetes mellitus or another condition that compromises the immune system, such as acquired immunodeficiency syndrome, malignancy, or chemotherapy.
Pathogenesis and Clinical Manifestations

The process starts with an external otitis -Infection of the soft tissue of the external auditory canal ("swimmer's ear") is common, especially in hot, humid climates, after minor repeated trauma for pruritus I the channel with cotton swabs, or sharp objects or and exposure to swimming-pool water, which has a high concentration of pathogens, also a foreign body left in EAC -most frequent cotton. Rare the origin is an acute or chronic suppurative otomastoiditis (Figure 3). The most frequently cultured pathogen, Pseudomonas aeruginosa, is not a normal inhabitant of the auditory canal. Other possible pathogens include Staphylococcus epidermidis, aureus gram-negative bacteria, and fungus like Aspergillus Niger, flavus, fumigatus, Candida albicans.
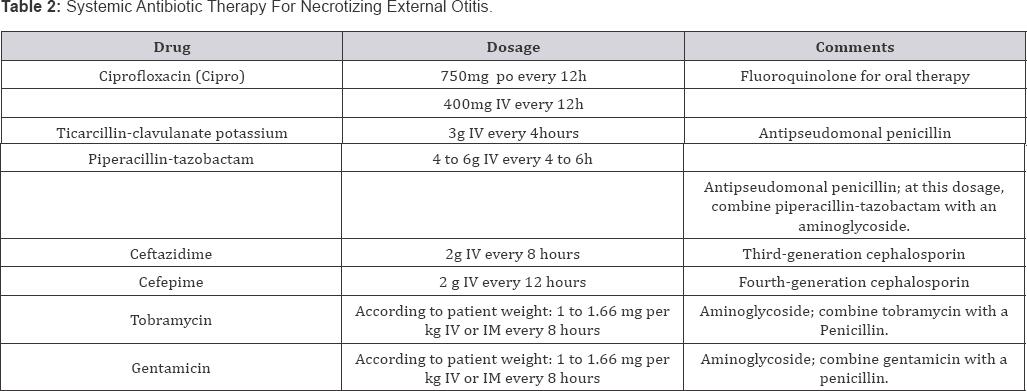
Although necrotizing external otitis can occur in immune- competent persons, it typically develops in persons with diabetes mellitus or another condition that compromises the immune system, such as acquired immunodeficiency syndrome, malignancy, or chemotherapy. In diabetes mellitus, poor vascular supply resulting from microvascular disease is aggravated by Pseudomonas vasculitis, which further restricts tissue perfusion [10]. Diabetes mellitus is also associated with impaired polymorphonuclear cell function and a higher pH of cerumen in the aural canal (Figure 4). These factors, along with the sensitivity of P. aeruginosa to low pH, further restrict bodily defenses against infection. Patients with osteitis of the base of the skull sometimes have extra-auricular manifestations, such as cervical lymphadenopathy, inflammation of the parotid gland. Trismus (because of temporo-mandibular joint involvement),or irritation of the masseter muscle (Table 2).
Note: Culture should be performed before systemic antibiotic therapy is initiated.
As the infection spreads in the temporal bone, it may extend into the cranium and result in cranial nerve palsies. These palsies generally are caused by the secretion of neurotoxins or the compressive effect of the destructive process through the relevant foramina. Because of its anatomic location in the temporal bone, the facial nerve is usually the first nerve to become involved. Cranial nerve involvement indicates a poor prognosis. Death is usually due to intracranial complications such as sigmoid sinus thrombosis, but it also may occur because of treatment complications, including bone marrow suppression induced by long-term antibiotic therapy [11]. Prognosis is adversely affected by comorbid conditions, which are common in patients who develop malignant external otitis.
Patients with external otitis complain of otalgia and sensitivity to auricular movement. Otorrhea may be present, and obliteration of the external auditory canal by edema and secretions may cause hearing loss or a sensation of fullness in the ear. Oedema with erythema of ear canal is common. However tympanic membrane is usually intact. The infection may extend to the cartilaginous skeleton of the ear canal and through Santorini's fissures to reach the temporal bone, causing osteitis. One of the hallmarks of this extension is granulation tissue in the bone-cartilage junction of the external auditory canal. This otoscopic finding is of extreme importance.
Diagnosis
Family physicians should maintain a high index of suspicion for necrotizing external otitis in immune-compromised patients who have external otitis. Special alertness is required when external otitis is refractory to treatment and patients complain of severe otalgia, especially at night. The diagnosis of necrotizing external otitis is based on the clinical presentation and confirmed by laboratory tests and imaging studies.
Laboratory Tests
a) Bacteriological, mycological exam of the pus and culture in almost all cases reveals Pseudomonas aerogenosa. Occasionally Staphylococcus aureus and anaerobic bacteria has been reported.
b) CBC-anemia, neutropenia /leukocytosis
c) Metabolic parameters, liver, renal function must be checked -erythrocyte sedimentation rate (ESR), white and red blood cell counts.
d) Glucose and Creatinine levels and culture of ear secretions. The ESR is typically elevated in necrotizing external otitis; therefore, it is a useful indicator of treatment response. Before topical or systemic antibiotic therapy is started, ear secretions should be cultured, because susceptibility patterns may change after the initiation of treatment (i.e., bacteria might become resistant to an antibiotic during treatment.
e) Biopsy of the granulation tissue removed from the external auditory canal is essential to exclude a malignant processes or a Wegener granulomatosis.
Imaging Studies: Conventional radiography plain x-rays Schulller, Stenvers provides insignificant information about malignant otitis externa. Significant demineralization of the base of skull must occur before any changes are seen on plain film. CT scanning is used to determine the location and extent of diseased tissue .The temporal bone is the first bone to be affected, with imminent involvement of the petrous apex and mastoid. Extratemporal bone extension has become rare since the introduction of powerful antibiotics. In evaluating the CT scan, it is important to remember that at least one third of bone mineral must be lost before radiologic changes become apparent; conversely, bone remineralization continues long after the infection is cured. Thus, as related to the infectious process, pathology is late to appear on the CT scan and late to disappear. These factors limit the usefulness of CT scanning as a follow-up tool.
Scintigraphy of the bone
a) Both osteoclasts and osteoblasts absorb 99mTc. Hence, bone scanning can locate a pathologic process in bone but is not informative about the nature of the process (infectious or other). Because the 99m Tc scan remains positive as long as bone repair continues, this imaging modality is not helpful in follow.
b) Since 67Ga is absorbed by macrophages and cells of the reticulo-endothelial system, scanning with this radioisotope is a sensitive measure of ongoing infectious process.
c) Scintigraphy with 67Ga, can be used for initial diagnosis and as a follow-up method. -MRI -contrast iv -best to revealed inflammations
d) Imaging to prove the extension of infection to bony structures is generally necessary to establish the diagnosis of necrotizing external otitis MRI is more available and easy to use with a good resolution of soft tissues and inflammation.
Differential diagnosis
a) Severe external otitis and necrotizing external otitis.
b) Osteitis of the base of the skull in a middle-ear infection.
c) Cancer of the EAC, parotid gland or middle ear infected -Tuberculosis of the parotid or ear.
Complications
Progressive skull base osteomyelitis can result in
a) CN VIII--Facial nerve paralysis being the most common.
b) CN IX,X,XI palsy (Jugular foramen syndrome)
c) CN XII (hypoglossal canal) are less often involved.
d) Thrombosis of lateral sinus, superior and inferior petrous sinuses.
e) Secondary osteomyelitis at the petrous apex can spread to the floor of the middle cranial fossa or the bazi-sphenoid with the development of sphenoidal sinusitis.
f) Meningitis
g) Abscesses-extradural ,near the process, subdural- after meningitis ,cerebral-temporal ,multiple-hematogenic spread, cerebellar
h) Epicranial abscesses
i) Condritis supurative with deformation of the auricles
j) Deafness
k) Osteomyelitiis of the skull base
l) Osteitis of the TMJ with distruction
m) 13.Extension on the parotid gland with abscess fistulisation in the EAC
Prevention: In many patients with necrotizing external otitis, the initiating event may be self-inflicted or iatrogenic trauma to the ear canal. Therefore, susceptible patients should be instructed to avoid manipulation of the external auditory canal (i.e., they should not use cotton swabs to remove cerumen). Cleaning of the external auditory canal, including aural irrigation by medical staff, should be carried out with extreme caution to avoid injuring delicate skin in the canal. Eczematous conditions involving the meatus of the canal should be treated topically, because these conditions may result in pruritus that leads to scratching of the irritated skin .Prognosis seems to be related directly to the stage that the disease has reached at the onset of treatment. This in turn requires great awareness of the condition.
Treatment: Treatment of necrotizing external otitis includes correction of immunosuppression (when possible), local treatment of the auditory canal, long-term systemic antibiotic therapy and, in selected patients, surgery. Strict control of diabetes mellitus is mandatory, although it can be difficult to achieve during the acute illness, usually the patients is treated with Insulin Act rapid to maintain the level of glycaemia .Other immunosuppressive states and comorbid conditions also must be aggressively managed. Ex dialysis for renal failure, neupogen in neutropaenia. Local treatment of the auditory canal includes meticulous cleaning and debridement plus topical application of antimicrobial agents (antibiotics and others). Sequesters and other necrotic tissue should be removed. Initially, treatment may include the application of antimicrobial-impregnated dressings to the canal.
An anti-Pseudomonas agent should be used first; if necessary, the agent can be changed on the basis of the culture results. As in other infections involving bone, longterm administration of systemic antibiotics is the mainstay of treatment. The introduction of antipseudomonal agents in the 1980s simplified the ambulatory treatment of osteitis of the base of the skull. Fluoroquinolones, primarily ciprofloxacin and ofloxacin, are DNA-gyrase inhibitors that are effective against P. aeruginosa and well tolerated by patients. Poor vascularization of the target area is one of the reasons that high-dose antibiotic therapy is needed to treat malignant external otitis. For ex, the dose of ciprofloxacin is 750 mg x2 /day. Treatment should be continued for at least four weeks, but the duration of therapy must be individualized on the basis of the clinical presentation (night pain, physical findings), ESR, and imaging studies.
Recurrence is a well-recognised aspect of this disease and is usually manifested by insidious onset of otalgia followed by headache and tempero-mandibular joint pain. High mortality rate reported in initial studies (37% by Chandler, 1977) have steadily decreased with the development of potent antipseudomonal antibiotics. Other antibiotics that are effective against P. aeruginosa include aminoglycosides, penicillin (especially piperacillin-tazobactam), ceftazidime cefepime and, occasionally, imipenem. Depending on bacterial sensitivity, a combination of agents may be needed. One common combination is antipseudomonal penicillin and an amino-glycoside. Hyperbaric oxygenotherapy, an adjunct to antibiotic therapy, is believed to increase the ability of polymorphonuclear cells to fend off pathogenic bacteria but administration is difficult and the procedures are very expensive.
Surgery has a definite but increasingly limited role in the treatment of osteitis of the base of the skull. Although bone sequesters and abscess is treated surgically, further extension of the operation may be counterproductive because it may expose healthy bone to the infection. In case of otomastoiditis mastoidectomy.
Discussion
In my entire carrier I treat 5 patients with malignant external otitis All have immune-depression, 4 patients were with diabetes mellitus at varying levels of control. One with chronic renal failure also and the last, was a non-diabetic young lady with AIDS discovered with the severe disease, with no obvious predisposing factor.
a) 3 cases starts classical as an initial otomycosis with pruritus infected because of abusing scratch with external otitis and extension periauricular.
b) 1 case was a chronic otomastoiditis complicated after activation-water protruded in the EAC with malignant external otitis and skull base osteitis of the temporal bone but also TMJ and involvement of the parotid gland
c) 1 case was an acute otomastoiditis complicated with retroauricular abscess and facial palsy -in an young lady who proved to be in the final stages of AIDS unknown, probably taken 10-15 years ago after transfusions-she suffer from Thrombocytopenia idiopathica.
d) In 4 cases the complete healing was possible but the lady with AIDS died though prolonged antibiotic treatment and surgical debridement were efficient in 4 cases but radical mastoidectomy was necessary in two cases .In case of the lady with AIDS, complications after the surgery, starts immediately one by one with facial palsy, dehiscence of the retro-auricular inc ision with necrosis of the tissues including pericondritis, condritis of the auricle.
Conclusion
i. Malignant external otitis, a morbid osteomyelitis of external auditory canal, mastoid and skull base caused by Pseudomonas aeroginosa is always related with immunosuppression.
ii. Classic is an old patient with diabetes mellitus, but other organ failure or chemotherapy in treatment for cancer, immunosuppressive treatment like corticotherapy after large organ transplant are other possibilities including infection HIV.
iii. In diabetes is important poor vascular supply, as a root pathogenic factor, but also the function of neutrophils is impaired and Ph of cerumen is acid.
iv. In most cases is an infection with Pseudomonas aerugiosa -known to induce vasculitis, but Staphilococus aureus or a fungus like Aspergillus or Candida are discovered in the pus-microbiology-cultures and sensibility to antibiotics test are essential.
v. An early diagnosis with a high index of suspicion and an aggressive treatment with wide local excision if required, debridement and prolonged antibiotic therapy usually proves successful.
vi. Extremely severe morbidity -The pain was severe, kept on fluctuating and was not fully relieved even after treatment. Recurence of osteitis and slow extension requires
vii. A long antibiotherapy and periodic MRI-repeated to expose osteitis.
viii. Mastoidectomy was required in case of otomastoiditis complications but difficult to realized in decompensated diabetes, neutropenia, anaemia, trombopenia .
ix. After the surgical intervention, the cavity became fairly dry with epithelialization very difficult, usually dehiscence of wound, granulation of inflammatory tissue and extension of osteomyelitis is frequent.
x. For this reason is very important the general support ,insulin therapy, transfusions of blood, platelet cells, Neupogen-to stimulate production of neutrophils in case of neutropenia. This experience must be shared with the physicians treating diabetes, or oncology-haematology, rheumatology, immunology specialists
xi. Very high index of suspicion in elderly diabetics or otherwise immune-compromised patients presenting with earache can help in early diagnosis and early referral before the development of facial palsy and thus decreasing the morbidity.
xii. This highlights the need for increasing the awareness regarding the condition especially among non-otologists.
References
- Babistzki A, Sade J (1987) Malignant external otitis. Journal of otolaryngology 101(3): 205-210.
- Chandler JR (1968) Malignant external otitis. Laryngoscope 78: 12571294.
- Chandler JR (1977) Malignant external otitis, further considerations. Annals of otology, Rhinology and laryngology 86: 417-428.
- Gherini SG, Brackman DE, Bradley WG (1986) Magnetic resonance imaging and computerised tomography in malignant external otitis. Laryngoscope 96(5): 542-548.
- Meltzer PE, Keleman G (1959) Pyocutaneous osteomyelites of the temporal bone, mandible and zygoma. Laryngoscope 69(10): 13001316.
- Mills (1986) Malignant otitis externa. British Medical Journal 292: 429-430.
- Morrison GA, Bailey CM (1988) Relapsing malignant otitis external successfully treated with ciprofloxacin. J Laryngol Otol 102: 872-876.
- Rubin J, Yu VL (1988) Malignant external otitis: insights into pathogenesis, clinical manifestation, diagnosis and therapy. The American Journal of Medicine 85(3): 391-398.
- Scully BE, Neu HC, Parry MF (1986) Oral ciprofloxacin therapy of infection due to pseudomonas aerogenosa. Lancet 1(8485): 8192 -822.
- Shpitser T, SternY, Cohen O (1993) Malignant External Otitis in Non diabetic patients. Annals of Otology, Rhinology, Laryngology 102: 870872.
- Thakar A, Kacker SK, Bahadur S (1996) Malignant external otitis. Indian Journal of Otolaryngology and Head and Neck surgery 48(2): 114-120.





























