A New Electromagnetic Technology as a Strategy to Help the Recovery of the Anterior Cruciate Ligament Injury in Athletes: A Pilot Study
Francesco Zingale1, Beatrice Marina Pennati2*, Alessandra Comito2, Filippo Fioriti3, Stefano Fiorini3 and Gabriele Mascherini4
1University of Florence, Firenze, Italy
2El.En. Group, 50041, Calenzano, Italy
3Prosperius Lab - Villa Cherubini Insitute, Florence, Italy
4Sports and Exercise Medicine Unit, Clinical and Experimental Department, University of Florence, Firenze, Italy
Submission:October 06, 2023;Published:October 18, 2023
*Corresponding author:Beatrice Marina Pennati, El.En. Group, 50041 Calenzano, Italy
How to cite this article: Francesco Z, Beatrice Marina P, Alessandra C, Filippo F, Stefano F. A New Electromagnetic Technology as a Strategy to Help the Recovery of the Anterior Cruciate Ligament Injury in Athletes: A Pilot Study. Glob J Addict Rehabil Med. 2023; 7(3): 555713. DOI: 10.19080/GJARM.2023.07.555713.
Abstract
Background: Because of its anatomical location, the knee joint has to sustain enormous forces during exercise and physical activity. One of the most frequent damage affecting ligaments in the lower body is the Anterior Cruciate Ligament (ACL) injury. Treatment may include rest and rehabilitation physical exercises. This study wanted to explore an alternative method for supporting ACL injury recovery using an electromagnetic device for young athletes.
Methods: A total of 10 athletes, 4 females and 6 males, who had undergone ACL surgery for the first time were considered. They ranged from 15 to 22 years.
Results: After two months of follow-up from the experiment starting time, our results showed for every patient an evident muscle tonification in both limbs.
Conclusion: Our data showed that for athletes combining physical exercises with the electro-magnetic technology had led to a significant and positive improvement in muscle tone and strength without discomfort or side effects in patients after ACL surgery. A milder approach gives the athlete a gradual recovery and a variable intervention window based on the patient’s characteristics and personal needs. The device we used represents valuable and effective support that could be widely employed in the physiotherapy field.
Keywords: Physiotherapy; FMS (Flat Magnetic Stimulation); Muscle toning, Athletes; Anterior cruciate ligament (ACL) injury; Cryotherapy; Electrostimulation; Heterogeneity; Echography; Homologous limb; Neurological diseases
Introduction
Because of its anatomical location, the knee joint has to sustain enormous forces during exercise and physical activity. Therefore, it is not surprising that 15-30% of sport-related injuries affect this body structure [1]. Confirming this, Swenson et al. [2] carried out a retrospective study in several American high schools describing knee injury rates by sport, accounting for 15.2% of all high school sport-related damages [2]. One of the most important ligaments in the lower body is the Anterior Cruciate Ligament (ACL). This is a key structure in stabilizing the knee joint and connecting the femur to the tibia, so it is crucial for daily life activities and sports [3]. ACL injury is widespread, especially in under-25-years subjects and specifically in sports that involve sudden stops or changes in direction, jumping, and landing (soccer, basketball, football, downhill skiing) [1,4]. The main symptoms reported are pain, swelling, and difficulty moving the joint. Depending on the severity of the ACL injury, treatment may include rest and rehabilitation physical exercises on both legs, electrostimulation, and cryotherapy [5] to help regain strength and stability. Similarly, when the damage is too consistent, and surgery is needed to replace the torn ligament, pre-and post-surgery physiotherapy is crucial for a rapid and effective recovery, as well as all the abovementioned strategies [6]. Therefore, maximizing muscle mass is the primary strategy in the athletes’ population. Even if there are several preventive programs in the physiotherapy routine, the possibility of re-injury is very high, with a second ACL injury rate of 23% in under 25 years athletes who return to sport within two years from the first reconstructive surgery [7,8]. In addition, the risk of injury on the same knee lasts for five years from the first lesion [9].
Although in recent years, the sports sector has raised a solid and challenging need for quick muscular injury recovery, there is substantial heterogeneity in the ACL rehabilitation protocols available in the scientific literature. Criteria for managing the athlete’s signs of progress are not standardised as well as the follow-up timings and the requirements that should be met before returning to sport [10]. Indeed, Magnetic Resonance Modelling with electromagnetic technology is the latest advancement in non-invasive muscle toning [11-17]. Magnetic stimulation has been used to effectively treat various medical conditions, such as urogynecological, neuro-psychiatric, and musculoskeletal disorders [18-20]. Furthermore, athletes show different muscle fiber compositions depending on the sport: a marathon runner may have approximately 80% low-twitch red fibers, while this percentage is lower in a sprinter. Thus, choosing personalised and efficient strategies is crucial, especially after surgery. In this scenario, this pilot study wanted to explore an alternative method for supporting ALC injury recovery using an electromagnetic device for young athletes. The technology used is Flat Magnetic Stimulation (FMS), which can make a muscle passively contract without brain involvement.
Materials and Methods
All treatments were performed at Prosperius Lab at Villa Cherubini clinic in Florence between February and April 2022.
Study Population
A total of 10 athletes, 4 females and 6 males, who had undergone ACL surgery for the first time were considered for the treatment. They ranged from 15 to 22 years old with a mean age of 19 years old. General Information, such as the type of sport performed, injury, and date of birth, was collected for every patient. Specific physiotherapy was performed during the whole study period but just the injured limb was treated with electromagnetic technology while the other was considered as a control.
Device technology
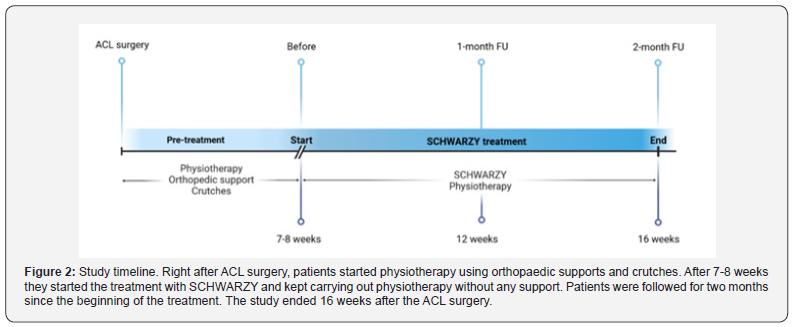
The device system is a medical device used primarily for body fat reduction and body remodelling [21] but it has already demonstrated its potential as a muscle-toning tool [22,23]. The patients were treated on the injured limb with the device using the Flat Magnetic Stimulation (FMS) technology, which made the muscles move without brain involvement thanks to up to two pads applied on a specific body area. Right after ACL surgery and for 7-8 weeks (“pre-treatment” step), the patients started a rehabilitation process with physiotherapy, orthopaedic devices and crutches (see Figure 2 for the study timeline). Thus, the study population was considered moderately active with normal muscle tone and the treatment with SCHWARZY started 7-8 weeks after the ACL surgery (still further supported with physiotherapy exercises only). They were treated for 27 sessions (9 weeks, 2 months of follow-up), three times a week. For all the treatments, the Muscle “Shaping 1” protocol was used. It is characterised by the alternation of muscle contraction and resting steps, repeated in series, to avoid lactic acid formation. Moreover, the stimuli are trapezoidal-shaped, and the frequency is adjustable (around 25 Hz).
Physiotherapy protocols
Patients were involved in a dedicated physical activity to make the athlete regain the ability to bend the knee of about 130° after 4-5 weeks from the treatment start (stretching and pull-ups). Moreover, specific exercises were performed to improve proprioceptive ability (balance exercise devices), muscle flexibility, and strength (exercise bike, treadmill, skill mill). All the activities were repeated ten times per session and slowly increased based on the patient’s feedback.
Functional Measurements
A monthly medical visit was conducted for every patient for three months. The muscular trophism of the quadriceps was evaluated during every session: the thigh circumference was taken on the standing patient at 6 cm, 12 cm, and 20 cm from the kneecap top, respectively. The mean value of three measurements was reported.
Statistical Analysis
A paired Student’s t-test was used to compare the treated and treated legs of every patient Statistical significance is accepted to be p < 0.05. Moreover, with the ANOVA test, data groups regarding the differences in the volume of both treated and not treated thighs were compared. In addition, the variability within these data was calculated with the variability between the groups. Statistical interpretations were carried out with the SPSS program version 25.0 (IBM).
Results
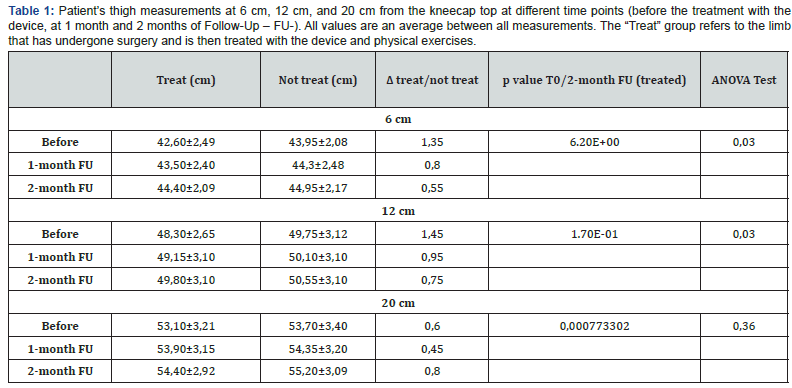
The type of injury, sport, and treated limb are specified. Soccer was the most common sport (4/10, 40%), followed by athletics (2/10, 20%), taekwondo (1/10, 10%), jujitsu (1/10, 10%), tennis (1/10, 10%), and rugby (1/10, 10%). In two (2/10, 20%) patients, a medial meniscus injury was present besides the ACL injury, and one patient had damage to both menisci (1/10, 10%). There was no relevant difference between the incidence of ACL injury in the right or left thigh. After two months of follow-up from the experiment starting time (see “Before” rows in Table 1), our results showed for every patient an evident muscle tonification in both limbs. Table 1 shows the patient’s thigh measurements (averages) at different distances from the kneecap top (6, 12, 20cm), and the difference in thigh circumference values (Δ) between the treated and not treated limbs. Measurements were taken two months after the surgery (“Before” in Table 1), then at three months (1-month Follow Up - FU -) and four months from the surgery (2-months FU). Standard deviation (STDEV) values are also reported. The STDEV ranges are wide because all the patients were considered at the same time. Moreover, we performed a paired Student’s t-test comparing values of a single thigh from the same patient at the beginning and at the end of the treatment. Overall, for treated and not treated limbs, a p-value <0.05 was obtained. Whereas, when the Student’s t-test is carried out considering treated and not treated limbs at a fixed timepoint, results were not statistically significant (p>0.05). When the ANOVA test is performed, only the 20cm measurement results are not statistically significant even if a slight increment is present.

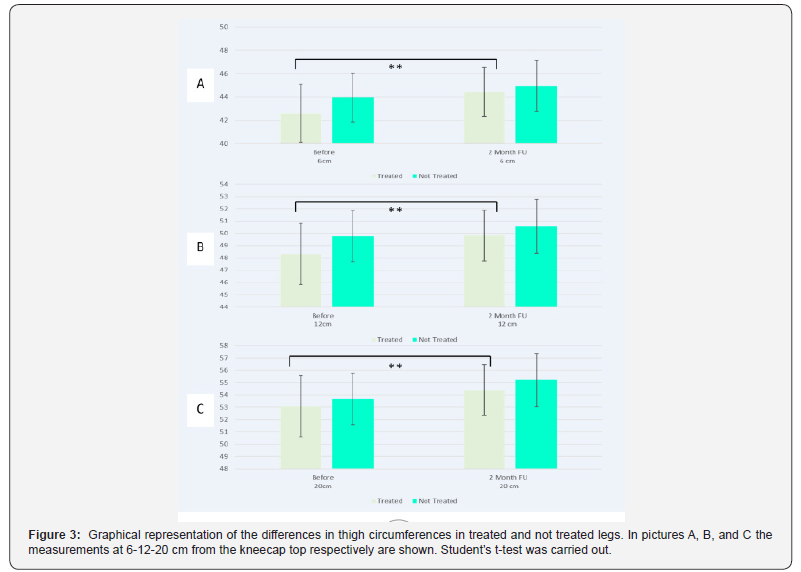
A graphical representation of the differences in thigh circumferences in treated and not-treated legs at different time points is reported in Figure 3. Even if the difference was slight, in all cases, it was bigger before the beginning of the treatment with the device combined with physical exercises than the followups. Specifically, considering the treated legs, the mean difference before the treatment and after 2 months of follow-up was 1.80 cm at 6cm from the kneecap, 1.50cm at 12cm, and 1.30cm at 20cm.
Discussion
Our data showed that for athletes combining physical exercises with the Flat Magnetic Stimulation technology had led to a significant and positive improvement in muscle tone and strength. Confirming these findings, Leone et al [22] previously reported that with the same technology, it was possible to obtain an increase in muscle thickness ranging from 14% to 23%. Similarly, in our results, there was no statistically significant difference between the treated and not treated thighs but a considerable diversity between measurements of the same limb at the experiment starting point and after two months of follow-up. Data analysis with the ANOVA test proved to be ineffective when measurements at 20cm are considered. Although there is a slight increase, this fact could be due to the anatomical area involved. Indeed, it is the rectus femoris muscle that probably had a minor decrease in muscle trophism after the surgery. Nevertheless, our results showed a general increase in dimensions and circumference in treated limbs suggesting a probable improvement in muscle strength. The diversity between the legs’ dimensions can be explained by the lighter protocol used (“Shaping 1”) for the experiment. A milder approach gives the athlete a gradual recovery and a variable intervention window based on the patient’s characteristics and personal needs. However, low-frequency levels and the “Rest-Hold-Fall” shape of the impulse can be modified if needed. As a matter of fact, having the possibility of a 1-50Hz frequency range and different shapes of impulse (square wave, ladder, sinusoidal, trapezoidal), have opened the device employment to various medical areas. Moreover, it is widely demonstrated that electromagnetic waves can have many applications. For example, there is a chair-shaped device that, thanks to the TOP Flat Magnetic Stimulation (TMS), is now largely used for the treatment of urinary incontinence, persistent vulvar pain and vulvodynia, and other disorders and dysfunctions with remarkable results [24-26]. In conclusion, the use of non-invasive medical strategies represents an incentive for the patient to pursue the treatment and improve their quality of life.
Study Limitations and future perspectives
Our future goal will be to increase the number of patients, including a control group, and employ multiple study device protocols. Specifically, it would be more advisable to have a control group not receiving any treatment with Flat Magnetic stimulation. Indeed, previous studies demonstrated that crosseducation can happen. This implies a strength gain in the contralateral limb following a unilateral training program on the homologous limb [27]. Due to this, unilateral training of the unaffected limb has been proposed as a therapeutic approach to help gain strength and skills in patients with acute injuries, immobilisations, or musculoskeletal and unilateral neurological diseases [27,28]. Furthermore, muscular strength and tone need to be thoroughly investigated. For example, it would be interesting to collect qualitative data such as echography or ultrasound [29] exams to assess muscle improvement and evaluate the patient’s comfort and satisfaction levels to determine compliance with the treatment. We also hypothesise that an increase in trophism can correlate with a stabilization of the athlete’s sports activities and that after ACL reconstruction, it might be important to use therapeutic strategies that decrease the loss of muscle strength through central neural mechanisms. In addition, we think that the innovative technology we propose in this study could be a valuable opportunity to treat fragile population categories such as the elderly and disabled who need to improve and maintain muscle tonicity [30].
References
- Parkkari J, Pasanen K, Manila VM, Kannus P, Rimpelä A (2008) The risk for a cruciate ligament injury of the knee in ad-olescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med 42(6): 422-426.
- Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, et al. (2013) Epidemiology of knee injuries among us high school athletes, 2005/06–2010/11 Med Sci Sports Exerc 45(3): 462-469
- Diermeier TA, Rothrauff BB, Engebretsen L, Lynch A, Svantesson E, et al. (2021) Treatment after ACL injury: Panther Symposium ACL Treatment Consensus Group. Br J Sports Med 55(1): 14-22.
- Moses B, Orchard J, Orchard J (2012) Systematic review: Annual incidence of ACL injury and surgery in various populations. Res Sports Med 20(3-4): 157-179.
- van Melick N, van Cingel REH, Brooijmans F, Neeter C, van Tienen T, et al. (2016) Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 50(24): 1506-1515.
- Hartigan EH, Axe MJ, Snyder ML (2010) Time Line for Noncopers to Pass Return-to-Sports Criteria After Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther 40(3): 141-154.
- Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, et al. (2016) Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med 44(7): 1861-1876.
- Paterno M, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2014) Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. American Journal of Sports Medicine 42(7): 1567-1573.
- Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and con-tralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21(8): 948-957.
- Andrade R, Pereira R, van Cingel R, Staal JB, Espregueira-Mendes J (2020) How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med 54(9): 512-519.
- Langeard A, Bigot L, Chastan N, Gauthier A (2017) Does neuromuscular electrical stimulation training of the lower limb have functional effects on the elderly?: A systematic review. Exp Gerontol 91: 88-98.
- Matsuse H, Hashida R, Takano Y, Omoto M, Nago T, et al. (2017) Walking Exercise Simultaneously Com-bined With Neuromuscular Electrical Stimulation of Antagonists Resistance Improved Muscle Strength, Physical Function, and Knee Pain in Symptomatic Knee Osteoarthritis: A Single-Arm Study. J Strength Cond Res 31(1): 171-180.
- Alon G, McCombe SA, Koutsantonis S, Stumphauzer LJ, Burgwin KC, et al. (1987) Comparison of the effects of electrical stimulation and exercise on abdominal musculature. J Orthop Sports Phys Ther 8(12): 567-573.
- Han TR, Shin HI, Kim IS (2006) Magnetic stimulation of the quadriceps femoris muscle: comparison of pain with electrical stimulation. Am J Phys Med Rehabil 85(7): 593-599.
- Makarov S, Bogdanov G, Noetscher G, Appleyard W, Ludwig R, (2019) Design and Analysis of a Whole-Body Noncontact Electromagnetic Subthreshold Stimulation Device with Field Modulation Targeting Nonspecific Neuropathic Pain. Brain and Human Body Modeling, pp. 85-123.
- Mezzana P, Pieri L, Leone A, Fusco I , Schwarzy (2021) The new system for muscle toning and body shaping. J Cosmet Dermatol 20(8): 2678-2680.
- Katz B, Bard R, Goldfarb R, Shiloh A, Kenolova D (2019) Ultrasound Assessment of Subcutaneous Abdominal Fat Thickness After Treatments With a High-Intensity Focused Electromagnetic Field Device: A Multicenter Study. Dermatol Surg 45(12): 1542-1548.
- Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Avanzini G, (2009) Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120(12): 2008-2039.
- Yokoyama T, Fujita O, Nishiguchi J, Nozaki K, Nose H, (2004) Extracorporeal magnetic innervation treatment for urinary incontinence. Int J Urol 11(8): 602-606.
- Biondo A, Gonzalez Isaza P, Fusco I (2022) Efficacy of Top Flat Magnetic Stimulation Technology for Female Stress and Urge Urinary Incontinence: A Clinical Evaluation. World Journal of Nephrology and Urology 11(1) : 18-23
- Nisticò SP, Bonan P, Coli F, Verdelli A, Fusco I, et al. (2022) A New Protocol to Treat Abdominal Subcutaneous Fat Combining Microwaves and Flat magnetic stimulation. Bioengineering 9(5): 182.
- Leone A, Piccolo D, Conforti C, Pieri L, Fusco I (2021) Evaluation of safety and efficacy of a new device for muscle toning and body shaping. J Cosmet Dermatol 20(12): 3863-3870.
- Negosanti F, Cannarozzo G, Zingoni T, Leone A, Fusco I (2022) Is It Possible to Reshape the Body and Tone It at the Same Time? Schwarzy: The New Technology for Body Sculpting. Bioengineering 9(7): 284.
- Biondo A, Murina F, Fusco I (2022) Treatment of Pelvic Floor Hypertonic Disorders with top Flat Magnetic Stimulation in Women with Vestibulodynia: A Pilot Study. J Women’s Health Dev 5(2): 175-84.
- Isaza PG, Borrego RS,Fusco I (2022) A case of stress urinary incontinence after radical prostatectomy successfully treated with an innovative device based on top flat magnetic stimulation. World J Urol 40(7): 1887-1889.
- Lopopolo G, Salsi B, Banfi A, Isaza PG, Fusco I . Is It Possible to Improve Urinary Incontinence and Quality of Life in Female Patients? A Clinical Evaluation of the Efficacy of Top Flat Magnetic Stimulation Technology. Bioengineering 9(4): 140.
- Green LA, Gabriel DA (2018) The effect of unilateral training on contralateral limb strength in young, older, and patient populations: a metaanalysis of cross education. Phys Ther Rev 23(4-5): 238-249.
- Manca A, Hortobágyi T, Carroll TJ, Enoka RM, Farthing JP, et al. (2021) Contralateral effects of unilateral strength and skill training: modified Delphi consensus to establish key aspects of cross-education. Sports Med 51(1): 11-20.
- Nisticò SP, Bonan P, Coli F, Verdelli A, Fusco I, et al. (2022) A New Protocol to Treat Abdominal Subcutaneous Fat Combining Microwaves and Flat magnetic stim-ulation. Bioengineering 9(5): 182.
- Hodges PW, Tucker K (2011) Moving differently in pain: a new theory to explain the adaptation to pain. Pain 152(suppl 3): S90-S98.