Abstract
BCCs are one of the most common malignant tumors worldwide. The global incidence of BCCs is increasing the article describes Basal cell cancers and the anatomical locations these cancers are present. This association is important to Dermatologists, Plastic surgeons, oncosurgeons as well as General Surgeons. Anatomic sites may determine course, management, prognosis and outcome in most cases.
Aim: The aim of the article is to provide all updated and renewed information about Basal cell cancers in different positions in body, the anatomic sites of occurrence and associations with different Syndromic entities.
Method: Review of literature from all standard text, latest references from standard indexed journals taken to verify the associations.
Conclusion: The incidence of Basal Cell cancers is increasing globally. The incidence is increasing not only in normal anatomic sites where these cancers are usually found but also in atypical or rare locations. An extensive and careful study of lesions such as non-healing ulcers should be extensively sought so as to rule out BCC.
Keywords:Ultraviolet; Dermis; Exposed; Trunk; Head and neck; Rodent; Metastasis
Abbreviations:WHO: World Health Organization; BCCs: Basal Cell Cancers
Introduction
Basal cell carcinomas are common of skin cancers and belong to keratinocyte cancers. The incidence of BCCs is dramatically increasing globally and are the most common cancers among fair-skinned populations worldwide. Australia has the highest incidence. Asian and African origin people are also showing a marked increase in incidence and now BCC is one of the most common types of skin cancer in certain populations such as among individuals of Asian or African origin. BCC is not as common in blacks as in white population [1]. It is the most common cutaneous malignancy of white skinned people and second most common cutaneous malignancy in dark skinned people [2]. The Head and Neck region is the Anatomically favoured site [3,4]. UV radiation has been implicated in development of Skin cancers. UV radiation is the major risk factor for BCC as well as SCC, their anatomical distributions differ. It has been seen that there is a considerable difference in anatomic locations. The Squamous cell carcinoma occurs primarily on sites mostly exposed to sunlight such as the face and exposed parts of the upper and lower limbs, whereas BCC occurs also on these sites and those less frequently exposed to sunlight such as the trunk. Sunbathing increases the risk [5].
BCCs are one of the most common malignant tumors worldwide with skin involvement. According to the World Health Organization (WHO), BCCs represent malignant tumors which have originated from basal cells found in the inter-follicular epidermis or in the hair follicle. Although the reporting of BCC cases is not precise, its global incidence is increasing, affecting approximately one million new patients each year. BCC typically presents as a reddish or pinkish shiny nodule or macule with telengastasia. It may enlarge in course of time with ulceration often described as Rodent Ulcer. Basal cell cancers in darker population are difficult to detect clinically as pearly borders and telengiactasis are difficult to see in these individuals. Thus, they are detected at late stages or advanced stages in black populations. More than 80 Percent occurs in head and neck region.
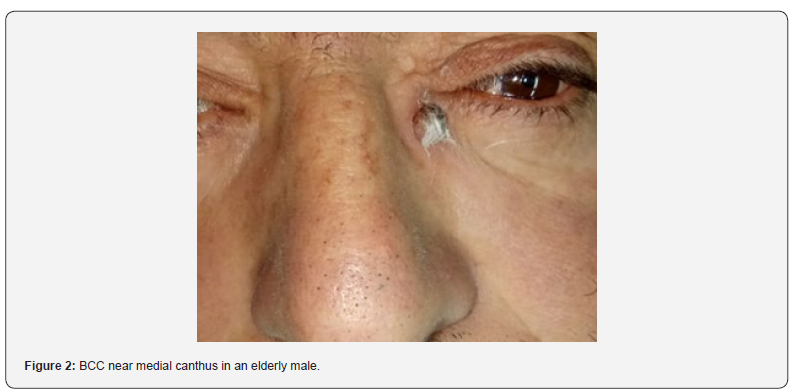
Face, nose, cheek, Nasolabial folds and eyelids are the most common sites followed by Shoulder, back or chest. Malar region and nose are common sites for BCC [6,7]. Superficial BCCs are common on Shoulder, back or chest. BCCs around auricle are also reported. Most cases of BCC are reported from the face. This is followed by cases of BCC on nose or lateral aspect of the nose. The other sites effects are forehead, lips and scalp. Reports of BCC in Back and Axillary region are also reported [8]. BCCS can have varied presentations such as a non-healing ulcer, a pigmented lesion, a crusted lesion or a bleeding ulcer. Xeroderma pigmentosa, Basal Cell Nevus syndrome Rombo syndrome and Bazex Dupre Christol syndrome predispose to BCC.
BCC may also arise from atypical anatomical locations, such as the oral cavity or the vulva [9]. BCCs at these sites are not typically associated with UV radiation exposure as a primary risk factor, as these are sun protected areas. This suggests a possible explanation of multiple other risk factors such as chronic inflammation, immune suppression, Immunosuppression because of drugs, conditions like HIV, Organ Transplant procedures, Diseases such as Paget’s disease of the vulva or lichen sclerosus to be important causative factors. Vulvar BCCs are rare and account for 2 percent of vulvar malignancies [10,11]. BCCs also develop at the site of a burn scar, or even from a benign tumor-like lesion, such as a verruca vulgaris but association with Vitilgo is rare [12].
Differences in anatomic location may also contribute to the formation of different BCC histologic subtypes. Evaluation of tumor anatomical distribution revealed that the head and neck were the most frequent sites of tumor occurrence in both sexes. In considering gender difference, it was found that variations in the anatomical distribution where the scalp, ears and extremities were less common involved more females than males. Also, more than 65 % of BCCs in female patients occurred on the face, followed by the scalp in 21.7%. Considering sun exposure as the likely main cause of the disease, the difference may be explained by women’s clothing style (veil) in our region according to the religious customs (Figures 1-3).

Conclusion
The incidence of Basal Cell cancers is increasing globally not only in the developed world but in underdeveloped countries as well. In addition to normal anatomic sites where these cancers are usually found but also in atypical or rare locations. With more reporting of cases and increase in literature a direct relation with more evidence based statistical analysis would get clearer as far as location and prognosis and treatment of BCCS in relation to Anatomic sites is concerned.
Conflict of Interest
Nil.

References
- Wong CS, Strange RC, Lear JT (2003) Basal cell carcinoma. BMJ 327(7418): 794-798.
- Khullar G, Saikia UN, De D, Radotra BD (2014) Nonmelanoma skin cancers: An Indian perspective. Indian J Dermatopathol Diagn Dermatol 1(2): 55-62.
- D Farhi, N Dupin, A Palangie, A Carlotti, MF Avril (2007) Incomplete excision of basal cell carcinoma: rate and associated factors among 362 consecutive cases,” Dermatologic Surgery 33(10): 1207-1214.
- V Smith, S Walton (2011) “Treatment of facial basal cell carcinoma: a review. Journal of Skin Cancer p. 7.
- Zhang M, Qureshi AA, Geller AC, Frazier L, Hunter DJ, et al. (2012) Use of tanning beds and incidence of skin cancer. J Clin Oncol 30(14): 1588-1593.
- Vuyk HD, Cook TD (1997) Auricular reconstruction after Moh's surgery. A review Face 5: 9-21.
- Telfer NR, Colver GB, Morton CA (2008) British Association of Dermatologists. Guidelines for the management of basal cell carcinoma. Br J Dermatol 159(1): 35-48.
- Tambe SA, Ghate SS, Jerajani HR (2013) Adenoid type of basal cell carcinoma: Rare histopathological variant at an unusual location. Indian J Dermatol 58(2): 159.
- Cömert Asuman, Akin Özlem, Tümerdem Burçak (2008) An Unusual Location of Basal Cell Carcinoma: The Clitoris and the Vulva. Indian J Dermatol 53(4): 192-194.
- Mulayim N, Silver DF, Ocal IT, Babalola E (2002) Vulvar basal cell carcinoma: Two unusual presentations and review of the literature. Gynecol Oncol 85: 532-537.
- Michael A Finan, Gregg Barre (2003) Bartholin's gland carcinoma, malignant melanoma and other rare tumours of the vulva. Best Pract Res Clin Obstet Gynecol 17(4): 609-633.
- Fiszon-Cerqueira L, Ramos-E-Silva M, Guerreiro FB, Cistaro-Serrano M, Carneiro AHC, et al. (2019) Giant basal cell carcinoma associated with vitiligo. Clin Case Rep. 7(9): 1782-1786.






























