Migrainous Vertigo: Evaluation and Treatment
Constantinos Avraamides*
University College London, Europe
Submission: June 18, 2016; Published: July 12, 2016
*Corresponding author: Constantinos Avraamides, UCL (University College London), Ifigenias 48A, Strovolos 2007, Nicosia Cyprus, Europe, Tel: +35722446810 Email: avraamides@ hearingaids.com.cy
How to cite this article: Constantinos A. Migrainous Vertigo: Evaluation and Treatment. Glob J Oto. 2016; 1(4): 555566. DOI: 10.19080/GJO.2016.01.555566
Abstract
Migrainous vertigo (MV) is a disorder that many patients or clinicians can accidently ignore due to the variation of its symptoms. Although much research took place about migrainous vertigo from numerous medical organizations, such as the International Headache Society (IHS) [1], MV is not formally considered to be a medical disorder. Scientists nowadays study epidemiology, aetiology and clinical features of this disorder in order to have the ability to recognize and different diagnose migrainous vertigo form other similar disorders. The lack of information about MV leads to misdiagnose patient with that specific condition which at the end causes even more problems such as mistreatment or no treatment at all. As a matter of fact MV can vary between patients and that makes the diagnosis even more complex but challenging for the clinicians. Moreover there is growing recognition of a syndrome called vestibular migraine Kayan [2], which is vertigo directly caused by migraine.
Epidemiology
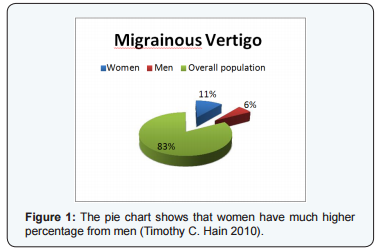
Epidemiology is an important part to monitor. With the knowledge of it you can find common factors that may lead to the actual disorder and that may help you to develop a treatment of the disorder. Neuhauser et al. [3] set the lifetime frequency of MV to be 0.98%. In isolation migraine and vertigo are the two most ordinary causes for visits to the G.P. Migrainous vertigo occurs at all ages; about 5% of men have migraine (Figure 1) (Table 1) Hain [4]. Women of childbearing age have greater occurrence, up to approximately 10% at the onset of menstruation, and escalating to nearly 30% at the peak age of 35years. During menopause, rates of migraine rapidly turn down in women back to, about, 10%. As I have mentioned before, a more recent study recommended that 88% of 2991 patients who had diagnosed themselves as having sinus headache, actually had migraine Hain [4].
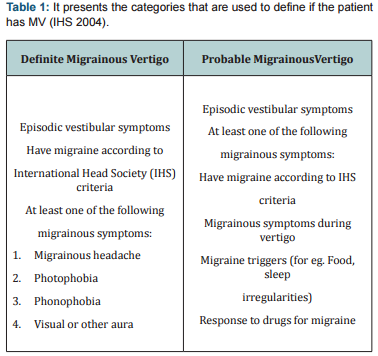
That is an enormous amount of patients and by that we can understand how many patients might not be diagnosed with MV due to that concept. Based on this argument, it is important to mention that the International Headache Society has not yet included migrainous vertigo as a recognized medical condition, although other organizations have included it. Neuhauser and Lempert suggest that patients with definite MV present recurrent episodic vestibular symptoms of at least moderate severity; current or previous history of migraine, migrainous symptoms such as headache, photophobia, phonophobia or other aura symptoms during at least two vertiginous attacks. Patients may report primarily rotational vertigo, though vertigo may be positional and the patient may grieve only head motion intolerance.
The duration of symptoms varies from few seconds to several days and vertigo does not need to be simultaneous to migrainous headache. This is a big disadvantage because it is not easy to identify it. However, those criteria are not clear enough to give scientists the ability to correctly identify migrainous vertigo and it is easily understood that if some criteria are not universal then they are not easily acceptable around the globe. Finally patients with migrainous vertigo might experience hearing loss but it is quite rare. Furthermore vestibular testing might have normal results.
Aetiology
Aetiology of migrainous vertigo is not known (IHS 2004). Due to limited investigation studies during the acute phase of the attack, we cannot be sure about the aetiology. Ii is well known that peripheral lesions are important to investigate during the acute phase but it is also easily understood that is not always possible. In bibliography it is commonly written that migrainous vertigo can be carried on through families (IHS 2004). Medication also could lead to this disorder and by this I include patients who take birth control pills, vasodilators or other drugs. Other trigger factors may be some kinds of food and alcohol. Another reason, which is not well defined, is motion sickness. Through different studies, scientist seems to believe that motion sickness might be a trigger for migrainous vertigo.
As I have mentioned before, aetiology of migrainous vertigo is not know; there are many factors that may lead to that situation but there is no “golden” rule that we can assume. Scientists believe that migrainous vertigo is a central disorder causing peripheral problems. Vertigo is a part of that general disorder and it is strongly believed that it is happening due to a pathophysiology higher up in the cerebellum or in the brain. That pathophysiology can cause vertigo or give the feeling of imbalance. Furthermore it is not known by now what is causing that specific situation; but it is acceptable that more likely the problem is located in the neurotransmitter release. However this theory cannot explain the variation between patients. Other well-known disorders, with a problem in neurotransmitter release, are not developing such a variation of symptoms.
Clinical Characteristics
As deep as you search in that area you are going to find many sources explaining the characteristics of that disorder. Although due to the limited population based studies, the findings are not helpful and they can vary between them. Neuhauser et al. [5] suggest that migrainous vertigo can last from seconds to days. That range is quite broad though and it can be helpful only if you try to exclude other disorders rather than just predict that it is MV, just from the duration. In addition Neuhauser et al. [5] mention that most of the patients experience longer lasting attacks, which could be sustained for hours to days. Audiological failure is not common in that specific disorder, Neuhauser et al. [5] suggest that the greater percentage of the migrainous vertigo population don’t face any hearing loss; but if they do so, the hearing loss is mild to moderate and it is progressively reduced when the acute phase of the attack is relaxing.
In addition, patients with MV may not have phonophobia nor photophobia, which due to IHS are crucial symptoms for diagnosis. Moreover migraine might follow vertigo, or the opposite, vertigo might follow migraine. It is also common to have migraine and vertigo at the same time Ballenger [6]. These findings though are debatable due to the limitation of the case studies. Unfortunately these findings are what we have available and it is what we build on our case studies.
Differential Diagnosis
As it was previously described, differential diagnosis of migrainous vertigo is not an easy situation. That is happening due to the limited research in that specific area. Clinicians do not have a ‘gold standard’ test to diagnose migainous vertigo. By recording a good history of the patient is always helpful and that might guide you to the actual disorder. A family history record is essential and, if the clinician has the experience to take a good family and medical history, can actually diagnose the disorder. Asking the ‘good’ questions is a really difficult thing to do though. Clinicians are interested to know when the attack occur, they want to know about the duration of that attack, they also want to know if basilar migraine. Basilar migraine is a disorder, which lasts for 5-60 minutes together with vertigo.
In addition patients experience aura and other symptoms like diplopia and dysarthria. Neuhauser in an article recommended that quite a few MV patients are satisfying these criteria. One other disease that clinicians must exclude is Meniere’s disease. Meniere’s comes with a triad of symptoms that make it really obvious. From many studies like Neuhauser and Lempert it is shown that half of the Meniere’s population experience, also, at least one migraine attack. When the clinicians are recording the medical history it is important to check for the three symptoms of Meniere’s such as low frequency hearing loss, tinnitus and vertigo. A differential diagnosis is difficult and the only way to have it right is to exclude other disorders and take a good medical and family history. That ability is coming with experience and if a clinician is not sure about the diagnosis he/she is making is always better to ask someone with more experience. Our goal is always to give to the patient the best treatment for the problem he/she actually has.
Management and Rehabilitation
In my opinion, the lack of a golden standard diagnostic test leads to a lack of a golden standard treatment. Scientists, such as Neuhauser et al. [5], suggested that the treatment of migrainous vertigo most of the time is aiming the reduction of the migraine with respect to vestibular disorder. Migraine rehabilitation is not complicated and its aim is to avoid migraine triggers (red wine, cheese, chocolate, stress and many more). In addition to this prophylactic treatment, clinicians suggest patients to accept a pharmacological treatment. One of the most commonly used drugs in the treatment of migraine, during the attack, is triptans, which is in the family of drugs called ‘agonists’. Moreover it is important to act before you face the actual problem, so there are some drugs that the patient uses as a prophylaxis Brandt [7].
Propanolol, amitriptyline, valproate and tropiramate are a small part of a big family of drugs that clinicians can use to help patient with migraine. Medications are given to prevent or reduce the number of attacks in patients who experience frequent migraines. Commonly, these medications act over time to avoid blood-vessel swelling. In addition a treatment about vertigo is very vital. Clinicians can use vestibular suppressions such as Stemetil and Meclizin and vestibular rehabilitation. Moreover physiotherapy seems to help patients with migrainous vertigo. Physiotherapy aims to re-establish the body to a normal working state by employing techniques such as massage, manipulation, mobilisation, heat and hydrotherapy [8]. Physiotherapist suggested that migraine might be caused due to problems in the neck structure. Physiotherapy can help solve such problems.
Conclusion
Taking all points into consideration, by searching the bibliography about migrainous vertigo the first thing you can easily realise is the lack of information about this disorder. The lack of diagnostic criteria and also the absence of a specific treatment are making that disorder even more challenging for clinicians. As far as I understood migrainous vertigo is a variable disorder, speaking about the clinical features. That characteristic of the disorder, make it difficult to diagnoses and therefore treat. Clinicians must always remember that a good medical history is the A to Z in that specific disorder. Moreover due to the lack of information is essential, as clinicians, to keep on a database in order to expand the efficiency of the diagnosis and treatment.
Treatment of migrainous vertigo is split into two different categories. Prophylactic treatment is essential for patients but is also important for clinicians in order to know how to treat the acute phase of the disorder. Drugs are mostly used to treat this specific disorder.
Even though giving the drugs to the patient you might instantly help him/her, you must always have in mind that you must have a limitation in giving drugs to patients. As clinicians our first and only goal is to provide a good treatment to our patients, that statement is not easy but in my point of view that is what we should try to do because people don’t care how much you know, until they know how much you care there are other specific rising difficulties during the attacks or if there is a specific pattern of the attack. Furthermore information about family history of migraines or migrainous vertigo is essential for the differential diagnosis of the disorder. Due to the fact that migrainous vertigo is mostly a peripheral disorder, MRI scans are not really helpful because they appear normal after the attacks. PET scans during the attacks will give information to clinicians about the areas in the brain that are affected. Long lasting migraine attacks might distort brain image, which can be seen from MRI scans.
References
- Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders. Cephalalgia 24(1): 24-49.
- Kayan A (2003) Migraine Related Vertigo Classification and Diagnostic Criteria. Nottingham.
- Lempert T, Neuhauser H (2005) Migrainous Vertigo. Neurologic Clinics 23: 715-730.
- McMurray J (2010) Clinical practice. Systolic heart failure. N Engl J Med 362(3): 228-238.
- Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T (2001) The Interrelations of Migraine, Vertigo, and Migrainous Vertigo. Neurology 56(4): 436-441.
- Ballenger JJ (2009) Ballenger’s Otorhinolarygology 17 Head and Neck Surgery. Centennial, PMPH, USA.
- Brandt T (2003) Its Multisensory Syndrome. (2nd ed). Vertigo, Springer, Germany
- Park JH, Viirre E (2009) Vestibular Migraine May Be An Important Cause Of Dizziness/Vertigo in Perimenopausal Period. Med Hypotheses 75(5): 409-414.





