Abstract
Background: Metastatic spread of extragenital malignancies to the uterus is rare, with invasive lobular carcinoma (ILC) of the breast being the most common source. Unlike invasive ductal carcinoma, ILC demonstrates a unique metastatic pattern involving unusual sites such as the peritoneum, gastrointestinal tract, and female genital tract. Differentiating metastatic ILC from primary endometrial carcinoma can be challenging, certain therapies which induces endometrial changes.
Case Presentation: The current case is of a 53-year-old postmenopausal woman with abnormal uterine bleeding . Initial clinico-radiological evaluation was suggestive of endometrial pathology. Total abdominal hysterectomy with bilateral salpingo-oophorectomy revealed polypoid endometrial lesions which was infiltrating the myometrium. Histopathology demonstrated discohesive tumor cells with a lobular growth pattern. Immunohistochemistry findings were also supportive of metastatic lobular carcinoma of breast origin. Subsequent PET-CT identified a metabolically active lesion in the left breast with nodal and skeletal metastases. Breast biopsy confirmed invasive lobular carcinoma with low proliferative index.
Conclusion: This case highlights the importance of considering metastatic breast carcinoma in postmenopausal women with abnormal uterine bleeding, previous history of cancer. Accurate diagnosis requires careful clinicopathologic correlation and immunohistochemical profiling to avoid misclassification as primary endometrial malignancy. Early recognition of uterine metastasis is critical to prevent unnecessary surgical procedures and ensure timely systemic therapy.
Keywords:Invasive lobular carcinoma; Uterine metastasis; Abnormal uterine bleeding; Immunohistochemistry
Abbreviations: ILC: Invasive Lobular Carcinoma; SERM: Selective Estrogen Receptor Modulator; IDC: Invasive Ductal Carcinoma
Introduction
Metastatic involvement of the uterus from extragenital primary malignancies is a rare event, accounting for a small subset of secondary uterine tumors. Among these, breast carcinoma particularly the invasive lobular subtypes, the most frequently reported source of metastases to the uterus. Invasive lobular carcinoma (ILC) exhibits a unique metastatic pattern compared to the more common invasive ductal carcinoma, often involving unusual sites such as the peritoneum, gastrointestinal tract, retroperitoneum, and gynecologic organs including the uterus.
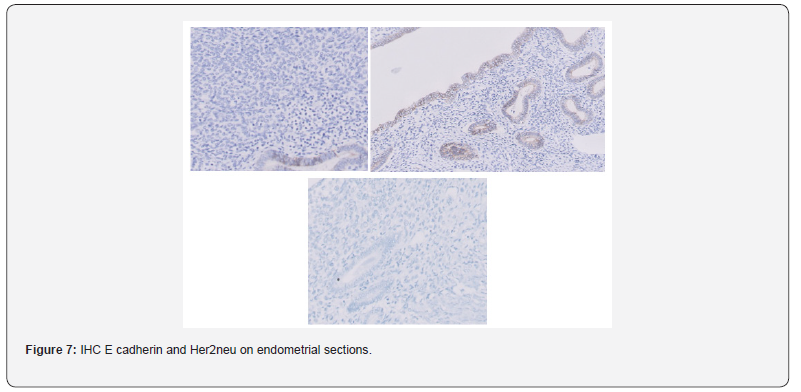
The tendency of ILC to metastasize to the female genital tract may be linked to the tumor’s characteristic loss of E-cadherin expression, resulting in discohesive tumor cells that more readily infiltrate stromal tissues. Within the uterus, the myometrium is more commonly involved than the endometrium; however, when endometrial involvement occurs, it may present with abnormal uterine bleeding, particularly in postmenopausal women. In certain Cases, a selective estrogen receptor modulator (SERM) widely used in hormone receptor-positive breast cancer, further complicates this clinical scenario. Excess estrogen can sometimes have an effect on the endometrium inducing hyperplasia, polyp formation, and even primary endometrial carcinoma.
These overlapping features can mask the presence of metastatic disease and delay definitive diagnosis. Recognition of uterine metastasis in patients with a history of ILC is crucial, particularly when symptoms such as abnormal vaginal bleeding emerge after long-term therapy. Diagnostic confirmation relies on histopathology, supported by immunohistochemical staining for markers like CK7, GATA3, and mammaglobin to establish breast origin. Herein, we report a rare case of metastatic invasive lobular carcinoma of the breast presenting as abnormal uterine bleeding, highlighting the diagnostic challenges and the need for heightened clinical suspicion in breast cancer survivors.
Case Presentation
A 53-year-old postmenopausal woman with a history of hypertension presented with complaints of abnormal uterine bleeding a year back. Clinical evaluation and imaging raised concern for endometrial pathology, prompting surgical intervention. She underwent a total abdominal hysterectomy with bilateral salpingo-oophorectomy four months later.
Gross examination: Total weight was 185gms, Total dimensions was 11 x 10 x 6cm, length of cervix was 3.5cm. Endometrium showed a gray, white irregular polypoidal mass, extending to the LUS and cervix (ranging from 0.3 to 0.5cm thickness). Bilateral adnexae were unremarkable. Myometrium showed a single subserosal leiomyoma measuring 2cm. No necrosis or haemorrhage was identified. Sections from the polypoidal mass were provided for discussion. Cut section showed a homogenous white whorled appearance.
Cervix: erosion, cervical wall showed a fibroid measuring 1.3cm. The right and left ovaries measured 1.5 × 1.5 × 1cm and 2 × 1.5 × 1cm, respectively, with congested external surfaces. Both fallopian tubes measured 3 cm in length, with normal caliber on cut section. Bilateral parametrial tissues were unremarkable.
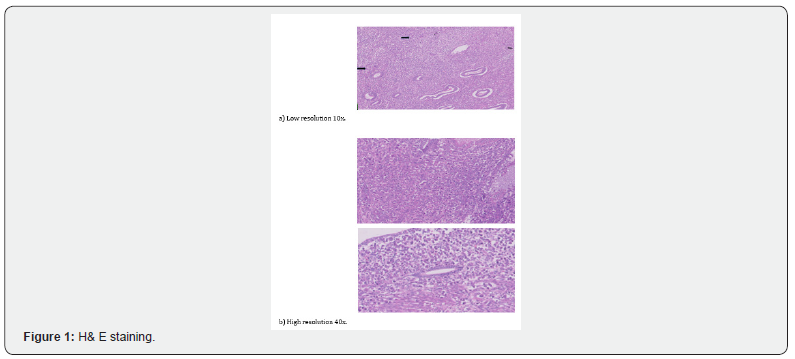
Microscopy examination: The endometrium showed polypoid projections of glandular pattern with benign glands and stroma with larger round to polygonal dyscohesive atypical cells with pleomorphic hyperchromatic vesicular nuclei and prominent nucleoli. At places a signet ring cell morphology was also noted.
These cells were present as sheets, at places in cords or also singly scattered in the endometrial stroma, just below and admixed with the endometrial glands. Mitotic rate was >2/10 HPF in such areas showing adenomyosis like pattern of invasion in less than half of the thickness of the myometrium.
This lesion was also seen extending to the cervix. Based on the findings, a diagnosis of Mullerian (Low grade) Adenosarcoma - Endometrium, cervix was made.
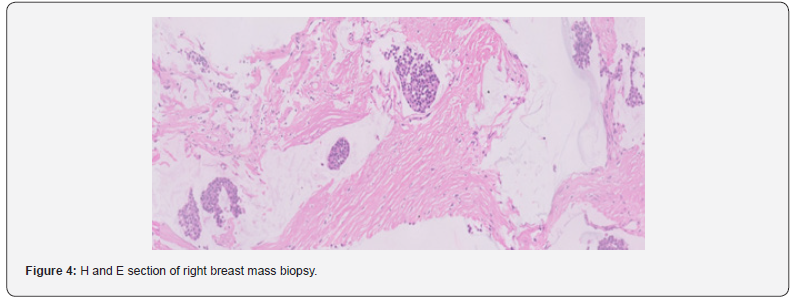
Imaging studies: Subsequent whole-body PET-CT demonstrated a metabolically active lesion in the right breast along with nodal and skeletal metastases, suggestive of disseminated malignancy. Also noted was an irregular intensity lesion in the left breast, which was also FDG avid consequently a right breast mass biopsy was performed.
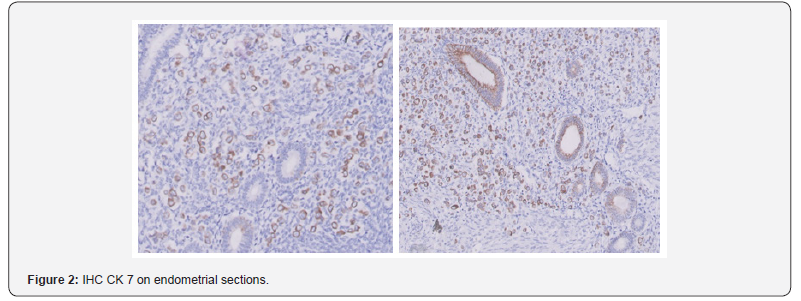
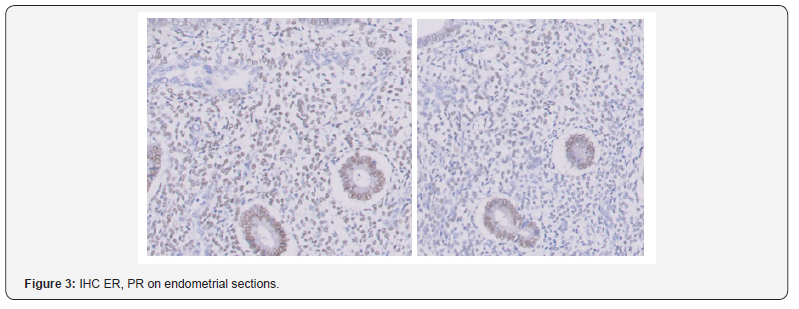
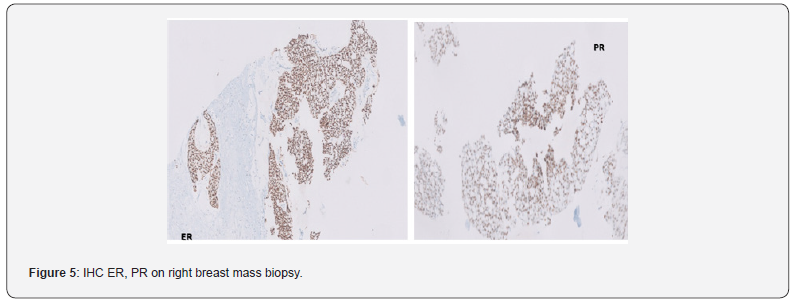
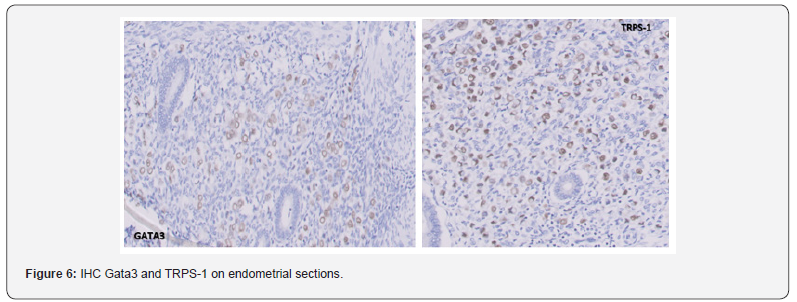
Breast biopsy & immunohistochemistry : A core needle biopsy of the right breast mass revealed Grade I mucinous carcinoma of the breast. Immunohistochemistry showed the tumor to be estrogen receptor (ER) positive (Allred score 5+3=8/8), progesterone receptor (PR) positive (Allred score 5+2= 7/8), Her2neu negative with a Ki-67 proliferation index of 10–12%. Immunohistochemistry examination on the endometrial sections was positive for PAN CK and Vimentin, while negative for SMA, Desmin, Pax8, WT1, CD10, Synaptophysin and Cyclin D1 (Not overexpressed). After the knowledge of the breast mass, additional IHC markers were performed, which showed positivity for GATA 3 and CK 7, while Ki-67 index was found to be 24 to 26% with E-cadherin being lost in the tumor cells.
Diagnosis: The uterine corpus and cervix were involved by an Invasive carcinoma with dyscohesive tumour cells. The tumour cells expressed PanCK, CK7, GATA3, ER and PR. They were negative for Pax8, Vimentin, Her2/neu (Score 0), WT1, SMA and Desmin. E cadherin were also lost in the tumour cells , while Ki67 is 24 to 26%. This can be best considered as a Metastatic Breast carcinoma with a lobular immunophenotype(in view of an irregular left breast mass on radiology and immunophenotype). This could potentially be the metastasis of the occult lobular carcinoma from the left breast FDG avid irregular mass. A biopsy was advised, but the patient refused. A monomorphic undifferentiated carcinoma of the endometrium raised suspicion for an aggressive or secondary malignancy. In the postoperative period, imaging performed for surveillance had incidentally detected a right breast lump along with an irregular density, ill defined lesion in the left breast (Figures 1-7).
Discussion
The female genital tract is not frequently involved by metastatic tumors. When it is, the ovaries are most often affected [1,2]. Tumors that secondarily involve the uterus usually do so by direct extension from adjacent pelvic organs or as a result of widespread peritoneal implants from ovarian carcinomas. Embolic metastases to the uterine corpus are distinctly unusual, especially from cancers originating in extragenital sites [3]. Abnormal/ Dsyfunctional uterine bleeding is the most classical initial manifestation of primary and/or secondary endometrial neoplasia. Breast cancer is the most common extra-gynecologic secondary source of endometrial neoplasia by being the main primary site that metastasizes to the uterus, especially lobular type [4,5]. Invasive lobular carcinoma (ILC), also known as infiltrative lobular carcinoma, is the second most common invasive breast cancer, after invasive ductal carcinoma (IDC).
ILC more frequently manifests with multifocal, multicentric, contralateral breast, and distant metastatic disease than does IDC. The distant metastatic pattern of ILC also differs significantly from that of IDC. Some investigators have suggested that, compared with IDC, ILC has a higher distant metastasis rate likely because of its infiltrative nature [6]. While both types have similar rates of liver metastasis, ILC more commonly metastasizes to the gastrointestinal tract, genitourinary tract, retroperitoneum, and peritoneum than does IDC [7]. Approximately 3–10% of breast cancer patients have metastatic disease at their initial diagnosis; recurrent disease or metastasis occurs in approximately 30% of patients during follow-up after initial treatment [7].
Mazur et al. [2] studied the anatomic localization of metastases in the uterine corpus and concluded that involvement of the endometrium itself accounted for 3.8% of the cases, both myometrium and endometrium 32.7%, and myometrium only 63.5% [2]. Of the cases limited to the endometrium, ILC is the most predominant histologic type, and given the site, these tumors are more likely to present with abnormal uterine bleeding than those arising in the myometrium only. It has been postulated that in ILC loss of E-cadherin, the cell-to-cell adhesion molecule, facilitates the metastasis process [8].
Like ILC in the breast, metastatic ILC tends to infiltrate the affected organs in a diffuse process instead of forming a discrete tumor nodule [9]. The overlapping morphologic features of the background endometrial stromal cells with the single cell and sheet-like proliferation of the metastatic tumor cells was a major diagnostic challenge in our case, especially that both cell types are likely to demonstrate positivity for hormone receptors. However, the positivity for breast origin sensitive markers like GATA3 and TRPS-1, in the tumor cells, along with the clinical backdrop, helped in reaching the correct diagnosis.
Conclusion
Uterine metastasis from extragenital malignancies is rare, with invasive lobular carcinoma (ILC) of the breast being the most common source. ILC is known for its diffuse infiltrative pattern and propensity to metastasize to unusual sites, including the female genital tract. This case underscores the diagnostic challenge when metastatic ILC involves the endometrium and mimics primary uterine pathology. In this patient, abnormal uterine bleeding and imaging findings initially suggested a primary endometrial lesion. Histopathology revealed discohesive tumor cells, and immunohistochemistry confirmed breast origin with markers such as ER, PR, CK7, and GATA3.
This report highlights the need for a high index of suspicion in breast cancer survivors presenting with gynecologic symptoms, particularly postmenopausal bleeding. Accurate diagnosis relies on a combination of clinical history, imaging, pathology, and immunohistochemistry. Recognizing metastatic disease early is crucial to avoid unnecessary surgical interventions and to direct appropriate systemic therapy. As breast cancer survival rate increases, awareness of such atypical metastatic presentations is essential for timely and effective patient management.
References
- Piura B, Yanai-Inbar I, Rabinovich A, Zalmanov S, Goldstein J (1999) Abnormal uterine bleeding as a presenting sign of metastases to the uterine corpus, cervix and vagina in a breast cancer patient on tamoxifen therapy. Eur J Obstet Gynecol Reprod Biol 83(1): 57-61.
- Mazur MT, Hsueh S, Gersell DJ (1984) Metastases to the female genital tract: analysis of 325 cases. Cancer 53(9): 1978-1984.
- Young RH, Scully RE (1986) Metastatic tumors of the uterine corpus: a clinicopathologic study of 63 cases. Cancer 58(9): 2163-2169.
- Bertucci F, Groulet A, Pierga JY, et al. (2015) Invasive lobular breast cancer: distinct molecular entity with specific clinical management. Breast Cancer Res 17: 21.
- S Ferlicot, A Vincent-Salomon, J Médioni, P Genin, C Rosty, B Sigal-Zafrani, et al. (2004) Wide metastatic spreading in infiltrating lobular carcinoma of the breast. Eur J Cancer 40(3): 336-341.
- Lamovec J, Bracko M (1991) Metastatic pattern of infiltrating lobular carcinoma of the breast: an autopsy study. J Surg Oncol 48(1): 28-33.
- Hagen Kennecke, Rinat Yerushalmi, Ryan Woods, Maggie Chon U Cheang, David Voduc, et al. (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28(20): 3271-3277.
- Berx G, Van Roy F (2001) The E-cadherin/catenin complex: an important gatekeeper in breast cancer tumorigenesis and malignant progression. Breast Cancer Res 3(5): 289-293.
- So Hyeon Yang, Jae Seok Lee, Ji Won Koh, Ilias P Nikas, Eun Na Kim, et al. (2017) The diagnostic utility of GATA3 and TRPS1 in metastatic breast carcinoma. Histopathology 70(4): 657-665.






























