Ultimate Leprosery in Europe
Cristina Otilia Laza* and Mariana Codreanu
Department of ENT, County Clinical Emergency Hospital of Constanta, Romania
Submission: February 19, 2018; Published: April 03, 2018
*Corresponding author: Cristina Otilia Laza, Department of ENT, County Clinical Emergency Hospital of Constanta, Romania, Email: cristinaotilia@gmail.com
How to cite this article: Cristina O L, Mariana C. Ultimate Leprosery in Europe. Glob J Oto 2018; 14(2): 555881.. DOI: 10.19080/GJO.2018.13.555881.
Abstract
Leprosy is a contagious and chronic systemic granulomatous disease caused by Mycobacterium leprae (Hansen's bacillus). It is transmitted from person to person and has a long incubation period (between two and six years). The disease presents polar clinical forms (the multibacillary lepromatous leprosy and the paucibacillary tuberculoid leprosy), as well as other intermediate forms with hybrid characteristics. The diagnosis, based on clinical suspicion, is confirmed through bacteriological and histopathological analyses, as well as by means of the lepromin test (intradermal reaction that is usually negative in lepromatous leprosy form and positive in the tuberculoid form). Treatment is difficult as it must be continued for long periods, requires several drugs with adverse effects, most commonly used drugs are dapsone, rifampicin and clofazimine. In Romania where leprosy was declared eradicated since 1950 is still in function the single and last hospital for patients with leprosy but the last patient was admitted in, 1980 and now all are cured but immobilized by their mutilation lesions. Now a nice place for retirement in 1900 was a hospital-prison where the unfortunate patients with leprosy were under treatment isolated from the entire world, There are only 23 patients now ,all very old expecting to died ,cured but depending on the hospital because of their severe mutilations sequel .But is this all ,leprosy in Europe is eradicated complete?
Keywords: Mycobacterium leprae; Skin involvment; Anesthesia nerv paresis; Mutilation
Introduction
a) Leprosy, also called Hansen's disease, is a chronic infectious disease that primarily affects the skin, the peripheral nerves, the mucosa of the upper respiratory tract, and the eyes. Leprosy can lead to progressive permanent damage of these structures, and the resulting devastating disfigurement and disability has led to the historical social stigma and isolation (leper colonies) of those affected by the disease.
b) Historically speaking, leprosy has existed since at least 4000BC, and the disease was present and described in the ancient civilizations of China, India, and Egypt. The first known written reference to the disease on Egyptian papyrus dates from about 1550 BC. It is believed that leprosy was brought to Europe by the Romans and the Crusaders and that later the Europeans brought it to the Americas. For centuries, leprosy remained a poorly understood disease characterized by human suffering and social isolation.
c) Leprosy can be considered 2 connected diseases that primarily affect superficial tissues, especially the skin and peripheral nerves. Initially, a mycobacterial infection causes a wide array of cellular immune responses. These immunologic events then elicit the second part of the disease, a peripheral neuropathy with potentially long-term consequences. The social and psychological effects of leprosy, as well as its highly visible debilities and sequelae have resulted in a historical stigma associated with leprosy.
d) Leprosy is a curable disease with the use of multidrug therapy (MDT). In 1991, the World Health Assembly passed a resolution to eliminate leprosy as a public-health problem by the year 2000.
e) Leprosy has been eliminated from 119 countries out of the 122 countries where previously leprosy had previously been deemed a public-health concern in 1985.
f) Countries in which leprosy is more commonly found include Angola, Bangladesh, Brazil, China, Central African Republic, Ethiopia, India, Indonesia, Madagascar, Myanmar, Nepal, Nigeria, Philippines, Sudan, South Sudan, Sri Lanka, United Republic of Tanzania, Democratic Republic of the Congo, and Mozambique.
g) On average, 150-250 new cases of leprosy are diagnosed each year in the United States, with most cases occurring in immigrants. 65% of these cases occurring in California, Florida, Hawaii, Louisiana, New York, Texas, and Massachusetts.
h) However, because the bacteria can be found in wild animals (for example, armadillos and chimpanzees), it is unlikely that leprosy will be totally eliminated like smallpox. The mode of transmission of leprosy is still unclear but is thought to be through a respiratory route. Cutaneous transmission appears to require prolonged contact to open lepromatous wounds. Leprosy is caused by Mycobacterium leprae, an add-fast bacillus, which is an obligate intracellular parasite. bacteria are thermo labile, growing optimally between 27 oC and 33 oC, and divide slowly; thus the disease evolves slowly and involves primarily cooler peripheral tissues such as in the fingers, nose, testicles, feet, and earlobes.
i) Although M. Leprae cannot yet be cultured on an artificial medium, it can nevertheless be inoculated into experimental animals, particularly immunologically deficient mice, to produce a disease similar to that in man. Based on the host's immunological status and clinical, histological and microbiological features leprosy divided into types [1-3].
Pathophysiology


Leprosy can manifest in different forms, depending on the host response to the organism. Individuals who have a vigorous cellular immune response to M leprae have the tuberculoid form of the disease that usually involves the skin and peripheral nerves. The number of skin lesions is limited, and they tend to be dry and hypoesthetic. Nerve involvement is usually asymmetric. This form of the disease is also referred to as paucibacillary leprosy because of the low number of bacteria in the skin lesions (ie, < 5 skin lesions, with absence of organisms on smear). Results of skin tests with antigen from killed organisms are positive in these individuals Figure 1 & 2.
Individuals with minimal cellular immune response have the lepromatous form of the disease, which is characterized by extensive skin involvement. Skin lesions are often described as infiltrated nodules and plaques, and nerve involvement tends to be symmetric in distribution. The organism grows best at 27-30 °C; therefore, skin lesions tend to develop in the cooler areas of the body, with sparing of the groin, axilla, and scalp. This form of the disease is also referred to as multibacillary leprosy because of the large number of bacteria found in the lesions (ie, >6 lesions, with possible visualization of bacilli on smear). Results of skin tests with antigen from killed organisms are nonreactive [4-6].
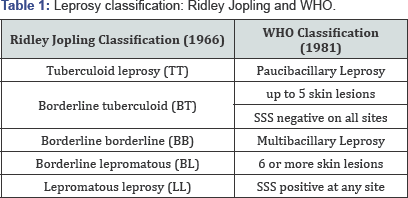
Patients may also present with features of both categories; however, over time, they usually evolve to one or the other (indeterminate or borderline leprosy). Interestingly, most individuals who are exposed to leprosy never develop the disease Table 1.
Classification of leprosy
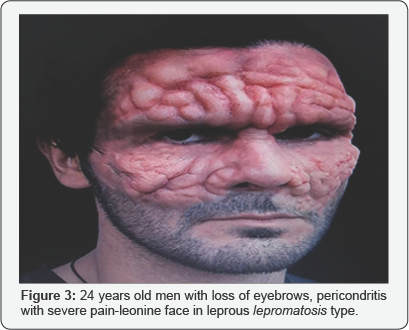
Leprosy has 2 classification schemas: the 5-category Ridley- Jopling system and the simpler and more commonly used WHO standard. In 1966, Ridley and Jopling proposed a classification system for leprosy for research purposes and is still used in clinical practice in U.S. and most European countries. The Ridley-Jopling system classifies leprosy as an immune-mediated spectral disease with tuberculoid leprosy (TT) at one end of the spectrum and lepromatous leprosy (LL) at the other end. These two ends of the spectrum are considered to be clinically stable. Immunologically, strong cell-mediated immunity correlates with the TT type and weak CMI correlates with the LL type of the disease. Between these two ends lies the clinically unstable borderline spectrum, which can be further subdivided into borderline tuberculoid (BT), mid-borderline (BB), and borderline lepromatous (BL), of which BB is the least stable. Leprosy as a disease frequently undergoes changes in clinical presentation depending on the immune status of the individual. I Hence, the Ridley-Jopling classification helps correlate the disease pathophysiology with the clinical features and describes leprosy as a spectral disease from a clinical, immunological, and histopathological perspective, but does not include the indeterminate and pure neuritic forms of leprosy Figures 3 & 4.

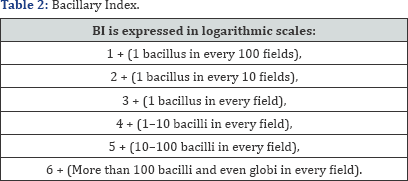
The WHO classification system (1981), which is an operational classification system, was developed to simplify chemotherapy as multibacillary (MB) or paucibacillary (PB) leprosy. This distinction was initiall made on the basis of SSS positivity, in which patients with a bacillary index, but more than 2 are treated as MB and the rest as PB. The BI is directly related to the bacterial load, and it denotes the total number of bacilli, regardless of their shape and staining. The current WHO classification of leprosy as MB or PB is simply based on the total number of leprosy lesions in a given individual. Initially, for feasibility and operational purposes, all of the patients who had SSS positivity were regarded as MB. However, when SSS was applied globally, quality control issues emerged. Hence, in 1998, SSS was omitted as a basis for the distinction between MB and PB leprosy [7-10].
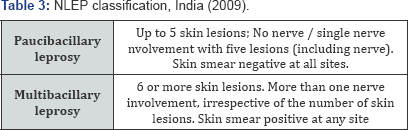
In India, the number of nerves involved, along with the number of skin lesions, is taken into consideration in the classification of leprosy into PB and MB cases. Single nerve involvement is labeled PB; more nerve involvement is labeled. INDIAN CLASSIFICATION was accepted and adopted in India in 1955 .The aim of the Indian system was to include all levels of leprosy workers from grass-root workers to researchers. The Indian classification includes six groups:
a) Tuberculoid,
b) Borderline,
c) Lepromatous,
d) Indeterminate,
e) Pure neuritic, and
f) Maculoanesthetic
In 1981, the Indian classification was modified and accepted by the Indian Association of Leprologists (IAL) and the new five- group classification was named the New IAL classification of leprosy Maculoanesthetic leprosy was later removed from this classification.
Mortality/Morbidity
Leprosy is rarely fatal, and the primary consequence of infection is nerve impairment and debilitating sequelae. According to one study, 33-56% of newly diagnosed patients already displayed signs of impaired nerve function. According to estimates, 3 million people who have completed multidrug therapy for leprosy have sustained disability due to nerve damage. Although both lepromatous leprosy and tuberculoid leprosy involve the skin and peripheral nerves, tuberculoid leprosy has more severe manifestations. Nerve involvement results in loss of sensory and motor function, which may lead to frequent trauma and amputation. The ulnar nerve is most commonly involved.
Damage in the following nerves is associated with characteristic impairments in leprosy:
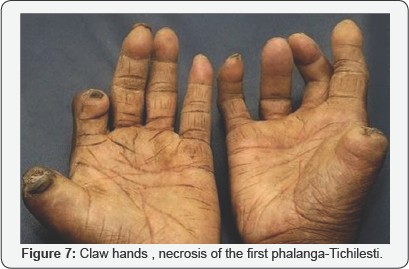
a. Ulnar and median - Clawed hand
b. Posterior tibial - Plantar insensitivity and clawed toes
c. Common peroneal - Foot drop
d. Radial cutaneous, facial, and greater auricular nerves (may also be involved; as seen in the image below)
Infiltration by bacteria may lead to destruction of nasal cartilage (lepromatous leprosy), ocular involvement, and diffuse thickening of the skin. Advanced cases of leprosy involve the loss of eyebrows and lashes, but these deformities are less common today Table 2.
Worldwide, leprosy is considered the most common cause of crippling of the hand, which is caused by ulnar nerve involvement. Peroneal nerve involvement can lead to foot drop, posterior tibial nerve involvement, and clawed toes. Symptoms are as follows:
a) Painless skin patch accompanied by loss of sensation but not itchiness (tuberculoid leprosy, unlike lepromatous leprosy, in which sensation is preserved.)
b) Loss of sensation or paresthesias
c) Wasting and muscle weakness
d) Foot drop or clawed hands (from neuritic pain and nerve damage
e) Ulcerations on hands or feet (ulcer at the metatarsal head
f) Lagophthalmos, iridocyclitis, corneal ulceration, and/ or secondary cataract due to nerve damage and direct bacillary skin or eye invasion
g) Type 1 (reversal) - Sudden onset of skin redness and new lesions
h) Type 2 (erythema nodosum leprosum- Many skin nodules, fever, redness of eyes, muscle pain, and joint pain
Diagnosis
Physical examination should include the following:
a) Evaluation of skin lesions
b) Careful sensory and motor examination
c) Palpation of peripheral nerves for pain or enlargement, with particular attention paid to the following locations:
I. Elbows - Ulnar nerve
II. Wrist - Superficial radial cutaneous and median nerves
o Popliteal fossa - Common peroneal nerve
III. Neck - Great auricular nerve Physical findings in specific leprosy subtypes
Tuberculoid leprosy (TT) or paucibacillary leprosy (PB): Vigorous host resistance and low infection - localized disease a-single, clear demarcated hypo pigmented/anesthetic skin area of the face, hand or feet, with thickening of the sub serving sensory or motor nerves. This could on to paralysis of muscles. Skin lesions may extend up to the nasal vestibule. This type of lesion falls short without involving the nasal mucosa. Isolated cranial nerve palsies (V and VIIth).
Borderline Tuberculoid Leprosy (BT): As TT, but more numerous, smaller skin lesions with thickening of peripheral nerves and deformity of the hands and feet Borderline Leprosy (BB). Numerous skin lesions of varying size and form (macules, papules, plaques) with punched-out, hypopigmented anaesthetic centres; widespread nerve.
Lepromatous leprosy (LL) or Multibacillary Leprosy (MB): Severely compromised host resistance and massive infection with diffuse infiltration of skin, nerves and mucosal surfaces by the bacteria. Cutaneous infiltration is more common over the edges of pinna, chin, nose and yebrows these areas have a temperature lesser than that of core temperature. These patients are considered to be highly infectious, as their nasal discharges contain potentially infectious lepra bacilli. Nose involvement
a. Crust formation
b. Nasal obstruction
c. Sero sanguineous discharge
d. Nodular yellowish thickening of nasal mucosa
e. T -anterior end of inferior turbinate
f. Nasal bridge collapse is commonly seen in these patients because bony and cartilaginous portions of nasal septum are destroyed due to perichondritis and periosteitis. Collapse of the nose is considered pathognomic.
g. Perforation of palate is possible in nasosinusal infection
h. Anterior nasal spine is commonly destroyed in this patient. Hyposmia is seen in 40% cases of lepromatous leprosy. -Also-trigeminal anaesthesia suborbital [11-15].
Oral lesions-19-60%
Air cooled sites are more frequent: hard palate, soft palate, labial maxillary gingiva, tongue, lips, buccal maxillary gingiva, labial mandible gingiva & buccal mucosa. Complete loss of uvula & fixation of the soft palate may occur Lingual lesions primarily occur in the anterior third as areas of erosion. Infection of the lip results in MACROCHELIA.
Affected soft tissue appears as yellowish to red, sessile, firm, enlarging papules that develop ulceration and necrosis followed by attempted healing by secondary intention. Maxilary involvement causes: Enamel hypoplasia of the developing teeth & tapering roots. Dental pulpal involvement: pulpal necrosis, obvious red discoloration of the crown Hair, including the eye brows and lashes often are lost. Nerve involvement. Decreased touch sensitivity to touch, pain, temperature [16-18].
Other signs
a) Gynaecomastia
b) Testicular Atrophy
c) Ichthyosis
d) Nerve Palsies
e) Neurotrophic Resorption of the Phalanges
f) Lucio’s phenomenon (endarteritis and ulceration) is noted in Mexico Active disease progresses through stages o invasion proliferation, ulceration and resolution with fibrosis Incubation period-2-5 years for tuberculoid type 8-12 years for lepromatous variant.
Laboratory studies
a) CBC count
b) Creatinine level
c) Liver function tests
d) Nasal smear, direct, cultures
e) Skin biopsy- stained with hematoxylineosin and Fite Faraco anathomopatology Immunologic tests include the following.
f) Polymerase chain reaction (PCR): PCR and recombinant DNA technology used to identify the mycobacterium in biopsy samples, skin and nasal smears, and blood and tissue sections.
g) Phenolic glycolipid-1: detection of antibodies to phenolic glycolipid sensitivity of 95% for lepromatous leprosy but only 30% for tuberculoid leprosy
h) Lymphocyte migration inhibition test (LMIT): for cell- mediated immunity Lepromin skin test -assesses a patient's ability to amount a granulomatous response against a skin injection of killed M leprae. Patients with tuberculoid leprosy or borderline lepromatous leprosy typically have a positive response (>5mm). Patients with lepromatous leprosy typically have no response.
i) Contact or family screening for history of leprosy
j) A nerve biopsy can be beneficial in ruling out diseases such as hereditary neuropathies or polyarteritis nodosa. Nerve biopsies may also help identify abnormalities in patients with subclinical leprosy and may be the only way to definitively diagnose completely neuropathic forms of leprosy [19-21].
Histologic Findings
Findings vary but can include dermatitis, giant cells, infiltration of nerve bundles with mononuclear cells, and granulomas. Lepromatous lesions generally contain numerous acid-fast bacilli and fat-laden macrophages with a paucity of lymphocytes Table 3.
Treatment & Management
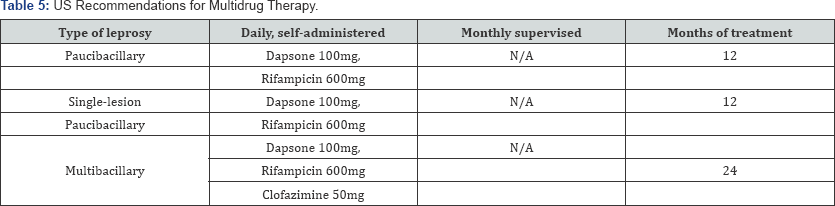
Medical Care: In response to the increased incidence of dapsone resistance, the WHO introduced a multidrug regimen in 1981 that includes rifampicin, dapsone, and clofazimine. Quinolones, such as ofloxacin and pefloxacin, as well as some macrolides, such as clarithromycin and minocyclin, are also effective However; the WHO still recommends the use of the long-term multidrug regimens whenever possible because they have been found to be more efficacious.
WHO Multidrug Therapy Regimens. Courtesy of WHO, Leprosy Elimination, http://www.who.int/lep/mdt/en/, accessed nov 14, 2017.
WHO Multidrug Therapy Regimens. Courtesy of WHO, Leprosy Elimination, http://www.who.int/lep/mdt/en/, accessed nov 14, 2017.
Corticosteroids have been used to treat nerve damage associated with leprosy, Prednisolone is believed to minimize pain and acute inflammation 40mg daily. Observations of increasing resistance in patients treated for leprosy have been reported in Southeast Asia, notably in Vietnam, the drug most commonly found to be resistant is dapsone, often in the context of prior exposure or treatment attempts with monotherapy.
Surgical Care: The goals of surgical treatment in patients with leprosy are to prevent further deterioration, to improve motor function, and, in some cases, to improve sensation. Preoperative requirements. First, patients must have completed the multidrug therapy and should have negative skin smear results. The patient should not use steroids a few months before surgery, and acute neuritis should not be evident. Stiffness of hands and feet should be minimized with preoperative therapy [22].
Neural surgery: Attempts to restore autonomic function and sensation are rarel. Draining of acute nerve abscesses and fascicular dissection can reduce the pressure on nerves and may improve sensation. In some cases, longitudinal epineurotomy may relieve some sensory loss. Considerable nerve function can be regained in the posterior tibial nerve with neurovascular decompression via release of the flexor retinaculum. Calcaneal bands can be slit to relieve distal compression of branches on the sole of the foot. Nerve grafts may be of some benefit in patients with localized lesions. Neural surgery may also be indicated in patients with unremitting nerve pain Table 4.
Reconstruction and Functional Restoration
Clawed hands are repaired with arthrodesis or with a tendon transfer to 1 of 4 insertion sites on the finger: interosseus tendons, proximal phalanx, dorsal extensor expansion, or flexor sheath annular pulleys. The palmaris longus, flexor digitorum superficialis, extensor carpi radialis longus, and extensor indices are tendons that can be used for transfer. Tendon transfers are also used to repair abduction and Opposition of the thumb, dorsiflexion of the foot, and flexion and extension of the metacarpophalangeal and proximal interphalangeal joints, respectively.
Contractures of the hand, such as the thumb web contracture, can be repaired with Z-plasty, and joint stability can be improved with tenodesis. The constrictions caused by repetitive injury and healing in patients with leprosy can be treated with several methods. removal of the carpal tunnel roof, ulnar nerve transposition anteriorly, and epicondylectomy. Procedures that limit hyperextension of the metacarpophalangeal joint or keep it in flexion are not indicated in the insensate hands of patients with leprosy, who suffer from continued weakness.
Amputation is a last resort and is reserved for cases of extremely diseased tissue. Eye procedures.
Loss of eyelid function may be treated with passing a strip from the temporalis muscle through the eyelid and connecting it to the inner canthus. Tarsorrhaphy may help narrow the opening of the eyelid, and canthoplasty reduces sagging of the eyelids.
Cosmetic surgery
a) Nasal reconstruction
b) Removal of excess skin
c) Replacement of eyebrows using transplants of scalp hair
d) Removal of breast tissue formation due to gynecomastia
Consultations
Orthopedic surgeon
Dermatologist
Neurologist
Psychiatrist, and physical therapist, based on the needs of the individual patient
Complications

Type 1 reaction
Reversal, is a delayed-type hypersensitivity reaction that arises when borderline leprosy shifts toward borderline lepromatous leprosy with treatment. The reaction is characterized by edema and erythema of existing skin lesions, formation of new skin lesions, neuritis, and additional sensory and motor loss and is treatment are nonsteroidal antiinflammatory drugs (NSAIDs) and high-dose steroids 40-60mg/ day Figure 5.
Type 2 reaction
Erythema nodosum leprosum (ENL), is a complication of lepromatous leprosy. It is characterized by the development of inflamed subcutaneous nodules accompanied at times by fever, lymphadenopathy, and arthralgias. High levels of tumor necrosis factor-alpha and immune complex deposition are associated with ENL. Treatment includes prednisolone, clofazimine, or thalidomide.
Lucio phenomenon
It is a severe complication of multibacillary leprosy that is marked by blue hemorrhagic plaques and necrotic ulcerations. The bacilli may extend to the endothelial cells along with the appearance of necrotic epidermis and vasculitis with thrombus formation and endothelial proliferation [23].
Follow-up
Monthly outpatient follow-up is recommended during treatment, although weekly visits may be necessary if the patient experiences a leprosy reaction Figure 6.

Follow-up laboratory studies during treatment include the following:
a) Urinalyses
b) CBC count
c) Creatinine
d) Liver function tests
Yearly skin scrapings taken from the 3 or 4 most active lesions are recommended. Successful treatment can result in flattening and elimination of nodules, papules, and once treatment is completed, the patient should be monitored for the next 5-10 years to evaluate for signs of relapse. To date, the relapse rate following completion of multidrug therapy has been 1% for both types of leprosy. Patients who have been successfully treated occasionally develop reversal reactions and further neuropathy.
Preventionp
Information campaigns about leprosy in high-risk areas are essential so that patients and their families, who were historically shunned from their communities, are encouraged to come forward and receive treatment. Early diagnosis and treatment with multidrug therapy is the most effective way of preventing disabilities from leprosy, as well as preventing further transmission of the disease.
Prognosis
Recovery from neurologic impairment is limited, Discoloration and skin damage typically persist. Physical therapy, reconstructive surgery, nerve and tendon transplants, and surgical release of contractures have all contributed to increasing the functional ability in patients with leprosy [24].
Patient Education
Patients with leprosy should be advised about the importance of continuing long-term therapy until the course of antibiotics is completed. The WHO recommends that the monthly administration of rifampin be directly observed. In patient with leprosy they are learn self-care techniques, hygiene, and proper footwear can help prevent ulcer formation and tissue damage. The WHO recommends examination of all household contacts of patients with leprosy, with careful instructions to seek medical care if signs and symptoms of leprosy appear.
Pregnancy in patients with leprosy can result in hormonal changes that lead to suppression of cell-mediated immunity, which may exacerbate symptoms of leprosy. Furthermore, pregnant women with leprosy are at greater risk of developing reactions and relapses. Type 1 reactions are more likely during the first few months following childbirth, whereas type 2 reactions typically occur during the third trimester of pregnancy and during lactation.
These patients have poor immunological resistance. They may hence progress to Lepromatous type. Skin lesions are more numerous and are seen around eyes, nose and mouth. In pure borderline lesions involvement of nasal mucosa is not seen. If nasal mucosal involvement is demonstrated than it will have to be assumed that the lesion has progressed to Lepromatous stage Table 5.
Differential Diagnoses
a) Allergic Contact Dermatitis
b) Superficial mycoses (tinea versicolor)
c) Birthmarks and scars
d) Granuloma multiforme
e) Lupus erythematosus
f) Pityriasis rosacia
g) Diabetes mellitus (neuropathy)
h) Dermatologic Manifestations of Sarcoidosis
i) Drug Eruptions
j) Granuloma Annulare
k) Insect Bites
l) Irritant Contact Dermatitis
m) Leishmaniasis
n) Onchocerciasis (River Blindness)
o) Pediatric Contact Dermatitis
p) Pinta
q) Psoriasis
r) Scabies
s) Syphilis
t) Tinea Versicolor
u) Vitiligo
Leprosy in Romania
In Romania at Tichilesti, a beautiful and clean place in Dobrogea, near Isaccea, Tulcea County: hidden between two hills in a beautiful green area, is the only hospital for lepers in the country also the single leprosarium in EUROPE. Tichilesti now is a strange mixture between hospital and village but at the beginning was a hospital-prison. In the valey are the buildings of the hospital, white-painted dating from 1900, up on the hills covered with forests, are small houses that the lepers have built during their stays.
The hospital in fact now only a nursery is occupied by 23 sick patients 1 doctor -D RAZVAN VASILIU,5 nurses with ten infirmaries , helped by two horses, a cart, a sled, a tractor, three cars, 10 hectares of arable land. At Tichilesti, the patients are old and now healed by the Hansen bacillus, but with fingers, legs, missing eyes, sequelae of a disease .The average age is about 60 years old , the last one brought here, was diagnosed in the 80s is Grisa, the real name being Grigorov Grigore.
The history of the hospital is older than a century, told Dr. Razvan Vasiliu, the director of the institution. By 1900 leprosy was created here in the true sense of the word, meaning a place of isolation, not comfort, on the site of a monastery where some lepers were already being cared for. But in 1916 Dobrogea was occupied by the Bulgarian army, and the southern neighbors abolish the settlement without forgetting to burn it. The 200 interns have fled wherever. After 1928, the authorities of the Greater Romania gather them and drive them back to Tichilesti, where, in the meantime, the hospital had been rebuilt [25].
«For the most part, they have been living here for three, four, even five decades,» says hospital head nurse Cristina Milosovici. Nobody has forgotten that moment, that day when he found out he's different from the others. Later they learned that they suffer from a strange disease, a curse that forces them to live far away from the normal course of life, besides society. None have forgotten and will not forget that day. This is how Cristache Tatulea, the one who is called «the mayor» of the Tichilesti hospital. «he remembers the day he arrived here: May 2, 1949. He was 16 years old.
The internship of life did not prevent Tichilesti patients from being, after all, normal people who had the misfortune to suffer from a malady that disfigures and for which mankind always maintains a current sense of horror. They are not prisoners now; they could leave the hospital anytime, leave, work in fields and sites, as Cristache Tatulea work on a shipyard in Navodari, but struck her legs. Behind the gates of the hospital, the patients fulfill their life loving, married, building houses and a family. Most of the families gave birth to healthy children who were sent far away, in turn, they remain healthy and their children also. So they now use to come in vacations to visit their grandparents, like any other grand children.
With the end of the illness, the history of what the Romanian and foreign press have called the «only leprozerie in Europe» will end, so the place will be transformed into a home for the elderly, and the changes have begun. In the backyard, the elderly and old lepers talk of old friends, proudly that now are real stars, a lots of turists visits the leprosery, take pictures, and they enjoy telling each one their story. All the turist use to bring them cakes, drinks, oranges, apples, or on Easter or Christmas, specific foods like sauseges, eggs, sarmale etc. Also they bring clothes, medical suplies or prosthesis. Periodically doctors of different speciality use to visits them .If is a more serious problem they are bring to the hospital in emergency. This is how I encoutered one of them because of a chronic otomastoiditis with cholesteatoma complicated with meningitis.
They are proud, even they are blind when dr Vasiliu is reading them the articles and use to describe every picture with a plastic description of the expression of the patient, and also use to give them, recommendation for the next time most important person who visits them was Jonathan Scheele. Lepra is define it as a contagious disease, but it is considered as the world less contagious disease between contagious diseases. Most of the time, the leper patient has the source of the infection in the family, according to Rasvan Vasiliu, is that leprosy is contracted in the early years of life. «If you've been 15-20 years old, it’s very hard, but it's not impossible to make leprosy anymore.» It would be very difficult for someone who comes from outside who has never had cases of leprosy in the family and who has an adult age to make illness. Even when there were no effective treatments for the disease, «Vasiliu argues. Hospital staff is the proof because worked in the hospital and not even one got sick with leprosy.
The patients are not carriers of the Hansen bacillus, they are uncontaminated, but they are dependent on medical care because of sequelae that occurred over time. They affected their hands, their feet or their eyes. «Tichilesti Hospital is home to them, most of them are old, here they go to life, they are visited, they go to children, who are healthy, happy that now no one is fraid of them and are free to leave but it’s their home here over time, some patients were discharged and settled in the villages near Tichilesti. The locals looked at them as normal people, of whom they had nothing to fear. In the courtyard of the hospital are two catholic dwellings, an Orthodox church and one Baptist. In this isolated place, viewed by most as a prison, religious freedom has been uninterrupted during the decades of communism.
Discussion
Leprosy was a scourge of medieval Europe. The image of the leper, covered with sores and face or limbs eaten away by infection, ringing a bell to announce his or her presence, remains powerful today. Yet at the beginning of the 16th century, leprosy suddenly changed from being a common to a very rare disease in Western Europe. Microbiologists have long been puzzled by this abrupt retreat. Did a genetic change make the bacteria less infectious and virulent? Was social change responsible? Or might the key factor be a change in human immunity to leprosy? The Journal of Science provides a partial answer, by publishing a genetic study. DNA of Mycobacterium leprae extracted from medieval graves is nearly identical to that of the modern bacterium, so there is no loss of bacterial infectiousness or virulence. Social changes may have played a part but living conditions for most of the population were not that different in 1400 and 1600.
Researchers at the Ecole Polytechnique Federale de Lausanne in Switzerland, most Europeans more resistant than the rest of the world population. But on the other side leprosy considered eradicated in Britain is still present and is often misdiagnosed as a common skin problem, Up to 129 cases were reported in England and Wales between 2001 and 2010. Globally, the majority of the patients with leprosy are from south-east Asia. Two recent cases were of men who had moved to the UK from Asia within the last few years immigrants suffering from leprosy were discovered, even the diagnosis was very difficult, aspects, types of stages re not recommender Both men noticed changes in the skin coloring and sensation but GPs initially thought it was due to skin infections or a form of eczema.
Diagnosis in western populations such as the UK is often delayed because doctors are unaware of the disease's presence in their country, or of its symptoms. Dermatology is not part in GP training to start with, so rare diseases like leprosy are seldom taught. Early diagnosis and treatment are crucial TO AVOID e nerve damage that causes the numbness that can in turn lead to loss of limbs.
Conclusion
a) Mycobacterium leprae and Mycobacterium lepromatosis. (B. Hansen) Although it is not very contagious, it can cause tissue to fall off, rot away, and become deformed.
b) The way it is passed on is by close and frequent contact between a contagious sufferer and a person who is genetically susceptible to developing the disease. Scientists believe that similarly to a cold, it can be passed in droplets of saliva from the nose and mouth.
c) The disease which dates back to 600 BC can strike decades after initial infection and cause lesions on the skin, loss of sensation in affected areas.
d) Historically lepers have often been ostracised by their families and communities, leading to the setting up of leper colonies during the middle.
e) Leprosy may masquerade as various other skin disorders, given its range of symptoms. Due to its rarity in Europe, it may easily be misdiagnosed and consequently pose future health risks for patients if missed.
f) A detailed medical history, including factors like travel to areas where the disease is more common, and examination of the skin and peripheral nerves, together with a high degree of suspicion in individuals at risk, are crucial towards diagnosis and the eventual treatment of leprosy.
g) US researchers announced that they are developing a vaccine against the disease.
h) In the 1990s, the World Health Organization (WHO) launched a campaign to eliminate leprosy as a public health problem by 2000 by using multidrug regimens therapy.
i) The goal of the WHO by the end of 2015 is still not realized they are pleased to reduce the rate of new cases by a more raid diagnosing the disease and multidrug therapy, methods in reducing transmission of the disease in the community.
j) The results are not visible yet because access and delivery of antibiotics continues to be a problem in the most endemic nations. With the precise transmission mechanism of leprosy still unknown and lack of an effective vaccine, leprosy will probably continue to be a public health problem in the coming decades.
References
- Anderson H, Stryjewska B, Boyanton BL, Schwartz MR (2007) Hansen disease in the United States in the 21st century: a review of the literature. Arch Pathol Lab Med Jun 131(6): 982-986.
- Anderson GA (2006) The surgical management of deformities of the hand in leprosy. J Bone Joint Surg Br 88(3): 290-294.
- Bakker MI, Hatta M, Kwenang A, Van Mosseveld P, Faber WR, et al. (2006) Risk factors for developing leprosy a population-based cohort study in Indonesia. Lepr Rev 77(1): 48-61.
- Britton WJ, Lockwood DN (2004) Immunology of Leprosy. Lancet 363(9416): 1209-1219.
- Deps PD, Guedes BV, Bucker Filho J, Andreatta MK, Marcari RS, et al. (2006) Characteristics of known leprosy contact in a high endemic area in Brazil. Lepr Rev 77(1): 34-40.
- Fred Ferri (2015) Leprosy. Ferri's Clinical Advisor 2015: 5 books in (1st Edn.), Philadelphia, PA: Elsevier/Mosby 687e4-687.e5.
- Joyce MP, Scollard DM (2004) Leprosy (Hansen's Disease). Conn’s Current Therapy. pp. 100-105.
- Baton Rouge, Louisiana (2016) Health and Human Resources Administration. Hansens Disease. National Hansen's Disease (Leprosy) Clinical Center.
- Kai M, Nguyen Phuc NH, Miyamoto Y, Maeda Y, Fukutomi Y, et al. (2011) Analysis of Drug-Resistant Strains of Mycobacterium leprae in an Endemic Area of Vietnam. Clin Infect Dis 152(5): e127-e132.
- Jacobson RR, Krahenbuhl JL, Yoder L (2006) Overview of Leprosy.
- (2015) Leprosy (Hansen's disease).
- Leprosy. World Health Organization.
- Moschella SL (2004) An update on the diagnosis and treatment of leprosy. J Am Acad Dermatol 51(3): 417-426.
- National Hansen's Disease (Leprosy) Program. US Department of Health and Human Services.
- Reibel F, Cambau E, Aubry A (2015) Update on the epidemiology, diagnosis, and treatment of leprosy. Medecine et Maladies Infectieuses 45(9): 383-393.
- Singh P, Busso P, Paniz-Mondolfi A, Aranzazu N, Monot M, et al. (2011) Molecular Drug Susceptibility Testing and Genotyping of Mycobacterium leprae Strains from South America. Antimicrob Agents Chemother 55(6): 2971-2973.
- Sridharan R, Lorenzo N, Narasimhan L (2005) Leprosy. Medscape Reference.
- Schreuder PA, Noto S, Richardus JH (2015) Epidemiologic trends of leprosy for the 21st century. Clinics in Dermatology 34(1): 24-31.
- (2016) The World Health Organization. Diagnosis of Leprosy. Leprosy Elimination
- (2014) Tierney D, Nardell EA Leprosy.
- Richard W Truman, Pushpendra Singh, Rahul Sharma, Alberto Paniz- Mondolfi, Adamandia Kapopoulou, et al. (2011) Probable zoonotic leprosy in the southern United States. New England Journal of Medicine 364(17): 1626-1633.
- The World Health Organization. Transmission of Leprosy. Leprosy Elimination.
- US. Department of Health and Human Services. National Hansen's Disease (Leprosy) Program. Health Resources and Services Administration.
- Ustianowski AP, Lockwood DN (2003) Leprosy: current diagnostic and treatment approaches. Curr Opin Infect Dis 16(5): 421-427.
- Walker SL, Lockwood DN (2007) Leprosy. Clin Dermatol 25(2): 165172.





























