Autoimmune Granulomatosis with Polyangiitis or Wegener Granulomatosis
Cristina Otilia Laza1*, Gina Enciu2, Luminita Micu2 and Maria Suta3
1Department of ENT, County Clinical Emergency Hospital of Constanta, Romania
2Department of Anatomo pathology, County Clinical Emergency Hospital of Constanta, Romania
3Department of Rheumatology, County Clinical Emergency Hospital of Constanta, Romania
Submission: February 19, 2018; Published: March 14, 2018
*Corresponding author: Cristina Otilia Laza, Department of ENT, County Clinical Emergency Hospital of Constanta, Romania, Email: cristinaotilia@gmail.com
How to cite this article: Cristina Otilia Laza, Gina Enciu, Luminita Micu, Maria Suta. Autoimmune Granulomatosis with Polyangiitis or Wegener Granulomatosis. Glob J Oto 2018; 13(5): 555871. DOI: 10.19080/GJO.2018.13.555871.
Abstract
Granulomatosis with polyangiitis, formerly known as Wegener granulomatosis, is a disease that typically consists of a triad of airway necrotizing granulomas, systemic vasculitis, and focal glomerulonephritis. If the disease does not involve the kidneys, it is called limited granulomatosis with polyangiitis. The etiology and pathogenesis of WG are unknown. Infectious, genetic, and environmental risk factors and combinations thereof have been proposed. The evidence to date suggests that WG is a complex, immune-mediated disorder in which tissue injury results from the interplay of an initiating inflammatory event and a highly specific immune response. Part of this response consists of the production of ANCA, directed against antigens present within the primary granules of neutrophils and monocytes; these antibodies produce tissue damage by interacting with primed neutrophils and endothelial cells The purpose of this article is to present 4 patients all diagnosed in our department ,with head and neck lesions ,every case with his manifestation and response to the treatment .We consider that a well trained ENT specialist must be able to diagnose and recognize such a disease but this requires knowledge and hard work. In the recent period of time, studies focusing on the suitability of biological agents in modifying the course of both systemic and localised disease have emerged. Spreading knowledge about this modern therapy in Wegener granulomatosis among otolaryngologists may contribute to the improvement of prognosis.
Keywords: Granulomatosis with Polyangiitis; Wegener Granulomatosis; Necrotizing Granulomatous Vasculitis
Introduction
Granulomatosis with polyangiitis (GPA), previously known as Wegener granulomatosis is an idiopathic vasculitis of medium and small arteries, characterized by necrotizing granulomatous inflammation of the respiratory tract with coexisting glomerulonephritis. The estimated incidence in Europe is 5-10 cases per 1 million populations. GPA/WG is generally characterized by antineutrophil cytoplasm antibodies (ANCA), although in rare cases of limited GPA, ANCA may not be present. As is proven in in vitro studies ANCA activate neutrophils, enhance their adherence to endothelium, causing their degranulation and harming endothelial cells [1-3].
The disease affects people at any age, but the most common age of presentation of GPA/WG is the sixth and seventh decade of life. Most often symptoms of GPA/WG belong to classic triad of upper respiratory tract, lungs and kidneys, although any organ may be affected. In 80%-95% of the patients the first symptoms of GPA/WG are otorhinolaryngological manifestations of head and neck .In some cases otorhinolaryngological symptoms are single sign of the disease called "limited GPA" in contrast to more advanced stages with systemic vasculitis called "generalized GPA/WG".
Limited GPA/WG phenotype is often more recurrent and refractory and it is more likely to affect younger and more female population. Generalized GPA/WG typically includes renal and/or pulmonary involvement and systemic symptoms such as fever, asthenia, anorexia or weight loss. Phenotypes of GPA differ from each other also in specific cytokine pattern. The limited form is characterized by Th1 lymphocyte polarization, as opposed to the generalized form with greater Th2 lymphocyte polarization. During the course of GPA/WG, the transformation from limited to generalized form and vice-versa is possible.
Symptoms
Granulomatosis with polyangiitis most commonly occurs in whites during the third to fifth decades of life. Often, the patient initially presents with symptoms that involve the head and neck.: more than 70% of presenting symptoms involve nasal, sinus, ear, or tracheal manifestations . Upper respiratory tract involvement generally precedes pulmonary or renal involvement. Otolaryngologic presenting symptoms of WG are commonly misdiagnosed as infectious or allergic in etiology.
The classic triad of full-blown Wegener granulomatosis (WG) consists of the following:
a. Necrotizing Granulomatous Inflammation of the upper and lower respiratory tracts
b. Systemic vasculitis of small arteries and veins
c. Focal glomerulonephritis
Not all patients show involvement of all 3 areas, and virtually any organ system can be involved. Both limited and systemic variations of the disease have been described, with including the following:
a. Head and neck alone
b. Head and neck and pulmonary
c. Head and neck, pulmonary, and renal
The clinical course can be rapid or indolent. Constitutional signs and symptoms, such as fever, weight loss, and fatigue, are common, but rarely dominate the clinical picture. Nose and sinuses. Sinonasal involvement is the most common manifestation of GPA in the head and neck region, it occurs in up to 85% of patients, and over 25% of patients have only sinonasal symptoms. Tissue damage and bone destruction is caused by reduced blood flow due to vasculitis. Naso-sinusal involvement usually starts in the septum area supplied by Kiesselbach plexus and then spreads to the paranasal sinuses to severe damage of the structures of outer nose, paranasal sinuses and skull base [4-6].
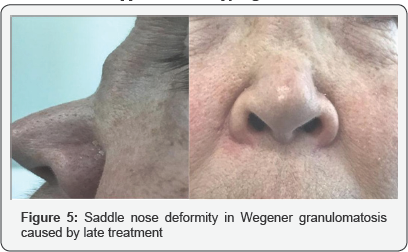
Clinical symptoms
nasal obstruction, purulent discharge, epitasis, crusting are the most frequent -hyposmia, reduction in the sense of smell, cacosmia may appear as a result of purulent secretions associated with growth of bacteria's such as Pseudomonas aeruginosa or Staphylococcus aureus, anemia in severe destructions ,collapse of the nose. Epiphora, other initial sign is caused by involvement of the nasolacrimal duct. Whistling symptoms in perforation of the nasal septum and in the more advanced cases "saddle nose" deformity. Perforations of nasal septum and their expansion can cause collapse of the cartilaginous part of the nose, which results in depressed appearance of the nose, so-called saddle- nose deformity. It deteriorates nasal obstruction and can cause anemia.
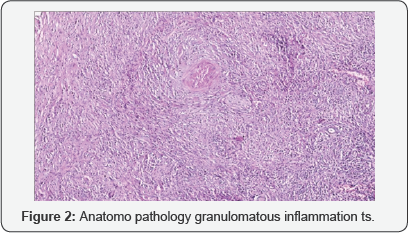
Although that anterior septum supplied by Kiesselbach plexus is the most frequent region of sinonasal GPA, any structure in the sinonasal cavity, including mucosa, turbinates, septum, and sinuses may be affected. For that reason there is an indication to link both flexible endoscopy and CT scans in order to disclose all potential lesions. Treatment of sinonasal GPA is difficult. Standard pharmacology or surgical interventions are often ineffective. To decrease the incidence of sinonasal intensifications culture-directed antibiotics followed by topical antibiotic irrigations can be helpful. Saline high-flow irrigations are also useful as an additional therapy to facilitate mucociliary clearance in affected nasal cavities Figures 1 & 2.

Perforations of nasal septum are generally not treated. Surgical management is not recommended due to poor tissue perfusion, bad wound healing and possible infections. It is vital in planning surgical treatment to identify an adequate period, when GPA is in remission. It is also important to choose suitable method of treatment that will have a chance of success in very poor vascular framework. Anyhow, saddle nose deformity can be successfully operated in the remission phase Chronic sinusitis affects 40-50% of patients with supra infection with true bacteria's or fungus. Although WG is generally less destructive than sinonasal lymphoma, Osteocartilaginous destruction may be revealed by the following:
a) Septal perforation
b) Pain at the nasal dorsum, which suggests chondritis Osteocartilaginous destruction does not correlate closely with active disease. Otologic involvement occurs in 25-40% of patients during the course of Wegener granulomatosis (WG), including external, middle and/or inner ear
c) External ear manifestations can be described as erythematous or ulcerated lesions that mimic perichondritis.
d) Implication of a middle ear is the most common form of otological manifestation of GPA and it usually appears as unilateral or bilateral chronic otitis media with serous effusion and conductive hearing loss. Otitis media occurs in 40-70% of cases and is the most common form of ear involvement in WG.
e) Suppurative otitis media or mastoiditis, with chronic otorrhea, deafness and post auricular pain.
f) Patients may have in 10% direct involvement by WG of the middle ear and/or mastoid mucosa, with resultant necrotizing granuloma and vasculitis this produces middle ear granulation tissue, tympanic perforation, and chronic purulent blood stained drainage. It can lead to extensive tympanic scarring or Granulomatous occlusion that results in persistent conductive hearing loss it is sometimes mistaken for otologic tuberculosis but improves only with the use of gluco corticoid general and local or cytotoxic agents.
g) Serous otitis media is the most prevalent type and is usually secondary to associated nasal disease and subsequent Eustachian tube dysfunction patients with WG require several tympanostomies and Dexamethasone transtimpanic injections during the course of their disease
h) Perichondritis Edema or erythema of the auricle may occur in 15% of WG patients and looks like relapsing polychondritis. The condition responds to treatment with glucocorticoids or cytotoxic agents.
Hearing loss
a) Conductive hearing loss is the most common audio logic finding in WG. It is caused by Otitis media or, less frequently, by direct WG involvement of the middle ear.
b) Sensorineural hearing loss is less common, frequent bilateral, looks flat like in Meniere flat cochlear nerve compression by adjacent granuloma, cochlear immune- complex deposition, and -local vasculitis of the cochlear vessels.
c) Progression is generally rapid; however, the condition is occasionally reversible with glucocorticoids or cytotoxic agents.
d) Secondary infection extending to the inner ear labirinthitis an alternative etiology of sensorineural hearing loss.
e) Vertigo or disequilibrium is rarely reported in WG. Possible causes include the following:
I. Vasculitis of the vestibular inner ear.
II. Granulomatous neuritis of the vestibular portion of cranial nerve VIII (CNVIII).
III. Vestibular deposition of immune complexes.
IV. Central cerebral or cerebellar involvement by WG.
V. Facial paralysis is rare as a presenting sign of primary Wegener granulomatosis (WG) of the middle ear or mastoid. It is caused by necrotizing vasculitis of the vasa nervorum or Neuritis due to Granulomatous involvement of the middle ear. Most cases resolve or improve with cytotoxic therapy; however, permanent facial paralysis secondary to delayed treatment has been reported.
VI. Facial neuropathy has also been reported in the absence of otologic WG involvement.
VII. Multiple cranial neuropathies may exists CNs) VI, VII, IX, and XII in patients with large cranial base lesions and destruction of the petrous portion of the temporal bone.
Hearing loss and vertigo may imitate Cogan syndrome (non syphilitic interstitial keratitis and bilateral audio vestibular deficits), leading to improper diagnosis .Middle ear effusions, resistant to systemic therapy, can be managed with placement of a ventilation tube. Hearing amplification devices may be considered in patients with hearing loss [7-10].
Ophtalmological involvement
a. Nasolacrimal duct obstruction epiphora
b. Orbital Granulomatous pseudo tumor
c. Periorbital edema
d. Chemosis
ii. Proptosis (15%)
iii. necrotizing nodular episcleritis, scleritis, ulcerations, retinal vasculitis corneal
Lungs
a. Dyspnea, cough, hemoptysis
i. Cavitating Granulomatous lesions
ii. Pulmonary parenchyma and bronchi
iii. Chest x-ray: single or multiple (<10) cavitary nodules of 5-100mm in diameter
b. Renal
i. 20 % have renal disease at time of 80% progress to glomerulonephritis
ii. U/A: Hematuria, proteinuria, red cell hypertension, edema casts,
c. Cutaneous
i. Ulcers of distal extremities
ii. Wart-like lesions around the elbows
iii. Pyoderma gangrenosum like lesions
iv. Petechia
v. Crusted plaques
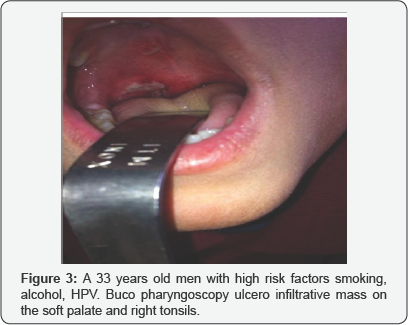
d. Oral or pharyngeal involvement occurs in up to 6% of patients.
e. Mucosal ulcerations are the most common oral lesions, usually buccal but may occur on the tongue, palate, or pharynx. Ulcers are persistent, not recurrent. Biopsy and IHC exam were important; also p ANCA, c ANCA, because they exclude malignancy and the final diagnosis was Wegener granulomatosis.
f. Gingivae are striking red, with variably described white, yellow, or blue areas. Strawberry gingival hyperplasia is path gnomonic for WG and may present as an early manifestation of the disease.
g. There is delayed healing of oral wounds. In time, underlying bone can be involved, leading to tooth mobility or tooth loss.
h. Oriental fistula, Osteonecrosis of the palate, and -labial mucosal nodules.
Oral biopsies are infrequently positive, but they remain important in the role of early diagnosis. Histologic features may be nonspecific-vasculitis and necrotizing granulomas are typically lacking instead, pseudo epitheliomatous hyperplasia, multinucleated giant cells, and inflammatory infiltrates are more common.
Laryngotracheal Involvement in Wegener granulomatosis (WG) may range from subtle hoarseness to stridor and life- threatening obstruction Figure 3.
Subglottic stenosis is the most characteristic and serious laryngeal lesion. It occurs in 16-20% of all patients with WG and up to 50% of pediatric patients with WG, can be the only presenting manifestation of WG. Some researchers have recommended that all patients with subglottic stenosis be evaluated for the presence of cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) and perinuclear ANCA (p-ANCA) as part of the routine laboratory workup.
Although WG is known to contribute to airway narrowing, the disease course of subglottic stenosis is thought to run independent of that involving WG. The immediate subglottic region of the trachea is particularly susceptible to narrowing secondary in part to laryngopharyngeal reflux, limited blood supply, and turbulent airflow and can result in airway compromise. Chronic scarring is thought to be the result of a recurrent insult such as laryngopharyngeal reflux in the presence of WG, rather than ongoing microvasculitis alone. Direct laryngoscopy may show edematous mucosa or bland scar. Biopsy specimens generally demonstrate only fibrosis and inflammation, without evidence of vasculitis.
Patients usually present dyspnea, wheezing or stridor. Cough and hoarseness are observed rarely. Patients with symptoms suggesting presence of subglottic stenosis should be examined with flexible endoscopy and CT imaging only 20% of involved cases diminish with immunotherapy; 80% remain fixed or irreversible because of chronic fibrosis.
Choice of treatment method depends on patient's clinical condition. In less advanced cases pharmacological treatment supported by topic inhaled glucocorticoids or optionally laser therapy can be sufficient. Despite pharmacotherapy up to 80% of patients have to undergo surgical interventions including translational injection of corticosteroids, endoscopic dilation, radial laser incisions, stent placement, tracheostomy or resection of involved segment followed by reconstruction of missing section .Any surgical procedure can lead to an aggravation of stenosis and for this reason it is recommended to initiate therapy with less invasive methods. However acute subglottic stenosis is life-threatening condition and often requires tracheotomy. Supraglottic stenosis is a rare complication. So far, only one case has been reported in the literature [11-14].
Salivary Gland Involvement
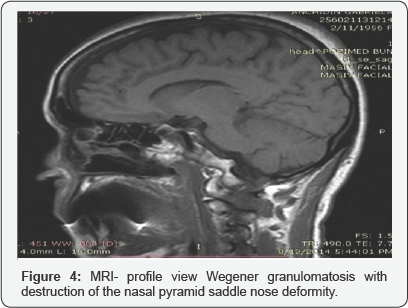
Involvement of the salivary glands is rare in Wegener granulomatosis (WG). It typically occurs early in the course of the disease, with enlargement of the parotids or sub maxillary glands. Extensive involvement of the salivary glands may produce sufficient destruction to simulate Sjogreen syndrome Figure 4.
Differential Diagnosis
a. Strawberry gums
b. Gingival hyperplasia induced by drugs (eg, phenytoin anticonvulsants, some calcium channel blockers, cyclosporine, conjugated estrogens)
c. Sarcoidosis
d. Tuberculosis
e. Leishmaniosis
f. Churg-Strauss syndrome-asthma and eosinophilia
g. Polyarteritis nodosa
h. SLE-systemic eritematous lupus is associated with the presence of immune complex deposition and presence of anti-dsDNA or anti-Sm antibodies, which are not present in other potential diseases
i. Scurvy (vitamin C deficiency)
j. Neoplastic processes (squamous cell carcinoma, leukemia, Kaposi sarcoma, TK/NK lymphoma)
k. Nasal substance abuse cocaine
l. Drug reaction propylthiouracil, methimazole, carbimazole, benzyl thiouracil, hydralazine, antitumor necrosis factor-a (anti-TNF-a), sulfasalazine, D-penicillamine, and minocycline
Diagnostic
According to Criteria of the American College of Rheumatology (ACR; 1990), GPA is diagnosed if 2 or more of the following 4 criteria are met:
A. Sinus involvement;
B. Lung X-ray showing nodules, a fixed pulmonary infiltrate or cavities;
C. Urinary sediment with hematuria or red cell casts; and
D. Histological granulomas within an artery or in the perivascular area of an artery or arteriole.
Laboratory findings in WG
a. CBC-normochromic normocytic anemia; thrombocytosis;
b. PCR ,RF positive ,ERS -high levels fibrinogen high
c. hyperglobulinemia, particularly of IgA.
d. Urine-analysis
e. The discovery in 1985 of auto antibodies directed against the cytoplasmic constituents of neutrophils (antineutrophil cytoplasmic antibody [ANCA] in patients with WG was a major advance in the diagnosis and understanding of WG.
Currently in clinical practice diagnosis is usually based on presence of distinctive ANCA and biopsy of affected organ. The main component of GPA diagnostics is serologic evaluation of cytoplasmic pattern of ANCA.
a. ANCA, mainly of the IgG type, are targeted against proteinase 3 (cytoplasmic anti-neutrophil cytoplasmic antibody, c-ANCA) or myeloperoxidase (perinuclear- antineutrophil cytoplasmic antibody, p-ANCA). Both main neutrophil granule components.
b. To determine level of ANCA immuno fluorescence and enzyme-linked immuno sorbent assay are used c-ANCA are specific for GPA, while P-ANCA is associated with inflammatory bowel disease, rheumatoid arthritis, autoimmune liver disease etc.
c. In generalized GPA, ANCA are elevated in 90%-95% of patients, in limited stage of GPA in the ear-nose-throat regions in only 46%-70% of patients Imaging Studies X-ray-chest, sinuses CT, MRI sinuses-inflammation of mucosa of the nasal sinuses, serous otitis bone destruction of the nasal cavity, maxillary sinuses and mastoid air cells, as well as sclerosing osteitis and bony thickening in the same locations, CT-lung, abdominal Pulmonary testing-Spyrometry, Bronchoscopy- biopsy renal biopsy Audiometry pure tone, vocal audiometry and immitance audiometry Fibroscopy /endoscopy of the nasal cavities , ears ,pharynx ,larynx . Biopsy The diagnosis of WG is made histologically by the presence of necrosis, Granulomatous inflammation with multinucleated giant cells, vasculitis, and micro abscess formation. IHC Biopsy is usually used when ANCA testing is non diagnostic or uncertain. In positive biopsies Granulomatous inflammation including palisading granulomas, scattered giant cells, vasculitis or necrotizing granulomata can be found .In localized disease, the role of the biopsy increases, because localized GPA has lower decisive predictive value of c-ANCA. In those patients biopsy should be performed to avoid oversight of c-ANCA negative GPA .Because up to 50% of specimens may be non diagnostic, in some patients repeat biopsies are necessary.
Prognosis
The Wegener granulomatosis is a serious disease, mean survival time of untreated generalized is 5 months 2 years due to renal or lung failure. Modern immunosuppressive treatments methods greatly improved patient outcomes and estimated median survival time to 21.7 years after diagnosis.. Approximately 20% of patients, even with therapy, eventually succumb to the disease or to the therapy [15-17].
Treatment
Treatment of GPA must be individualized to every patient and is divided in two phases
1. Induction is the first phase; the main goal of the first phase is rapid remission, which should last up to 6 months depending on clinical condition.
2. Maintenance, the second phase, which lasts 12-24 months, with the purpose to maintain remission and prevent aggravation of disease. According to the current recommendations for generalized GPA/WG the induction phase is based on combination of systemic corticosteroid and immunosuppressant therapy Figure 5.
Typical gluco corticoid therapy includes
a. Oral prednisone administration (starting prednisone - 1 mg/kg/day with a max 80 mg/day -reduction after 3-4 weeks.
b. intravenous bolus of methyl-prednisolone (7.5-15 mg/ kg/day) for 1-3 days in severe cases followed by oral therapy
Immunosuppressant
Cyclophosphamide (CYC) (alkylating agent) is in first- line of treatment (standard dose is 2mg/kg/day or 600mg/ m2). Every 2 weeks for 1 month (at a dose of 600mg/m2) and subsequently modified dosage until achieving remission, as low as possible toxicity Rituximab (RTX) (anti-CD20 monoclonal antibody) is offered to patients with a relapse after complete cycle of CYC or CYC is contraindicated. RTX should be given once a week at a dose of 375 mg/m2 for a month. RTX is preferred over CYC in premenopausal women, because of the potential induction of infertility of CYC. In severe cases of GPA/WG with pulmonary hemorrhage, plasma-exchange therapy combined with corticosteroid and immunosuppressant is recommended Other agents that have demonstrated effectiveness in small- scale studies are purine and pyrimidine anti metabolites, mycophenolate mofetil (anti proliferative agent), leflunomide (anti proliferative agent), anti thymocyte globulin (T-cell depletion antibody), and 15-deoxyspergualin (inhibitor of interleukin-2-stimulated maturation of T cells) Anti-TNF-a biological drugs have shown positive effects - infliximab but no significant with etanercept (TNF inhibitor) Table 1.

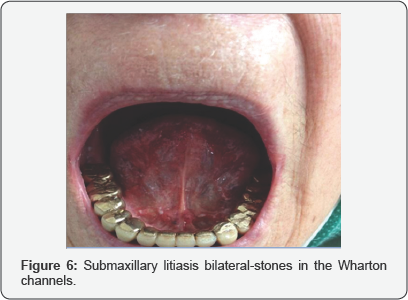
Intravenous immunoglobulin (IV Ig) can be considered when corticosteroids and CYC fail however, there is not any therapeutic advantage in patients with GPA plus is very expensive. Abatacept (inhibitor of CTLA-4 signals to T-cells) is proven to be associated with a high percentage of disease remission. The maintenance phase, which is introduced after remission achievement, lasts up to 24 months and is based on oral corticosteroids and azathioprine/methotrexate. Discontinuation or use of low doses of maintenance therapy is associated with a higher relapse rate Figure 6.
RTX can be used as maintenance therapy as an alternative to azathioprine but the optimal RTX dosing schedule, however, remains to be determined. In order to avoid Pneumocystis jiroverci infection, trimetoprim/sulfamethoxazole should be given during whole immunosuppressive therapy. Surgical treatment ought to be considered for patients who are not responding to pharmacotherapy. There is a wide variety of procedures that patients may undergo including
a) dacrio-cysto-rhinostomy-for stenosis of the nasolacrimal channel,
b) myringotomy or mastoidectomy for middle ear inj with steroids transtympanic in serous otitis
c) transtympanic aerator in serous otitis deafness caused by the disease involving middle or inner ear ,or caused by the treatment special treatment or hearing aids Treatment Sino nasal Disease
d) Low-dose systemic steroids, topical nasal steroids, saline irrigations, or antibiotics when bacterial super infection is suspected
e) FESS for chronic sinusitis
Rinoplasty repair of saddle nose deformity and septal perforation Laryngeal Disease (subglottic stenosis)
a. Medical management- Immunosuppressant and high dose steroids 2 therapy
b. Acute Airway obstruction-Tracheostomy
c. Subglottic stenosis Dilatation + Intra-lesion steroids or topical Mitomycin C
MLSS -suspended laryngoscopy with microscope and with CO2 laser, diode , Gouveris et al. Better report long term results with CO2 laser+ intralesional triamcinolone + topical mitomycin c and post-op immuno suppressants + PPI
a. Stents-for stenosis of the inferior trachea, bronchi
b. Resection and end to end anastomosis in tracheal circular stenosis -and stent Montgomery T-tube for 6 months-1 year
c. Laryngo tracheoplasty anterior ,enlargement with epiglottis ,posterior enlargement type Rhetti ,trachea-plasty with septal cartilage or from the ribs etc
The prognosis of WG has dramatically improved from a mortality rate of 82% before the era of immunosuppressive therapy to the current remission rate of more than 75% with appropriate medical therapy. Starting with ENT symptoms we diagnose 4 cases of Wegener Granulomatosis -
Case Report
Case Nr 1
First case was diagnose 7 years ago and is a men 53 years old -at the time of the diagnosis, now 60 years old, with risk factors smoking 2 packs of cigarettes on a day ,heavy intake in the same time of alcohol presenting with an oropharyngeal tonsilar ulceration ,was first consider as a cancer type epidermoid carcinoma, Biopsy indicate Granulomatous inflammation with vasculitis ,and IHC confirm, PCR ,RF ,ESR were very elevated -so we run a battery of test including p-ANCA ,and c-ANCA and were positive.
The response to steroids was amazing with ulceration disappeared in 4 month ,and the inflammatory tests improved in the a same time The patient is on Imuran and a low doses of Medrol and amazing till now no other symptom or sign of affecting another organ appear .Also he change his life styles, so he left alcohol and tobacco. He respects always the follow-up program.
Case Nr 2
6 years ago we admit in the ENT Clinic a 52 years old lady complaining of fever , headache ,mainly frontal ,on the face and nasal pyramid , purulent blood stained discharge , severe nasal obstruction bilateral ,posterior discharge , odynophagia. Also she accuses bilateral otalgia with hypoacusis.
Clinical examination, nasopharyngeal endoscopy ,imaging CT-contrast sinuses, otoscopy , immitance audiometry and pure tone audiometry seems to reveal a patient with Suppurative polypoidal pansinusitis and serous acute otitis .We start the treatment with Antibiotics iv, NSAIDS, ntiasal saline lavages, local antibiotics and steroids, antialergic, mucolitics but the response was low and what was weird was that the nonspecific inflammatory test were higher and higher every week.
We decide to perform FESS functional endoscopic surgery under GA, and we have the surprise to discover a biopsy with Granulomatous inflammation and vasculitis. We realize the importance of PCR, ESR, RF and order, p-ANCA, c-ANCA, Antinuclear Antibodies .so we sustain the diagnosis of Wegener Granulomatosis She was transfer to the rheumatology, she starts the treatment with steroids and Imuran-azathioprine and we continue our procedure for cleaning the sinuses and middle ear .with complete success. Till now she never complain of sinusal or ear problems but she developed pulmonary lesions with cough, discharge, haemoptysis, night sweats and X-ray revealed bilateral nodules, non cavitating. She was sending in pneumology department for pulmonary test, bronchoscopy, biopsy and they confirm vasculitis. For this reason they change the treatment returning at iv methyl-prednisolone and Rituximab. She is send periodically for an ENT examination, and till now she is in good status.
Case Nr 3
Is a 57 years old women complaining of headache, frontal, pain on the nasal pyramid, nasal obstruction and purulent discharge .4 years ago she was admitted in the clinic but at least 6 months she consult ENT doctors, also oro-maxillo facial surgeons for gingivitis. MRI exam revealed an intense inflammation in the nasal cavities on the mucosa lining the nasal septum, biopsy anatomo pathology IHC,PCR, ESR ,RF fibrinogen very elevated p ANCA, c ANCA, Ac anti EBV, Ac Antinuclear, Ac anti AND, etc.
When we contact a specialist in rheumatology to initiate the treatment, a few nodules appear in the left breast. In case of suspicion of cancer the immunosuppressive treatment is completely not recommended, so we think that at least local steroids we can use, and the patient left for biopsy-surgery etc. 6 months they continue to repeat biopsy, considering that inflammation can be only tuberculosis in origin, without looking at the diagnosis already establish, After 6 month of surgeries and difficulties to heal our lady return but with severe problems like Otitis supurative chronic right side and Serous otitis -on the left side, Deafness mix right side, conductive right side, Nasal pyramid deformed with saddle nose, Nasosinusal infection with Staphylococcus aureus, Inflammation with granulations and ulceration, hypertrophic pink granulose gingivitis [18-20].
Candidiasis, glosittis, Laryngitis catarrhal with dysphonia. I start in emergency treatment for sinusitis, otitis deafness, dysphonia and I finally present her to prof Maria Suta Rheumatology Department. She start the treatment with steroids and methotrexate than in the end they decrease the doses of steroids and in the and now is on low dose of Imuran. I succeed to clean the sinuses and nasal cavities, now clear, but narrow -with local steroids, antibiotics, permanent saline lavage, vit A, E, local gels with emollient and reparative actions substance like hyaluronic acid. Also after we surgical remove the granulose, polypoidal tissue from the right ear with supurative process, the eardrum perforation healed completely, on the right side we treat the serous otitis with steroids. Dexamethasone trans tympanic injections.
The pharynx, larynx was normal. Audiometry pure tone and immitance audiometry were also normal. Finally our patient was very happy to return to his work as a violin -music teacher .Still is coming periodically for a complete endoscopy and otoscopy, hearing test or if a few problems appeared like- recurrent litiasis in the submaxilary and lacrimal glands, and serous otitis bilateral after an Acute respiratory infection, tympanostomy was necessary plus transtympanic injections .Also she required repeated extraction of lachrymal and salivary stones.
Recently after the retirement of prof. Suta she was given in care to another dr who suddenly without a reason change the treatment completely even there were no clinical symptoms or laboratory changes ,replacing Imuran with Cyclosporine without admission in the clinic. Suddenly all naso sinusal, pharyngeal, otic symptoms reappeared more severe with dysphonia and dyspnoea with subglottic inflammation. Also she starts to present complications caused by medication most frequent ocular with ulceration of the cornea and keratitis. MRI was very useful to revealed inflammation of mucosa in the noses, ENT inuses, ears, pharynx and larynx and trachea bronchi but endoscopic no ulcerations or granulomas were found just inflammation with risk of subglotic stenosis. For this reason we ask help from another reference Rheumatology Clinic ,where under supervision of president of the Romanian Rheumatology Society ,they remove Cyclosporine and start with Solu-medrole plus Cyclophosphamide and progressive all the symptoms even complications disappears, also the lab test were much improved and even subglottic inflammation disappear. We still have problems with crusts in the nasal cavities, also pain on the nasal bones without redness but still signs that at the place of the saddle nose the process is still active. Also just now the perforation in the nasal septum appears. She returns to her job and never miss a follow-up session. Now the main problem is the gastro oesophageal reflux.
Case Nr 4
Was discovered 2 years ago, a 55 years old lady with naso-sinusal complains mainly on the left side, with nasal obstruction, purulent fetid discharge, headache, fever, bilateral otalgia, purulent left otorrhea, hearing loss, vertigo. After a complete general and ENT examination-including endoscopy of the nasal cavities, rhino pharynx, and hypo pharynx, larynx, otoscopy microscopic examination of the ears, we conclude that is a Pansinusitis on the left size possible odontogenic in origin, complicated with bilateral otitis media, but suppurated on the left size. We start in emergency treatment with Levofloxacin, saline, local antibiotics Neomycin, nasal local steroids-Mometasone- Nasonex, auricular aspirations of pus with instillation of drops with moxifloxacine. In this time we run a battery of lab test like: -CBC-leucocitosis, with neutrophila, anemia. ESR, PCR, fibrinogen very elevated we explore the hepatic, renal function, metabolism smear from the nose and ear for microbiological ,mycological exam s plus antibiogram, fungigram. CT scan sinuses, ears, mastoid processes revealed important inflammation of the pituitary mucosa with level of pus in the sinuses and complete opacity on the maxillary left sinus, with specific aspect like fungal sinusitis, also osteitis, liquid and thickening of the mucosa of the middle ears and mastoid cells. We decide after 2 weeks of intense general and local treatment that an endoscopic sinus surgery is required, nasal smear Klebsiella pneumoniae, Pseudomonas aeruginosa, the last one in the left ear also .Both germs were sensible to Levofloxacin, so we keep it but we include Amykacin. After the surgery, biopsy indicate Granulomatous infection, with necrosis so we order c-ANCA, p-ANCA slight positives After the transfer to the Rheumatology she start the treatment with methyl prednisolone and azathioprine, we continue local treatment for the nose, sinuses and ears, but the results clinical and lab test were not good. They change the treatment but even with larger doses or new drugs the results were discouraging.
Because at the last examination, we discover important necrosis on the posterior part of the nasal left cavity, with a permanent Suppurative fetid process I have to think at a possible lymphoma TK/NK, so I repeat biopsy and order IHC, for T cells Killer and Natural Killer. We still wait for the results, because in this time the patient is feeling worse than ever, with fever, severe pain, fetid nasal and auricular discharge ,dizziness deafness, tinnitus, she lost weight and lab tests are worst than ever
Discussion
a. Wegener Granulomatosis was first described by Klinger in 1933, followed by other investigators, including Rossle in 1933, Wegener in 1936 and 1939, and Ringertz in 1947.
b. WG/GPA is currently characterized as one of the ANCA- associated small vessel vasculitides. With predilection the upper and lower respiratory tracts are affected also lungs and kidneys. Histologic presence of necrosis, Granulomatous inflammation, and vasculitis are specific.
c. There is a strong and specific association with auto antibodies directed against proteinase 3, a constituent of neutrophil azurophilic granules. The presence of antibodies is an indicator for a diagnosis of WG/GPA, but it cannot replace biopsy.
d. The presence of ANCA is not required to make a diagnosis of WG/GIA by either the American College of Rheumatology (ACR) definitions. Occasionally, patients with infections, neoplasms, inflammatory bowel disease, sclerosing cholangitis and other rheumatologic diseases develop ANCA, predominantly perinuclear ANCA-s or exhibit an atypical staining pattern.
e. Most patients are white, the sex distribution is equal, and most present in the fifth decade, although the age range extends to both extremes.
f. The clinical presentation of WG/GPA can be so diverse that the list of differential diagnoses is vast, ranging from infections (fungal, bacterial, and mycobacterial) to other vasculitides, like, Polyarteritis nodosa , Horton, s temporal arteritis, Henoch-Schonlein purpura, sarcoidosis, LED, Behcet syndrome, and malignancies.
g. Unexplained constitutional symptoms as initial presentation are fever and weight loss but more frequently they appear during the illness.
h. The upper airway disease is the most common presenting feature of WG./GPA This includes sinusitis, oral lesions (ulcer, gingivitis), otitis media, hearing loss, epistaxis, and saddle nose deformity; sinusitis is the most frequent initial presentation in about half to two thirds of patients with WG/GPA.
i. Pulmonary involvement is one of the cardinal features of WG/GPA .in 45% of patients at presentation and 87% during the course of the disease. Cough, hemoptysis, and pleuritis are the most common pulmonary symptoms. The most common radiographic findings include pulmonary infiltrate (67%) and nodules (58%).
j. Renal disease also may be seen as the initial presentation or during the course of the disease. Once present, renal disease may progress from asymptomatic and mild to fulminant glomerulonephritis within days or weeks, resulting in end-stage renal failure.
k. Ocular manifestations have been reported to occur in 28 to 58% of patients with WG/GPA, and they may be part of the initial presentation in 8 to 16% of patients. A complete ophthalmologic examination, CT or MRI of the orbits and sinuses may provide useful anatomic information.
l. Other unusual presentations of WG/GPA include salivary gland, cutaneous, gastrointestinal, and cardiac involvement. .In our case breast lesions are very rare.
Conclusion
Oto-rhinolaryngologist is the first physician to contact for the majority of patients with GPA. This diagnosis must always be taken into consideration in patients with recurrent upper respiratory tract infections, otitis, mucosal ulcers and laryngitis. Even rare Granulomatous diseases, vasculitis and autoimmune diseases must be taking in consideration because of their frequent manifestation in ENT areas. So its important for an ENT specialist to be well inform and to detain solid knowledge about this type of diseases. Proper and early diagnosis is crucial for imminent therapy implementation and allows avoiding irreversible organ damage, see mutilation like saddle nose Studies, which appeared recently, create prospect for the introduction of less toxic and more effective treatment of GPA with biological agents.
References
- Belloso A, Estrach C, Keith AO (2008) Supraglottic stenosis in localized Wegener granulomatosis. Ear Nose Throat J 87(7): E11-E14.
- Comarmond C, Cacoub P (2014) Granulomatosis with polyangiitis (Wegener): clinical aspects and treatment. Autoimmun Rev 13(11): 1121-1125.
- Daum TE, Specks U, Colby TV, Edell ES, Brutinel MW, et al. (1995) Tracheobronchial involvement in Wegener's granulomatosis. Am J Respir Crit Care Med 151(2 Pt 1): 522-526.
- Daikeler T, Kistler AD, Martin PY, Vogt B, Huynh Do U (2015) The role of rituximab in the treatment of ANCA-associated vasculitides (AAV). Swiss Med Wkly 145: w14103.
- Erickson VR, Hwang PH (2007) Wegener's granulomatosis: trends in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg 15(3): 170-176.
- Fortin PM, Tejani AM, Bassett K, Musini VM (2013) Intravenous immunoglobulin as adjuvant therapy for Wegener's granulomatosis. Cochrane Database Syst Rev 1(3): CD007057.
- Gottschlich S, Ambrosch P, Kramkowski D, Laudien M, Buchelt T, et al. (2006) Head and neck manifestations of Wegener's granulomatosis. Rhinology 44(4): 227-233.
- Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaitre O, et al. (2014) Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med 371(19): 1771-1780.
- Holle JU, Gross WL (2013) Treatment of ANCA-associated vasculitides (AAV). Autoimmun Rev 12(4): 483-486.
- Jones RB, Tervaert JW, Hauser T, Luqmani R, Morgan MD, et al. (2010) Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med 363(3): 211-220.
- Leavitt RY, Fauci AS, Bloch DA, Michel BA, Hunder GG, et al. (1990) The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum 33(8): 1101-1107.
- Lloyd G, Lund VJ, Beale T, Howard D (2002) Rhinologic changes in Wegener's granulomatosis. J Laryngol Otol 116(7): 565-569.
- Mansi IA, Opran A, Rosner F (2002) ANCA-associated small-vessel vasculitis. Am Fam Physician 65(8): 1615-1620.
- Martinez Del Pero M, Chaudhry A, Jones RB, Sivasothy P, Jani P, et al. (2009) B-cell depletion with rituximab for refractory head and neck Wegener's granulomatosis: a cohort study. Clin Otolaryngol 34(4): 328-335.
- Rao JK, Weinberger M, Oddone EZ, Allen NB, Landsman P, et al. (1995) The role of antineutrophil cytoplasmic antibody (c-ANCA) testing in the diagnosis of Wegener granulomatosis. A literature review and meta-analysis. Ann Intern Med 123(12): 925-932.
- Rasmussen N (2001) Management of the ear, nose, and throat manifestations of Wegener granulomatosis: an otorhinolaryngologist's perspective. Curr Opin Rheumatol 13(1): 3-11.
- Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, et al. (2010) Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med 363(3): 221-232.
- Watts RA, Lane SE, Scott DG, Nossent H, Gonzalez-Gay MA, et al. (2001) Epidemiology of vasculitis in Europe. Ann Rheum Dis 60(12): 11561157.
- Wong RJ, Gliklich RE, Rubin PA, Goodman M (1998) Bilateral nasolacrimal duct obstruction managed with endoscopic techniques. Arch Otolaryngol Head Neck Surg 124(6): 703-706.
- Wawrzycka K, Szczeklik K, Darczuk D, Lipska W, Szczeklik W, et al. (2014) Strawberry gingivitis as the first manifestation of granulomatosis with polyangiitis. Pol Arch Med Wewn 124(10): 551-552.





