Videolaryngoscope Assisted Fiberoptic Bronchoscopy for Difficult Intubation in Upper Airway Cancer
Francisco OM Vieira1, Cecil B Rhodes2, Aaron Smith2 and Shannan Case CRNA3
1Assistant Professor of Otolaryngology - Head and Neck Surgery, University of Tennessee Health Science Center at Memphis, USA
2Department of Otolaryngology - Head and Neck Surgery, University of Tennessee Health Science Center, USA
3Certified Registered Nurse Anesthetist, University of Tennessee Health Science Center, USA
Submission: March 20, 2018; Published: April 06, 2018
*Corresponding author: Cecil B Rhodes, Department of Otolaryngology - Head and Neck Surgery, University of Tennessee Health Science Center, Memphis, Tennessee, USA, Email: asmit286@uthsc.edu
How to cite this article: Francisco O V, Cecil B R, Aaron S, Shannan C C. Videolaryngoscope Assisted Fiberoptic Bronchoscopy for Difficult Intubation in Upper Airway Cancer. Glob J Oto 2018; 14(3): 555888. DOI: 10.19080/GJO.2018.14.555888.
Abstract
Objectives: We present a combined method of videolaryngoscope assisted fiber optic bronchoscopic intubation "VLS/FOBI” for head and neck cancer patients presenting with upper airway obstruction who would otherwise undergo initial awake tracheostomy.
Methods: 16 patients presenting with stage III and IV laryngeal, hypopharyngeal and thyroid tumors who were anticipated to be difficult intubations are studied. A combined use of broad view from videolaryngoscope (VLS) assisted by fiber optic bronchoscopic intubation (FOBI) is described. Exposing available supraglottic landmarks allows for proper positioning of fiberoptic flexible bronchoscope to be advanced through the vocal cords and confirmed visually.
Results: In this cohort 16 out of 38 patients with head and neck cancers met the inclusion criteria, 5 (31%) patients although considered for the technique were not attempted. The remaining 9 (69%) patients underwent the VLS/FOBI procedure and resulted in successful intubations at first pass without any complication.
Conclusion: Advanced head and neck cancer patients can require expedited awake surgical procedures due to the inability to secure the airway, which leads to increased risks for complications. However, VLS/FOBI when feasible is easily performed, efficient, and decreases the need for awake tracheostomy. The equipment is readily available and requires no more time than the standard intubation.
Keywords: Videolaryngoscopy; Videolaryngoscope; Fiberoptic Intubation; Fiber optic Bronchoscopic Intubation; Awake Tracheostomy; Difficult Airway Intubation
Introduction
Recent publications have shown evidence that use of high resolution digital video laryngoscope (VLS), when compared to conventional direct laryngoscope (DL), is superior when managing difficult airways in elective and emergency settings [1,2] In a large-scale multivariate model Mosier J et al. [3] compared VLS alone to DL with a MacIntosh blade for difficult airway management in the emergency department. VLS appeared to be superior to DL for these cases, improving visualization of true vocal cords and increasing efficacy of tracheal intubation. In terms of success rates for rescue attempts, VLS and DL were equivalent [3]. VLS has been successfully used in assisting rigid bronchoscopic endotracheal in obstructing endotracheal neoplastic process for direct stent placement [4].Complex analyses have developed predictors that can contribute to a challenging airway resulting in a difficult or failed airway intubation. However, they are far from practical and have a limited role for routine clinical use.
This limited use is due to the subjective and/or objective variation in personal skills and different interpretations of a patient's airway for the same predictive model [5,6]. Even though a thorough preoperative assessment, complications cannot be avoided in many cases and all necessary resources are vital in managing unanticipated difficult airways [7]. The fiberoptic bronchoscope alone has restrictions and may be limited in its use. It offers a narrow frontal view of airway structures. Also, the primary operator has full control over the procedure and the assistant is restricted to providing only limited help. Furthermore, skill and time management place restrictions on the use of the fiberoptic intubation due to rapid oxygen desaturation in patients with other associated hemodynamic and respiratory related comorbidities [8].
Contraindications to attempting fiberoptic bronchoscope intubation include patients with total laryngeal obstruction such as malignant lesions, airway bleeding, or laryngeal injury and is relatively contraindicated in patients with moderate subglottic stenosis or facial trauma with active oropharyngeal bleeding. Failure of an endotracheal intubation on a difficult airway typically results in cricothyroidotomy or awake tracheostomy. These options are known to have substantially increased risk of morbidity and mortality, with complications occurring in about 7% to 8% for this group of patients [9-15]. A combined intubation technique using fiberoptic bronchoscope intubation assisted via video laryngoscope (VLS/FOBI) for difficult airways was previously described in the literature in 2004 by Doyle [8]. The combination of these two tools increases the visualization of airway anatomy and can potentially alleviate some of the risk in difficult airway intubation.
Procedure
Following standard monitoring and pre-oxygenation general anesthesia is induced by a hypnotic and a neuromuscular blocking agent followed by mask ventilation. The technique is performed by two operators; one principal operator and one assistant operator. The VLS is introduced by the assistant operator for a broad inspection of the area, followed by introduction of the fiberoptic bronchoscope (Olympus 5.1mm fiberoptic bronchoscope LF-DP, Tokyo, Japan) with an endotracheal tube placed over the scope. The flexible bronchoscope is used as a stylet for the endotracheal tube and the eyepiece should be preferentially connected to a monitor, providing an accessory view to the anatomy to all assistants involved in the intubation process [9]. While the assistant gently introduces an adequate blade size to manipulate and position the VLS to appropriately identify key visible landmarks (epiglottis, arytenoids, false vocal cords and true vocal cords), the operator then introduces the fiberscope mounted with the endotracheal tube and advances it toward the area in which the vocal cords are located.
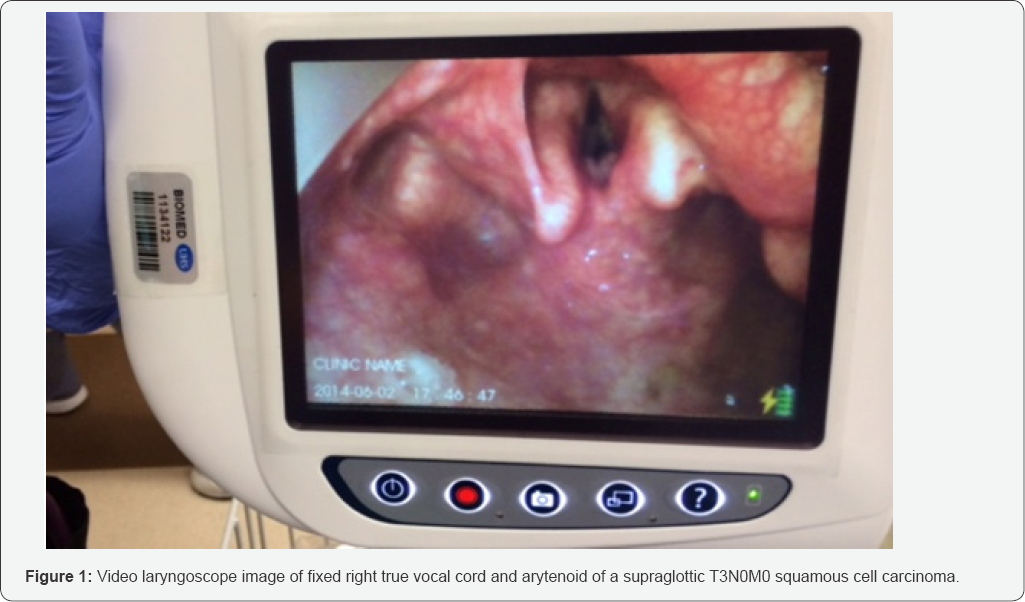
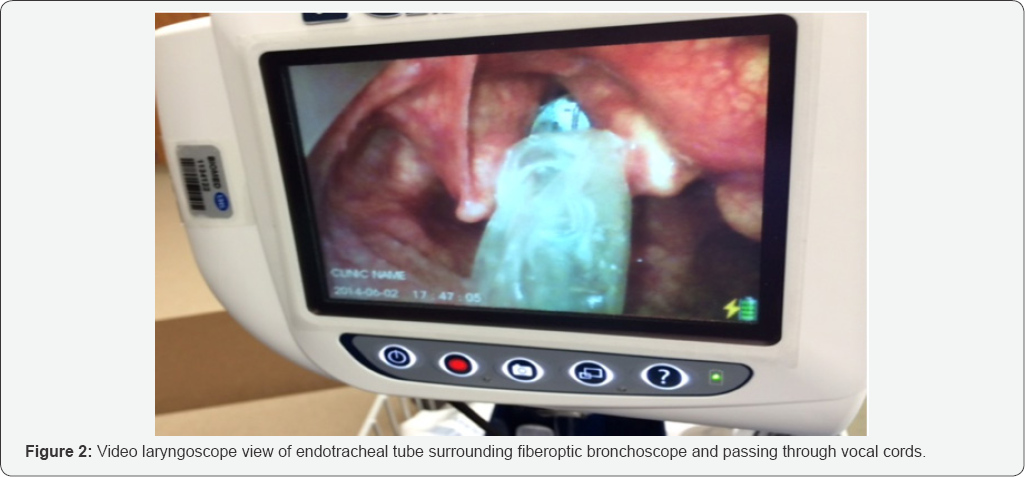
When the tip of the scope has passed through the vocal cords and placement into the trachea is visually confirmed, the endotracheal tube is cautiously advanced into the glottis. The wide view of 50 degrees from the VLS based on the available supraglottic landmarks allows for monitoring and easy correction of the narrower view from the bronchoscope, especially when any misdirection due to advancing towards the piriform sinus and esophagus. After the endotracheal tube advancement through the vocal cords, correct placement is confirmed by direct visualization and the flexible scope and VLS are carefully removed. The supraglottic view provided by the VLS both before and during insertion of the endotracheal tube is shown in (Figures 1 & 2).
Methods
This study was approved by the Institutional Review Board and included 16 out of 38 laryngeal, hypo pharyngeal and thyroid cancer patients spanning a period from 2012 to 2016 who planned to undergo attempted intubation via VLS/FOBI for stage III and IV laryngeal cancer with extension to hypopharynx or hypo pharyngeal cancer extending to the larynx or thyroid cancer with compression/invasion of airway who were anticipated to be a difficult intubation and had agreement by anesthesiology for the procedure. These patients also must have had a CT scan and were undergoing recent laryngoscopy exam and biopsy followed by tracheotomy. We excluded twenty two (58%) patients with stage I and II cancers. We also excluded advanced laryngeal, hypo pharyngeal or thyroid cancers with extensive obstruction of the larynx (Comark-Lahane Grade 4), unidentifiable upper Aerodigestive anatomy, ulcerated or friable lesions and patients with stridor.
Results
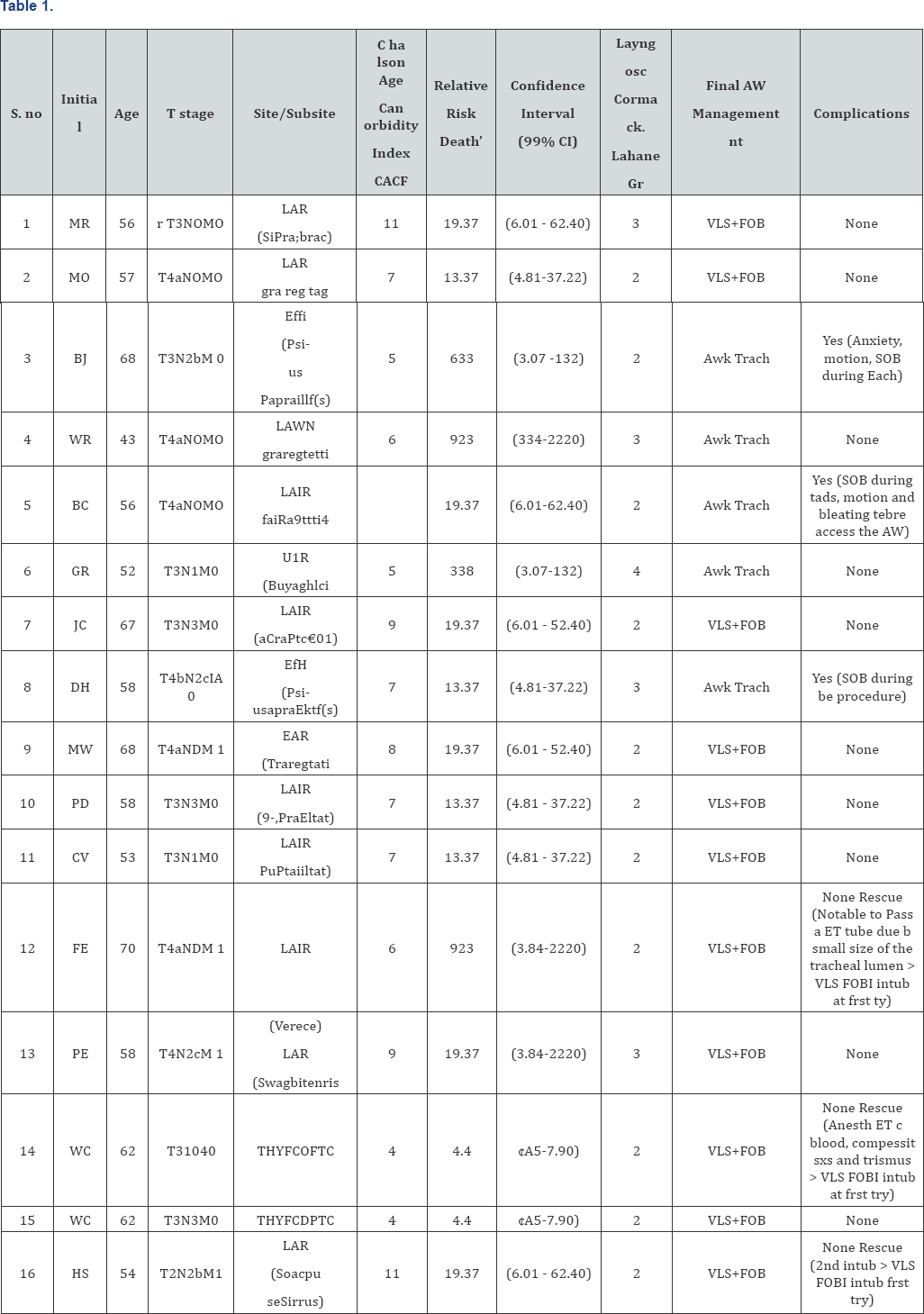
From 16 patients evaluated, there were 7 stage III (44%) and 9 stage IV (56%) patients as seen in Table 1. Out of 16 patients considered for VLS/FOBI, eight (50%) patients were not initially attempted with this method due to the anesthesiologist preference, 5 (31%) were requested securing of the airway by awake surgical tracheotomy. Of these, three (19%) were stable airways but the anesthesiologist was unfamiliar with the method. Two patients were unstable and had developed stridor in the morning prior to the procedure due fast progression of the tumor since last laryngoscopy. Three (19%) were tried intubation by VLS alone by anesthesiologist, after a failed intubation trial all three were successfully rescued by VLS/FOBI. Eleven patients (69%) intubated by VLS/FOBI procedures resulted in successful intubations at first pass without any complication such as trauma to adjacent tissues, bleeding, oxygen desaturation, or loss of supraglottis view that could delay the intubation process. None of the intubations via this method took longer than 2 minutes.
Discussion
The ultimate fear of an anticipated difficult intubation is "failure to intubate," and the principal factor contributing to failed tracheal intubation is the inability to view the vocal cords [7]. This situation is not uncommon in advanced oral cavity, pharynx, larynx, thyroid gland, neck metastatic cancer, post irradiated neck, laryngeal deviation or previous surgery where the normal landmarks are distorted or absent due to tumor progression. Elective fiberoptic intubation is a technique considered standard by American Society of Anesthesiologists task force on management of the difficult airway when a challenging airway is anticipated, such as in the aforementioned cases [11]. However, FOBI is limited by three important factors. First, the technique is mostly dependent on FOBI user experience and confidence, and therefore, outcome is operator skill dependent. Secondly, the position of the patient and the level of sedation contribute to the base of the tongue, epiglottis, and pharyngeal soft tissue falling to the back of the pharynx obstructing the airway [12,13].
Lastly, it is not infrequent for the operator to struggle to recognize laryngeal landmarks resulting from the limited narrow view from the flexible bronchoscope and potential secretions or blood obscuring the optics. The described technique is particularly useful when the narrow view limitation can be compensated by using the panoramic view from the VLS in which the 60o blade lifts the base of the tongue and pharyngeal soft tissue, yielding a much broader frontal view of the epiglottis, arytenoids, and aryepiglottic folds. The ultimate result is the additional visualization from the FOB assisted by VLS over the area of interest while having the operator to freely manipulate and advance the tip of the fiberscope. A suction and irrigation channel is also available for usage during the intubation. In a large randomized clinical trial the median time for Videolaryngoscopy intubation was 3 minutes [14]. Overall, in our series none of the cases required a second pass or took longer than 2 minutes. However, three cases we changed to a longer VLS blade and three cases we removed the blade to clear excessive secretions over the optics.
However, these changes did not add increased overall time to intubation. It is known that awake tracheotomy in cancer extending to the larynx is not exempt from complications and can pose a sudden major risk to the airway due to many factors. Typically, these patients are smokers with COPD, compromised pulmonary function and low respiratory reserve. When performing an expeditious surgical airway procedure there are unique risks such as unexpected coughing, anxiety, panic, motion or inability to maintain a supine position, inability to maintain neck a still under extension, possibility of distorted anatomy or associated uncontrolled comorbidities. These unique risks associated to comorbidities can result in oxygen desaturation, bleeding, pneumothorax, sudden loss of ventilation, seeding tumor in the peristomal access, and death. We included in Table 1 Charlson Age Comorbity Index "CACI” and respective relative risk of death.
These complications are not always mentioned in the literature [9,15,16]. For these reasons, one should keep in mind high morbidity and mortality due to the potential existing risks when performing awake tracheostomy on these patients. If the anatomy is favorable the ideal is to perform tracheotomy in patients under controlled conditions who are previously intubated and whose airway is already secure. There were any randomized controlled trials comparing the frequency of seeding tumor due to endotracheal intubation on larynx cancer patients in the literature. However; Esteller et al discussed stomal recurrence and tumor seeding of the tracheostomy site [17]. Apparently, this risk can be potentiated by expedited or emergent awake tracheostomies.
Conclusion
Even with a thorough clinical pre-anesthetic assessment, complications cannot be predicted in this subset of patients. Tracheotomy is ideally performed in a previously intubated patient whose airway is secure when compared to awake tracheotomy under local anesthesia. Sudden changes like impending airway obstruction in a stable patient may require an expedited surgical procedure, increasing risks for complications. Videolaryngoscopy combined fiberoptic bronchoscopic assisted endotracheal tube placement is easily performed and efficient, providing an excellent view of the airway anatomy. VLS/ FOBI is a useful method for professionals involved in airway management in hospital setting. The equipment is readily available in a majority of hospitals. Although this technique requires an assisting hand, it is considered easier to perform than fiberoptic intubation alone, requires the same amount of time for intubation, and potentially saves the patient from emergent or urgent airway procedures which carry increased risk of complications.
References
- Brown CA, Bair AE, Pallin DJ, Lauren EG, Wall RM (2010) National Emergency Airway Registry (NEAR) Investigators. Improved glottic exposure with the Video Macintosh Laryngoscope in adult emergency department tracheal intubations. Ann Emerg Med 56(2): 83-88.
- Griesdale DE, Liu D, McKinney J, Choi PT (2012) Glidescope® videolaryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anesth 59(1): 41-52.
- Mosier JM, Stolz U, Chiu S, Sakles JC (2012) Difficult Airway Management in the Emergency Department: Glidescope Videolaryngoscopy Compared to Direct Laryngoscopy. J Emerg Med 42(6): 629-634.
- Yarmus L, Gilbert C, Akulian J, Feller Kopman D (2012) Novel use of GlideScope for rigid bronchoscopic placement of Dynamic (Y) stent. Ann Thorac Surg 94(1): 308-310.
- Yents SM (2002) Predicting difficult intubation-worthwhile exercise or pointless ritual? Anaesthesia 57(2): 105-109.
- Shiga T, Wajima Z, Inoue T, Sakamot A (2005) Predicting Difficult Intubation in Apparently Normal Patients: A Meta-analysis of Bedside Screening Test Performance. Anesthesiology 103(2): 429-437.
- Cormack RS, Lehane J (1984) difficult tracheal intubation in obstetrics. Anaesthesia 39(11): 1105-1111.
- Doyle DJ (2004) GlideScope-assisted Fiberoptic Intubation: A New Airway Teaching Method. Anesthesiology 101(5): 1252.
- Altman KW, Waltonen JD, Kern RC (2005) Urgent Surgical Airway Intervention: A 3 Year County Hospital Experience. Laryngoscope 115(12): 2101-2104.
- Vitin AA, Erdman JE (2007) A difficult airway case with GlideScope- assisted fiberoptic intubation. Journal of Clinical Anesthesia 19(7): 564-565.
- Caplan RA, Benumof JL, Berry FA, Blitt CD, Bode RH, et al. (2013) Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 98(5): 1269-1277.
- Xue FS, Li CW, Zhang GH, Li XY, Sun HT, et al. (2006) GlideScope®- assisted awake fiberoptic intubation: initial experience in 13 patients. Anaesthesia 61(10): 1014-1015.
- Crosby ET, Cooper RM, Douglas MJ, Doyle DJ, Hung OR, et al. (1998) the unanticipated difficult airway with recommendations for management. Can J Anaesth 45(8): 757-776.
- Lascarrou JB, Boisrame Helms J, Bailly A, Le Thuaut A, Kamel T, et al. (2017) for the Clinical Research in Intensive Care and Sepsis (CRICS) Group. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation among ICU Patients. A Randomized Clinical Trial. JAMA 317(5): 483-493.
- Moore MS, Wong AB (2007) GlideScope intubation assisted by fiberscope. Anesthesiology 106(4): 885-886.
- Yuen HW, Loy AH, Johari S (2007) Urgent awake tracheotomy for impeding airway obstruction. Otolaryngology Head and Neck Surg 136(5): 838-842.
- Esteller E, Aguero A, Martel M, Lopez M, Quer M, et al. (2014) Stomal recurrence in head and neck cancer patients with temporary tracheostomy. Auris Nasus Larynx 41(5): 467-470.





























