Unilateral Laryngeal and Lingual Paralysis (Tapia Syndrome) After Cardiac Surgery for Aortic Aneurysm: A Case Report and Proposal for a Rehabilitation Protocol
Matteo Cavaliere2*, Rossella Cuofano1, Maria Spagnuolo1, Giuseppe Panetti2, Maria Panetti2 and Maurizio Iemma1
1Department of Otorhinolaryngology, University Hospital “San Giovanni di Dio e Ruggi d'Aragona', Salerno, Italy ’
2Department of Otorhinolaryngology, “Ascalesi Hospital“, Naples, Italy
Submission: March 23, 2018; Published: April 03, 2018
*Corresponding author: Cavaliere Matteo, Via Madonna di Fatima 53 - 84084 Fisciano (Salerno), Italy, Tel: (39) 3479043472; Email: matorl@inwind.it
How to cite this article: Matteo C, Rossella C, Maria S, G, Maria P, Maurizio I . After Cardiac Surgery for Aortic Aneurysm: A Case Report and Proposal for a Rehabilitation Protocol. Glob J Otolaryngol 2018; 14(2): 555884. DOI: 10.19080/GJO.2018.14.555884
Abstract
Tapia syndrome is a rare complication after cardiac surgery, with only 4 other cases described in the literature. It is characterized by ipsilateral paralysis of the vocal cord and tongue due to an extracranial involvement of the recurrent laryngeal and hypoglossal nerves. We describe this clinical case occurred at our Hospital and the protocol of logopedic rehabilitation adopted. The patient (31 years, male) developed the Tapia syndrome after surgery for aneurysm of the ascending aorta. In the post-operative period he developed severe dyspnea and dysphagia that required a tracheostomy and a logopedic rehabilitation therapy that led to a fast and efficient swallowing without aspiration after 47 sessions (less than 4 months).The progressive recovery of the function suggests aprassic nerve damage. However, the logopedic therapy is recommended to limit the possibility of permanent functional deficits and quickly recover swallowing and phonation.
Keywords: Tapia syndrome; Laryngeal paralysis; Tongue paralysis.
Introduction
Tapia syndrome, first described in 1904 by A. Garcia Tapia, is a rare complication after cardiac surgery, withipsilateral paralysis of vocal cord and tongue by extracranial involvement of recurrent laryngeal and hypoglossal nerves. It is usually related to anesthesia and position of patient's head during surgery [1,2] with only 4 cases described in literature [3-6]. We present this rare complication occurred at our Hospital and the rehabilitation protocol adopted.
Case Report
Medical history
30 October 2014: a male patient of 31 years underwent cardiac surgery for correction of ascending aortic aneurysm and pulmonary valve insufficiency according to Tirone David technique [1].
4 November 2014: already extubated from 2 days, he underwent tracheostomy for dyspnea and was fed with total parenteral nutrition for dysphagia for both solids and liquids.
Diagnostic study
ENT evaluation:
a. Deficit of lingual strength and lateral deviation of tongue to the right, as for a deficit of the right XII cranial nerve;
b. Right hemi-laryngeal paralysis and left hemi- laryngeal paresis in an intermediate position (the latter already present before surgery);
c. Profuse stagnation of mucus and saliva in pyriform sinuses, as for upper esophageal sphincter opening deficit;
d. After semisolid bolus, increased secretions in hypopharynx and valleculae, as forlingual thrust deficit, with partial aspiration followed by strong cough;
e. After semi-liquid bolus, increased secretions in hypopharynx, as for pharyngo-esophageal propulsion deficit, with partial aspiration followed by strong cough.
Pharyngo-esophageal videofluoroscopy [1]:
a. Reduced movement of lingual retropulsion: bolus was swallowed only after repeated attempts with compensation movements;
b. Epiglottis immobility;
c. Low contraction of upper and middle pharyngeal constrictor muscles: bolus was stagnant in valleculae and pyriform sinuses, that emptied incompletely and after repeated attempts;
d. A portion of contrast medium passed into the airways in post-swallowing phase.
Logopedic treatment
4 December 2014: definition and beginning of an individualized logopedic rehabilitation program to:
a. Improve speed and efficiency of swallowing.
b. Remove suction through compensatory strategies (facilitating postures, voluntary defensive maneuvers of the airways, dietary tricks and correction of salivary deficits) and strategies to recover mobility and strength of each structure of oro-pharyngeal-laryngeal district.
c. Treatment of dysphagia followed two different paths, compensation and rehabilitation, to ensure the patient to safely feed. The work plan acted on:
i. General area: on being vigilant, as our patient was, and activation of metacognition, to identify, discriminate and recognize swallowing movements, at every stage.
ii. Sectorial area: on general relaxation, body awareness and breathing control.
iii. Specific area: therapeutic measures on the structures involved in swallowing and bound to:
a. Compensation of patient disability by facilitative posture (head bent forward, head turned to the right) and dietary tricks (consistency, cohesion degree, homogeneity, bolus volume and temperature).
b. Recovery of tone, strength and mobility of lips, tongue and laryngeal structures by [1,2]:
c. Masako maneuver: production of «ka» sound by holding the tip of tongue between the incisors, boosting posterior pharyngeal wall.
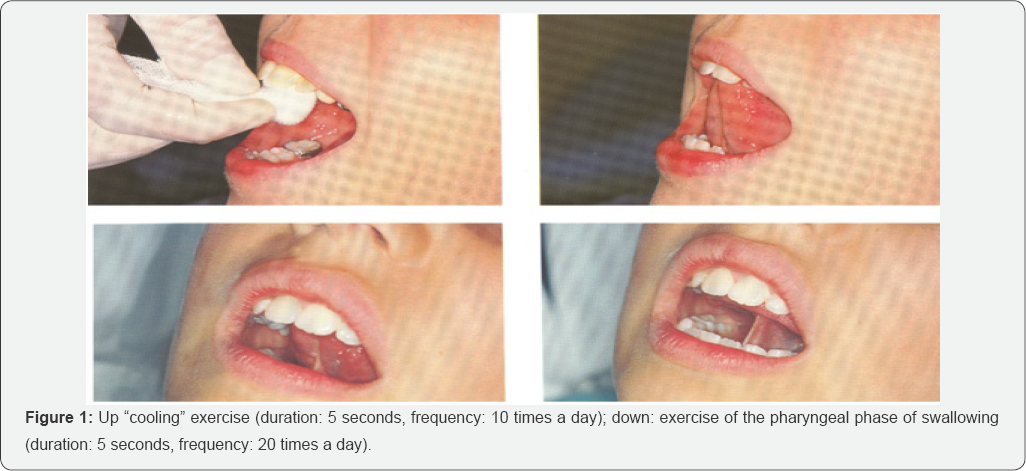
Proprioception exercises, achieving neuromuscular response through stimulation of proprioceptors, free nerve endings and receptors that govern tactile and thermal sensitivity of tongue (Figure 1)
a. "Cooling” exercise: an ice cube wrapped in gauze at level of the retro-incisive papilla on the two sides of the tongue, evoking tongue elevation towards the stimulated area;
b. Exercise to retraces pharyngeal phase of swallowing: patient is asked to open his mouth, to bring the tip of his tongue in contact with the papilla, to raise the whole tongue towards palate and to «flatten it» against this, for 5 seconds, and then to remove the dorsum of tongue from the palate, whilst maintaining the tip in contact with it Figure 2.
Muscular gymnastic and functional recovery exercises
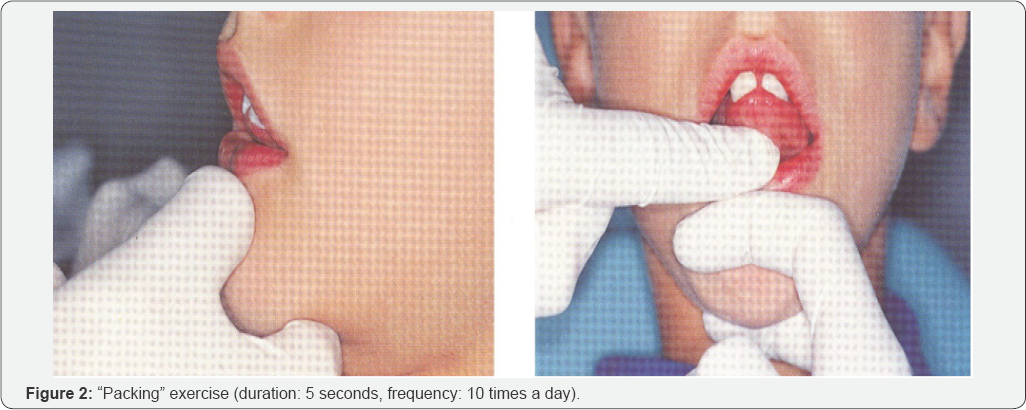
a. "Packing” exercise for muscles of the mouth floor (Figure 3): the tip of tongue rests on the palate, in contact with palatine wrinkles. Patient has to slightly open his mouth and press the tip of tongue very strong against the palate, maintaining the same position. During the exercise, the rehabilitator pushes with his index finger under muscles of oral floor, both to verify the effective contraction, and to exert a resistance opposing the downward movement of mouth floor.
b. "Tongue depressor” exercise for the tip of tongue (Figure 4): patient is asked to push his tongue tip horizontally against a tongue depressor placed over his mouth.
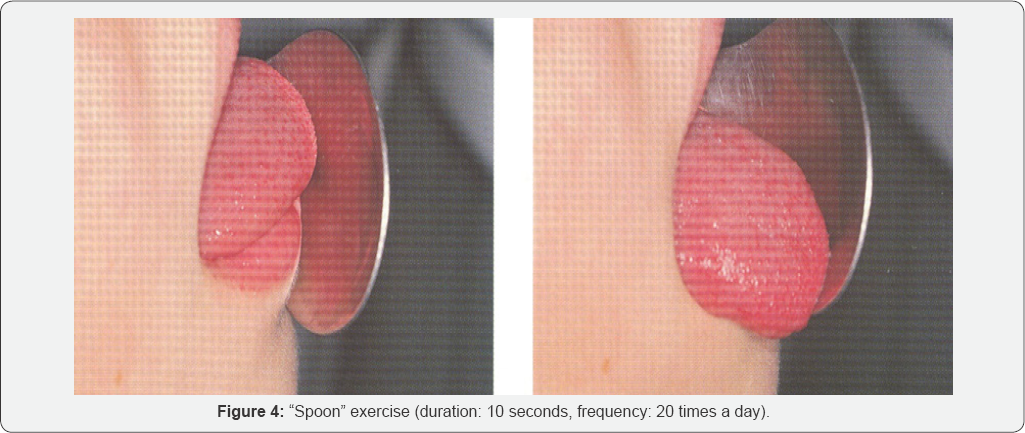
c. "Spoon” exercise for the tip of tongue (Figure 5): push and simultaneously move the tip of tongue against the concave surface of a spoon, circumferentially from right to left.
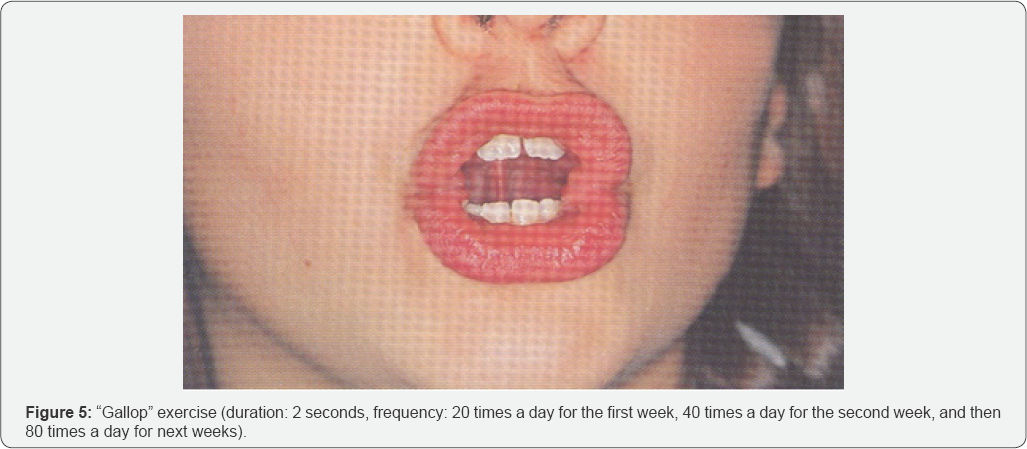
d. "Gallop” exercise for the body tongue: the tongue, initially positioned with the tip in contact with palate, detaches from it, in a sweeping motion toward the mouth floor, imitating noise of a galloping horse. With the production of sounds A and O, the exercise also alternatively acts on labial commissures, thus enhancing buccinator muscles.
e. "Yawning” exercisefor tongue retrusion and for posterior portion of the tongue: patient has to yawn and feel the position that the tongue assumes; then, repeating the movement without yawning, the tongue must flatten and move back.
f. Exercises of circling of lingual apex and displacing appropriate pseudo-boluses within oral cavity; in particular, we used whole olives asking to eat the fruit and eject the core.

Exercises of phono-articular rehabilitation
a. Slow and hyper-articulate repetition of letters produced by bringing the tip of tongue on incisive papilla, ie L-T-N-D, with vowel emissions before and after these letters; rapidly and loudly repetition of 5 identical syllables: LALALALALA, NANANANANA, DADADADADA, TATATATATA, RARARARARA.
b. Addition of a wheezing prolonged S and repetition of words with these groups fast changing articulatory position, even for other groups like LT-LD-ND.
c. Say for as long as possible the letter R, by vibrating the tip of tongue against the anterior portion of palate.
d. Use letters produced with the middle part of tongue against the palate, ie C and G, and by lifting the back of tongue and velo-pharyngeal structures, ie K and G.3
Treatment sessions were 47 in 4 months
a) 19th session: Patient began to drink semi-liquids with a glass.
b) 23rd session: Tracheostomy tube was removed and he began to eat semi-solids.
c) From 26th session, solids (pasta, beef tenderloin, stewed chicken breast and Pandoro).
d) From the 33rd session, pizza margherita and cake with berries.
e) From the 37th session, mozzarella and sliced, potato omelette, vegetable omelette and biscuits with ice cream.
f) 47th session: He showed mild difficulties only for liquids, increased tone of voice with reduced hoarseness.
Discussion And Conclusion
Tapia syndrome is a rare complication after cardiac surgery with ipsilateral paralysis of the vocal cord and tongue, and a normal function of the soft palate. It is usually related to anesthesia and to the position of the patient's head during surgery, resulting in stretching of the vagus and hypoglossal nerves [7-12].
The pathogenetic hypothesis is a pressure-related neuropathy due
a. For paralysis of tongue, to the trauma of XII cranial nerve during intubation, due to both the pressure applied on the lateral border of tongue using the Macintosh blade, and to hyperextension of head and neck [1,2]. In the latter case it is possible that nerve is compressed on the lateral protrusion of the anterior face of the transverse process of C1.
b. For vocal fold paralysis, to the compression of anterior branch of recurrent laryngeal nerve between the cuff of a dislocated endotracheal tube and posterior portion of the thyroid shield
References
- Drouet A, Straboni JP, Gunepin FX (1999) Paralysis of the hypoglossal nerve after orotracheal intubation for general anesthesia. Ann Fr Anesth Reanim (18): 811-812.
- Eduardo Rubio-Nazabal, Jose Marey-Lopez, Soledad Lopez, Alvarez- Perez, Antonio Martinez-Figueroa, et al. (2002) Isolated bilateral paralysis of the hypoglossal nerve after transoral intubation for general anesthesia. Anesthesiology (96): 245-247.
- Kenneth C, Arbelaez C, Yodice P (2002) Bilateral vocal cord dysfunction complicating short term intubation and the utility of heliox. Respiration 69(4): 366-368.
- Nalladaru Z, Wessels A, DuPreez L (2012) Tapia's syndrome-a rare complication following cardiac surgery. Interact Cardiovasc Thorac Surg 14(1): 131-132.
- Rotondo F, De Paulis S, Modoni A (2010) Peripheral Tapia's syndrome after cardiac surgery. Eur J Anaesthesiol 27(6): 575-576.
- Sotiriou K, Balanika M, Anagnostopoulou S, Gomatos C, Karakitsos D, et al. (2007) Postoperative airway obstruction due to Tapia's syndrome after coronary bypass grafting surgery. Eur J Anaesthesiol 24(4): 378379.
- Gelmers HJ (1983) Tapia's syndrome after thoracotomy. Arch Otolaryngol 109(9): 622-623.
- Tesei, Poveda LM, Strali W, Tosi L, Magnani G, et al. (2006) Unilateral laryngeal and hypoglossal paralysis (Tapia's syndrome) following rhinoplasty in general anaesthesia: case report and review of the literature. Acta Otorhinolaryngol Ital 26(4): 219-221.
- David TE (2014) Aortic valve-sparing operations. Semin Thorac Cardiovasc Surg 23(2): 231-238.
- Siebens A, Linden P (1985) Dynamic imaging for swallowing pathophisiology reeducation. Gastrointestinal Radiology 10(1): 251253.
- Schindler O, RuoppoloG, Schindler A (2011)Deglutologia. Omega Ed.
- Cozza P, Polimeri P, De Toffol P (2002) Manuale di terapia miofunzionale. Elsevier. Figure 4: "Spoon” exercise (duration: 10 seconds, frequency: 20 times a day).





























