Abstract
Post-transplant lymphoproliferative disorder (PTLD) is a serious and heterogeneous complication following solid organ transplantation, particularly liver transplantation. This review provides an in-depth look at PTLD, with a focus on its pathogenesis, clinical presentation, and management in liver transplant recipients. The pathogenesis is multifactorial, with Epstein-Barr virus (EBV) playing a central role, especially in EBV-seronegative recipients, and its development is driven by the intensity of immunosuppression.
We discuss the current WHO classification and the varied clinical presentations, with a particular focus on gastrointestinal and graft involvement. The management of PTLD is risk-adapted, starting with a reduction of immunosuppression (RIS) and escalating to rituximab monotherapy for CD20-positive disease. High-risk or refractory cases require combination chemoimmunotherapy, with promising emerging therapies like EBV-specific cytotoxic T lymphocytes (CTLs) for EBV-positive disease. Prognosis has improved but remains highly dependent on factors such as EBV status, PTLD subtype, and age, with pediatric patients generally having better outcomes.
Keywords:Post-Transplant Lymphoproliferative Disorder; Liver Transplantation; EBV; Lymphoma
Abbreviations: PTLD: Post-Transplant Lymphoproliferative Disorder; EBV: Epstein-Barr Virus; WHO: World Health Organization; GI: Gastrointestinal; CNS: Central Nervous System; PCR: Polymerase Chain Reaction; CT: Computed Tomography; PET-CT: Positron Emission Tomography-Computed Tomography; MRI: Magnetic Resonance Imaging; CSF: Cerebrospinal Fluid; EBER: EBV-Encoded RNA; RIS: Reduction of Immunosuppression; CTLs: Cytotoxic T Lymphocytes; IIM: Idiopathic Inflammatory Myositis; PM: Polymyositis; NHL: Non-Hodgkin Lymphoma; DLBCL: Diffuse Large B-cell Lymphoma; NK: Natural Killer; R-CHOP: Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisone; ATG: Anti-thymocyte Globulin; OKT3: Orthoclone OKT3; PLoS: Public Library of Science; TP53: Tumor Protein 53; GVHD: Graft-Versus-Host Disease; CAR: Chimeric Antigen Receptor; FDA: Food and Drug Administration; PARP: Poly ADP Ribose Polymerase; VEGF: Vascular Endothelial Growth Factor; TKIs: Tyrosine Kinase Inhibitors; FRα: Folate Receptor Alpha; IVIG: Intravenous Immunoglobulin; AI: Artificial Intelligence; BRCA: Breast Cancer gene
Introduction
Post-transplant lymphoproliferative disorder (PTLD) encompasses a heterogeneous group of lymphoid proliferations that arise because of immunosuppression following solid organ transplantation, most commonly manifesting as B-cell neoplasms with variable clinical behavior and histopathology [1-4]. PTLD is recognized as one of the most serious and potentially fatal complications after liver transplantation, with significant implications for patient morbidity and mortality [5-8]. The pathogenesis is closely linked to impaired immune surveillance, often in the context of Epstein-Barr virus (EBV) infection, particularly in EBV-seronegative recipients who acquire primary EBV infection post-transplant [1,2,4,8,9-12].
The incidence of PTLD after liver transplantation varies by age group and center, but large cohort studies consistently report a higher risk in pediatric recipients compared to adults. Recent data indicate an incidence of approximately 2–4% in adult liver transplant recipients and up to 5–11% in pediatric populations, with onset typically within the first-year post-transplant but cases occurring throughout long-term follow-up [1-3,5,12,14]. Pediatric patients are disproportionately affected due to higher rates of EBV Sero negativity at the time of transplantation, while adults may experience later-onset, often EBV-negative PTLD [1,3- 4,6-10,12]. The clinical spectrum ranges from benign polyclonal proliferations to aggressive monomorphic lymphomas, with monomorphic PTLD and poor performance status at diagnosis associated with worse outcomes [1,13].
Historically, the recognition of PTLD as a distinct posttransplant complication has evolved in parallel with advances in immunosuppressive regimens and improved transplant survival [4,9]. Early reports highlighted the increased risk of lymphoid neoplasms in transplant recipients, and subsequent studies have clarified the role of EBV, immunosuppression intensity, and underlying liver disease in modulating risk [3-4,6,9,11]. Despite improvements in diagnosis and management, PTLD remains a major challenge, with mortality rates as high as 50% in some cohorts [7,13]. This review aims to provide a comprehensive and up-to-date synthesis of current knowledge regarding PTLD following liver transplantation. By integrating recent advances and ongoing controversies, this article seeks to inform clinical practice and highlight areas for future research in the prevention and treatment of PTLD after liver transplantation [1-13].
Pathogenesis and Risk Factors
Post-transplant lymphoproliferative disorder (PTLD) represents a spectrum of lymphoid proliferations, most commonly of B-cell origin, arising in the context of impaired immune surveillance following solid organ transplantation, including liver transplantation [1-2]. The pathogenesis is multifactorial, with Epstein-Barr virus (EBV) playing a central role in most cases, particularly in early-onset PTLD.
Role of Epstein-Barr Virus and B-cell Proliferation
EBV is a ubiquitous gammaherpesvirus with tropism for B lymphocytes. In immunocompetent hosts, EBV infection is typically controlled by robust cytotoxic T-cell and natural killer cell responses, limiting the proliferation of infected B cells [4,7]. However, in transplant recipients, immunosuppressive therapy impairs these cytotoxic responses, allowing unchecked proliferation and transformation of EBV-infected B cells, which can progress to PTLD [12-16]. EBV drives B-cell proliferation through the expression of latent viral antigens that mimic normal B-cell activation and survival signals, further promoting lymphomagenesis [2,7].
Impact of Immunosuppressive Therapy
The intensity and duration of immunosuppression are major determinants of PTLD risk. Agents such as calcineurin inhibitors (tacrolimus, cyclosporine), anti-thymocyte globulin (ATG), OKT3, and newer agents like belatacept (especially in EBV-seronegative recipients) are associated with increased PTLD risk [16]. Induction therapy, particularly with T-cell depleting agents, is strongly linked to early PTLD, while cumulative immunosuppression over time contributes to late-onset disease [16]. Notably, mycophenolate mofetil, basiliximab, and daclizumab have not been associated with increased PTLD risk [16].
EBV Serostatus Mismatch
EBV seronegative recipients who receive organs from EBVseropositive donors are at markedly increased risk for primary EBV infection post-transplant, which is the most potent trigger for early EBV-positive PTLD [1,3,5,12,16]. The relative risk in this setting is estimated to be 10–75 times higher than in seropositive recipients [16]. This risk is particularly pronounced in pediatric populations, who are more likely to be EBV-nave prior to transplantation [4-15].
Pediatric Risk
Children are disproportionately affected by PTLD due to higher rates of EBV seronegativity at the time of transplantation and increased likelihood of primary EBV infection post-transplant [2-3,5-6,8,10]. Pediatric studies demonstrate that high levels of EBV DNAemia, older age at EBV DNAemia diagnosis, and higher tacrolimus levels prior to EBV infection are associated with increased PTLD risk [5-6]. The American Association for the Study of Liver Diseases and the American Society of Transplantation highlight the importance of EBV monitoring and early recognition in pediatric liver transplant recipients [12].
Other Viral and Environmental Cofactors
While EBV is the predominant viral driver, up to 50% of lateonset PTLD cases may be EBV-negative, with pathogenesis less well defined [16]. Hypotheses include prior (“hit-and-run”) EBV infection, persistent antigenic stimulation from the graft, infection with other viruses (e.g., cytomegalovirus, hepatitis C virus), and long-term immunosuppression. Underlying disorders such as primary sclerosing cholangitis, cystic fibrosis, and autoimmune hepatitis have been variably associated with increased PTLD risk [3,16]. Genetic factors, cytokine gene polymorphisms, HLA mismatches, and certain racial/ethnic backgrounds may also modulate risk, though evidence is less robust [16].
Classification and Histopathology of PTLD
The diagnosis and classification of post-transplant lymphoproliferative disorder (PTLD) is grounded in histopathological examination and immunophenotyping, with the World Health Organization (WHO) 2017 classification serving as the gold standard for categorization [1,5,17-18]. PTLD encompasses a heterogeneous spectrum of lymphoid proliferations, ranging from benign hyperplasias to aggressive lymphomas, most commonly of B-cell origin [1,5,17].
WHO Classification of PTLD
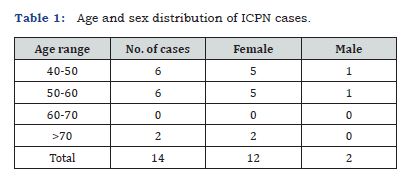
The WHO recognizes four major categories of PTLD, each with distinct histopathological and clinical features. Table 1 summarizes the classification of PTLD subtypes suggested by the World Health Organization (WHO).
• Non-destructive (Early) Lesions: Includes plasmacytic hyperplasia, infectious mononucleosis-like PTLD, and florid follicular hyperplasia. These lesions preserve underlying tissue architecture and are almost universally associated with EBV. They are typically polyclonal or oligoclonal and show a mixture of plasma cells, small lymphocytes, and immunoblasts [1,5,18-21].
• Polymorphic PTLD: Characterized by effacement of tissue architecture and a complete spectrum of B-cell maturation. These lesions are often EBV-positive (>90%), show variable clonality, and contain a mixture of B and T cells. They do not fulfill criteria for any specific lymphoma subtype [1,5,18-21].
• Monomorphic PTLD: Represents overt lymphomas that fulfill criteria for specific non-Hodgkin lymphoma (NHL) entities, most commonly diffuse large B-cell lymphoma (DLBCL), but also Burkitt lymphoma, plasma cell myeloma, and rarely T- or NKcell lymphomas. Monomorphic PTLD may be EBV-positive or negative and is always monoclonal. Histologically, monomorphic PTLD cannot be distinguished from their counterparts in immunocompetent patients, but EBV-positive cases are usually of non-germinal center B-cell type, while EBV-negative cases more often show germinal center phenotype [1,5,18-20-24].
• Classical Hodgkin Lymphoma-type PTLD: Rare, destructive lesions that fulfill criteria for classic Hodgkin lymphoma, typically EBV-positive (>90%), and show characteristic Reed-Sternberg cells with CD30+, CD15+, and CD20- immunophenotype [1,5,18- 21].
Histological Features and Immunophenotyping
Histopathological examination remains the cornerstone of PTLD diagnosis. Non-destructive lesions show preserved architecture and a polymorphic infiltrate, while polymorphic and monomorphic PTLDs demonstrate architectural effacement and destructive growth [1,5,18,21]. Immunophenotyping is essential for subclassification, with most monomorphic PTLDs expressing pan-B-cell markers (CD20, CD79a), and further subclassification based on germinal center (CD10, BCL6) versus non-germinal center (MUM1, CD138) markers [1,22-23].
T-cell and NK-cell PTLDs are rare and are classified according to lineage-specific markers [18]. Monomorphic PTLDs, especially DLBCL, may be further characterized by gene expression profiling and molecular studies. EBV-positive cases tend to be genomically stable and of non-germinal center phenotype, while EBVnegative cases show more complex genomic alterations and are often germinal center type [1,22-23]. TP53 mutations are more frequent in EBV-negative monomorphic PTLD [23].
Epstein-Barr Virus (EBV) Status in Tissue
EBV status is a critical component of PTLD evaluation. EBVencoded RNA (EBER) in situ hybridization is recommended for all cases, as it is the most sensitive method for detecting latent EBV infection in tissue [1,5,19,24-26]. EBV association is nearly universal in non-destructive and polymorphic PTLD, and in most Hodgkin lymphoma-type PTLD, but only about half of monomorphic PTLDs are EBV-positive [1,5,18,19].
EBV status does not currently guide therapy in adults but may have implications for pathogenesis and risk stratification [1,25]. The classification and histopathology of PTLD are defined by the WHO system, integrating architectural, cytological, immunophenotypic, and molecular features, with EBV status determined by EBER in situ hybridization as a key diagnostic adjunct [1-26].
Clinical Presentation in Liver Transplant Recipients
The clinical presentation of post-transplant lymphoproliferative disorder (PTLD) after liver transplantation is heterogeneous, but recurring symptom clusters help orient early recognition. Fever is common yet nonspecific, and in the liver transplant population, it should prompt consideration of occult infection, rejection, or lymphoproliferation. Generalized or regional lymphadenopathy is another frequent early clue and may be misattributed to reactive processes if tissue diagnosis is delayed. Gastrointestinal (GI) symptoms are particularly prominent in liver recipients, ranging from abdominal pain, nausea, vomiting, and diarrhea to overt bleeding, perforation, obstruction, or masslike lesions detected on endoscopy or imaging when the GI tract is the primary extranodal site.
Graft dysfunction, elevated liver enzymes, cholestasis, or jaundice may herald direct graft infiltration by PTLD, but can overlap with acute cellular rejection, biliary complications, or opportunistic infections; clinical context and histology remain decisive. Collectively, these symptom constellations underscore the need for a low threshold to pursue tissue diagnosis in transplant recipients with persistent constitutional or GI complaints [6,27–30,32].
Organ involvement in liver transplant recipients with PTLD is broad, with the GI tract the most affected extranodal site, followed by the liver graft, lungs, and central nervous system (CNS). GI disease can present with ulcerations, polypoid masses, or circumferential thickening and may precipitate life-threatening complications such as hemorrhage or perforation. Graftinfiltrating PTLD can drive rapid deterioration in hepatic function and systemic inflammation. Pulmonary involvement is less frequent but clinically important, manifesting as cough, dyspnea, or radiographic nodules and consolidations that mimic infection.
CNS disease represents a severe phenotype with seizures, focal deficits, or encephalopathy, and often signals disseminated, aggressive biology. Multiorgan disease at diagnosis portends worse outcomes and usually reflects monomorphic or advanced PTLD subtypes [27-29,31-32]. Timing after transplantation is clinically informative. Early-onset PTLD classically within the first post-transplant year correlates with higher net immunosuppression and is frequently Epstein-Barr virus (EBV) positive, with a predilection for extranodal sites including the GI tract, the liver graft, and the CNS.
In contrast, late-onset PTLD, which emerges after the first year, more often presents indolently with nodal disease and exhibits a higher proportion of EBV-negative biology. Diagnostic delays are common because symptoms are subtle and clinical suspicion wanes over time. Contemporary series in liver transplantation report median times to diagnosis that cluster around 12–24 months overall, with earlier onset in pediatric recipients and later onset in adults, consistent with the early/late dichotomy and the EBV biology shift over time [5,6,8,29,30].
Important age-dependent differences exist. Pediatric liver recipients develop PTLD more often and earlier than adults, driven largely by primary EBV infection in previously seronegative children who receive EBV-positive grafts; they also show a higher frequency of extranodal disease, especially GI tract and graft involvement, and can present with severe or catastrophic GI complications. Adults, by contrast, exhibit a relatively higher share of late-onset and nodal presentations, more variable symptomatology, and a larger proportion of EBV-negative disease years after transplantation. Large liver-transplant cohorts confirm higher PTLD incidence and earlier onset in children but poorer post-diagnosis survival in adults, highlighting distinct surveillance and management needs across age groups [5,6,31,33].
Diagnostic Evaluation
The diagnostic workup for PTLD after liver transplantation is multidisciplinary and should be coordinated by the transplant center. Initial assessment includes a thorough physical examination, with attention to lymphadenopathy, adenotonsillar hypertrophy, and organomegaly [37]. Laboratory evaluation should include quantitative EBV viral load measurement by PCR in peripheral blood, as EBV DNAemia is a sensitive marker for EBV-positive PTLD and is recommended for screening and risk stratification, especially in high-risk populations [10,35,37]. However, EBV PCR may miss EBV-negative PTLD and some localized or donor-derived cases [11,37].
>Imaging studies are essential for staging and disease localization. Whole-body CT (head to pelvis) is standard, with PET-CT providing additional sensitivity for metabolically active lesions and occult disease [36-37]. MRI is preferred for CNS involvement due to superior lesion delineation and reduced radiation exposure [9]. Bone marrow biopsy and lumbar puncture for CSF analysis should be considered if there is clinical suspicion for marrow or CNS involvement [37]. Histopathological examination of affected tissue remains the gold standard for PTLD diagnosis, with immunohistochemistry and in situ hybridization for EBV-encoded RNA (EBER) to confirm EBV status [13,37]. Liquid biopsy approaches, including cell-free plasma EBV DNA, are emerging as adjuncts for diagnosis and monitoring, with some evidence suggesting improved sensitivity for EBV-positive disease compared to cellular PCR [11].
Management Strategies
Management of PTLD is risk-adapted and sequential, beginning with reduction of immunosuppression (RIS) and escalating to targeted immunotherapy and chemotherapy as indicated [2,8,10,11,13,34,38].
Reduction of Immunosuppression (RI)
RIS is the cornerstone of initial PTLD management, aiming to restore EBV-specific cellular immunity while minimizing risk of graft rejection [11]. This typically involves reducing calcineurin inhibitor doses (cyclosporine or tacrolimus) by at least 50% and discontinuing antimetabolites (azathioprine or mycophenolate mofetil). RIS alone leads to regression in 20–80% of cases, with higher response rates in nondestructive and EBV-positive PTLD [2,11]. Close monitoring for allograft rejection is essential, and RIS may be less effective in EBV-negative, bulky, or advanced-stage disease [11].
Rituximab Monotherapy
For CD20-positive PTLD not responding to RIS, rituximab (anti-CD20 monoclonal antibody) is recommended as first-line therapy [1-2,5-6,8,10,12]. Rituximab monotherapy is effective in nondestructive, polymorphic, and monomorphic DLBCL PTLD, with favorable toxicity and improved performance status prior to chemotherapy [2,8,10,11,13,34,38]. Subcutaneous and intravenous formulations are used, with dosing typically 375 mg/ m² weekly for 4 doses, though regimens may vary [38]. Response rates are highest in EBV-positive and low-risk disease [38].
Combination Chemoimmunotherapy
Patients with high-risk features (bulky disease, advanced stage, poor response to RIS/rituximab) or monomorphic PTLD require combination chemoimmunotherapy, most commonly R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) or modified regimens [2,8,10,11,13,34-38]. Sequential risk-stratified approaches, as validated in PTLD-1 and PTLD-2 trials, reserve chemotherapy for those not achieving remission with rituximab alone. Treatment-related morbidity and mortality have decreased with modern regimens, but infection risk remains significant [10,11,34-38].
Adoptive Immunotherapy and Emerging Approaches
For relapsed or refractory PTLD, adoptive immunotherapy with EBV-specific cytotoxic T lymphocytes (CTLs) is a promising option, particularly in EBV-positive disease [8,10,11,34-38]. CTLs restore EBV-specific immunity with low toxicity and no risk of graft-versus-host disease, but are limited by cost, availability, and time to manufacture [10,11,34]. Other emerging therapies include immune checkpoint inhibitors and cellular therapies (e.g., CAR T-cells), though their use in PTLD is investigational and associated with unique risks in the immunosuppressed population [34]. Antiviral therapy is not effective as monotherapy but may have a role in combination with agents that induce viral thymidine kinase [11]. Management should be individualized based on PTLD subtype, EBV status, disease burden, and patient comorbidities, with multidisciplinary input from transplant, infectious diseases, and hematology/oncology teams.
Prognosis and Outcomes
The prognosis for PTLD after liver transplantation varies considerably but has generally improved over time. Overall survival rates show one-, three- and five-year survival of 81%, 74% and 60%, respectively [11]. However, survival rates vary across different studies, with some reporting overall survival at 1 year and 5 years of 78% and 64%, respectively [32]. The median survival time is approximately 37 months [11], though this varies significantly based on multiple prognostic factors. Approximately half of EBV+ PTLD cases do not respond to initial treatment or relapses, resulting in a poor prognosis [33], indicating substantial treatment challenges in certain subgroups.
EBV status emerges as one of the most critical prognostic factors. EBV-negative patients had better mean survival (95±79 months) [11] compared to EBV-positive patients. EBV status was the most important characteristic influencing likelihood of response to rituximab [34]. The timing of PTLD development also correlates with EBV status: during the first 4 years following liver transplantation, PTLD were predominantly related to EBV, while afterward most PTLD were EBV negative [5]. Type of PTLD (monomorphic type) is identified as a significant prognostic factor, with monomorphic PTLD having greater mortality.
Late-onset PTLD tends to be monoclonal, EBV-negative, and often more refractory to therapy [32]. Rituximab was associated with increased survival and should be considered as first-line therapy for PTLD patients [9]. However, response varies by patient characteristics, with poor response to rituximab noted in patients with age ≥ 30 years, extra-lymphoid tissue involvement, acute GVHD, and a lack of reduction in immunosuppressive therapy upon PTLD diagnosis. Additional important prognostic factors include age at diagnosis ≥ 18 years and poor clinical status (performance score > 2) at diagnosis [37,38].
Long-term outcomes show considerable variability. The 5-year survival is ~35% according to some studies, though this appears to be an overall figure that may not specifically reflect liver transplant recipients. Disease regression in response to a reduction in immunosuppression is a unique diagnostic feature of PTLD, but patients require close monitoring for allograft rejection during this process [10]. The management approach significantly impacts quality of life, as treatment often requires careful balancing of immunosuppression reduction with the risk of graft rejection, creating ongoing medical complexity for survivors.
There are no table differences in outcomes between adult and pediatric liver transplant recipients with PTLD. The overall survival rate at three, five and ten-years in the pediatric group was 81%, 79%, and 71%; compared to the adult group with 61%, 38%, and 28%; respectively, demonstrating significantly better outcomes in pediatric patients. Pediatric patients also show different treatment responses. In a Children’s Oncology Group study of low-dose chemotherapy with rituximab, the 2-year event-free survival was 71% and overall survival was 83% with median follow-up of 4.8 years [11]. The timing of onset also differs, with early onset PTLD patients showing one- and five-year survival rates of 64% and 54%, respectively, compared to 73% and 50% for the control group, though these differences were not statistically significant [33-38].
Conclusion
Post-transplant lymphoproliferative disorder remains a significant and complex challenge following liver transplantation. Its pathogenesis is deeply rooted in the interplay between immunosuppression and EBV infection, particularly in high-risk pediatric populations. As our understanding of the disease has evolved, so have diagnostic and management strategies, moving towards a risk-stratified, sequential approach. The cornerstone of management involves reducing immunosuppression, with rituximab monotherapy providing effective control for most cases.
However, the variable presentation, from non-destructive lesions to aggressive monomorphic lymphomas, necessitates a personalized approach, often requiring intensive chemoimmunotherapy or novel adoptive immunotherapies for refractory disease. Despite significant advancements in treatment, PTLD continues to carry a high mortality rate, particularly in adults and those with EBV-negative or monomorphic subtypes. Future research must focus on optimizing risk stratification, validating emerging therapies, and establishing tailored surveillance protocols to further improve outcomes and long-term quality of life for liver transplant recipients.
References
- Dierickx D, Habermann TM (2018) Post-Transplantation Lymphoproliferative Disorders in Adults. N Engl J Med 378(6): 549-562.
- Amengual JE, Pro B (2023) How I Treat Posttransplant Lymphoproliferative Disorder. Blood 142(17): 1426-1437.
- Bastian N Ruijter, Maarten E Tushuizen, Danny van der Helm, Mitchel Hew, Marjolein Reeven, et al. (2024) Primary Sclerosing Cholangitis and Other Risk Factors for Post-Transplant Lymphoproliferative Disease After Liver Transplantation in Adults. Liver Transpl 30(6): 640-646.
- Erin Y Chen, Natasha Dilwali, Krupa R Mysore, Sara Hassan, Sara Kathryn Smith, et al. (2025) Navigating Epstein-Barr Virus (EBV) and Post-Transplant Lymphoproliferative Disorder (PTLD) in Pediatric Liver Transplantation: Current Knowledge and Strategies for Treatment and Surveillance. Viruses 17(2): 254.
- Allen UD, Preiksaitis JK (2019) Post-Transplant Lymphoproliferative Disorders, Epstein-Barr Virus Infection, and Disease in Solid Organ Transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant 33(9): e13652.
- Tetsuya Tajima, Koichiro Hata, Hironori Haga, Momoko Nishikori, Katsutsugu Umeda, et al. (2021) Post-Transplant Lymphoproliferative Disorders After Liver Transplantation: A Retrospective Cohort Study Including 1954 Transplants. Liver Transpl 27(8): 1165-1180.
- Zaffiri L, Chambers ET (2023) Screening and Management of PTLD. Transplantation 107(11): 2316-2328.
- Barut Dogan, Yildirim Arslan Sema, Kunay Bora, Umman Veysel, Dernek Benan, et al. (2024) Post-Transplant Lymphoproliferative Disorder Associated Epstein-Barr Virus DNAemia After Liver Transplantation in Children: Experience from Single Center. J Med Virol 96(6): e29767.
- Vikas R Dharnidharka, Angela C Webster, Olivia M Martinez, Jutta K Preiksaitis, Veronique Leblond, et al. (2016) Post-Transplant Lymphoproliferative Disorders. Nat Rev Dis Primers 2: 15088.
- Ying Liu, Li-Ying Sun, Zhi-Jun Zhu, Lin Wei, Wei Qu, et al. (2021) Post-Transplant Lymphoproliferative Disorder After Paediatric Liver Transplantation. Int J Clin Pract 75(4): e13843.
- Regina Cheuk-lam Lo, See-ching Chan, Kwong-leung Chan, Alan Kwok-shing Chiang, Chung-mau Lo, et al. (2013) Post-Transplant Lymphoproliferative Disorders in Liver Transplant Recipients: A Clinicopathological Study. J Clin Pathol 66(5): 392-398.
- Deirdre A Kelly, John C Bucuvalas, Estella M Alonso, Saul J Karpen, Upton Allen, et al. (2013) Long-Term Medical Management of the Pediatric Patient After Liver Transplantation: 2013 Practice Guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transpl 19(8): 798-825.
- Yeh-Chung Chang, Rebecca R Young, Alisha M Mavis, Eileen T Chambers, Sonya Kirmani, et al. (2022) Epstein-Barr Virus DNAemia and Post-Transplant Lymphoproliferative Disorder in Pediatric Solid Organ Transplant Recipients. PLoS One 17(10): e0269766.
- Martinez OM, Krams SM (2017) The Immune Response to Epstein Barr Virus and Implications for Posttransplant Lymphoproliferative Disorder. Transplantation 101(9): 2009-2016.
- Green M, Michaels MG (2013) Epstein-Barr Virus Infection and Posttransplant Lymphoproliferative Disorder. Am J Transplant 13(Suppl 3): 41-54.
- Furlano PL, Böhmig GA, Puchhammer-Stöckl E, Vietzen H (2024) Mechanistic Understanding of EBV+Lymphoproliferative Disease Development After Transplantation. Transplantation 108(9): 1867-1881.
- El-Mallawany NK, Rouce RH (2024) EBV and Post-Transplant Lymphoproliferative Disorder: A Complex Relationship. Hematology Am Soc Hematol Educ Program 2024(1): 728-735.
- Leticia Quintanilla-Martinez, Steven H Swerdlow, Thomas Tousseyn, Carlos Barrionuevo, Shigeo Nakamura, et al. (2023) New Concepts in EBV-associated B, T, and NK Cell Lymphoproliferative Disorders. Virchows Arch 482(1): 227-244.
- Humar A, Michaels M (2006) American Society of Transplantation Recommendations for Screening, Monitoring and Reporting of Infectious Complications in Immunosuppression Trials in Recipients of Organ Transplantation. Am J Transplant 6(2): 262-274.
- Julia Salmerón-Villalobos, Natalia Castrejón-de-Anta, Pilar Guerra-García, Joan Enric Ramis-Zaldivar, Mónica López-Guerra, et al. (2003) Decoding the Molecular Heterogeneity of Pediatric Monomorphic Post-Solid Organ Transplant Lymphoproliferative Disorders. Blood 142(5): 434-445.
- Vanesa-Sindi Ivanova, Thomas Menter, Ningxuan Cui, Peter Leary, Carl Zinner, et al. (2025) Distinct Subtypes of Post-Transplant Lymphoproliferative Disorders: CHIP-like Mutations in Early Lesions and Substantial Mutational Differences Between EBV-positive and EBV-negative Diffuse Large B-Cell Lymphomas. Br J Haematol 206(2): 484-504.
- Marco Lucioni, Daniela Capello, Roberta Riboni, Giovanbattista Ippoliti, Carlo Campana, et al. (2006) B-Cell Posttransplant Lymphoproliferative Disorders in Heart and/or Lungs Recipients: Clinical and Molecular-Histogenetic Study of 17 Cases from a Single Institution. Transplantation 82(8): 1013-1023.
- Elizabeth L Courville, Sophia Yohe, David Chou, Valentina Nardi, Aleksandr Lazaryan, et al. (2016) EBV-negative Monomorphic B-Cell Post-Transplant Lymphoproliferative Disorders Are Pathologically Distinct From EBV-positive Cases and Frequently Contain TP53 Mutations. Mod Pathol 29(10): 1200-1211.
- Dierickx D, Pociupany M, Natkunam Y (2022) Epstein-Barr Virus-Associated Posttransplant Lymphoproliferative Disorders: New Insights in Pathogenesis, Classification and Treatment. Curr Opin Oncol 34(5): 413-421.
- Jwa Hoon Kim, Hyungwoo Cho, Heungsup Sung, Ah Ra Jung, Yoon Sei Lee, et al. (2021) Reappraisal of the Prognostic Value of Epstein-Barr Virus Status in Monomorphic Post-Transplantation Lymphoproliferative Disorders-Diffuse Large B-Cell Lymphoma. Sci Rep 11(1): 2880.
- Ryumei Kurashige, Masako Kurashige, Yosuke Okada, Kohei Higuchi, Sayako Yuda, et al. (2024) Differentiating Between Epstein-Barr Virus-Positive Lymphoid Neoplasm Relapse and Post-Transplant Lymphoproliferative Disorder After Sex-Mismatched Hematopoietic Stem Cell Transplantation. Am J Surg Pathol 48(4): 395-405.
- Jain A, Nalesnik M, Reyes J, et al. (2011) Post-transplant lymphoproliferative disease following liver transplantation. World J Gastroenterol 17(34): 4090-4101.
- Danziger-Isakov L, Kumar D, et al. (2022) Gastrointestinal manifestations, risk factors, and management in PTLD after solid organ transplantation. World J Gastroenterol 28(27): 3273-3291.
- Daan Dierickx, Nina Cardinaels (2015) Posttransplant lymphoproliferative disorders following liver transplantation. World J Gastroenterol 21(39): 11034-11043.
- Kim SJ, Pereira MR, et al. (2021) Current practices on diagnosis, prevention and treatment of PTLD in solid organ transplantation: A multi-center survey and case series. Transpl Infect Dis 23(4): e13602.
- Bhalala U, Ng VL, Arnon R, et al. (2025) Navigating Epstein-Barr virus and PTLD in pediatric liver transplantation: A comprehensive review. Children (Basel) p: 12.
- Chiao J, Chuang CH, Hu SY, et al. (2018) Post-transplantation lymphoproliferative disorder with isolated gastrointestinal involvement: literature review and case report. World J Gastroenterol 24(7): 826-834.
- Kebudi R, Yigit E, Gecim E, et al. (2023) Catastrophic gastrointestinal complications of post-transplant lymphoproliferative disorder in pediatric liver transplant recipients: A case series. J Med Case Rep 17: 398.
- Atallah-Yunes SA, Salman O, Robertson MJ (2023) Post-Transplant Lymphoproliferative Disorder: Update on Treatment and Novel Therapies. Br J Haematol 201(3): 383-395.
- Marco Lucioni, Daniela Capello, Roberta Riboni, Giovanbattista Ippoliti, Carlo Campana, Laura Bandiera, et al. (2006) B-Cell Posttransplant Lymphoproliferative Disorders in Heart and/or Lungs Recipients: Clinical and Molecular-Histogenetic Study of 17 Cases from a Single Institution. Transplantation 82(8): 1013-1023.
- Elizabeth L Courville, Sophia Yohe, David Chou, Valentina Nardi, Aleksandr Lazaryan, et al. (2016) EBV-negative Monomorphic B-Cell Post-Transplant Lymphoproliferative Disorders Are Pathologically Distinct From EBV-positive Cases and Frequently Contain TP53 Mutations. Mod Pathol 29(10): 1200-1211.
- Dierickx D, Pociupany M, Natkunam Y (2022) Epstein-Barr Virus-Associated Posttransplant Lymphoproliferative Disorders: New Insights in Pathogenesis, Classification and Treatment. Curr Opin Oncol 34(5): 413-421.
- Ryumei Kurashige, Masako Kurashige, Yosuke Okada, Kohei Higuchi, Sayako Yud, et al. (2024) Differentiating Between Epstein-Barr Virus-Positive Lymphoid Neoplasm Relapse and Post-Transplant Lymphoproliferative Disorder After Sex-Mismatched Hematopoietic Stem Cell Transplantation. Am J Surg Pathol 48(4): 395-405.






























