Abstract
Gallbladder cancer is a leading malignancy in Northeast India, with a particularly high incidence among women. Among the precursor lesions recognized in the 5th edition of the WHO classification of digestive system tumors, Intracholecystic Papillary Neoplasm (ICPN) is a recently defined and relatively rare entity. This prospective study, conducted at Ekopath Metropolis Lab, Guwahati, over a period of 16 months from January 2023 to April 2024, aimed to explore the pathological spectrum of ICPN and its association with invasive carcinoma. Out of 6663 cholecystectomy specimens examined, 102 showed neoplastic pathology, including 14 cases of ICPN. The majority of ICPN cases occurred in females, with a mean age of 52 years.
Most ICPNs exhibited intestinal histological subtypes, followed by a mixed intestinal and biliary pattern. Notably, 71.4% (10 out of 14) of the ICPN cases had an associated invasive adenocarcinoma, all of which showed high-grade dysplasia. The most frequent stages of invasive components were pT1b and pT2. This study observed a higher incidence of ICPN-associated invasive carcinoma compared to previously published literature. The findings underscore the diagnostic significance of ICPN and highlight its potential for malignant transformation. Recognizing and reporting such precursor lesions is crucial for early diagnosis and better clinical management of gallbladder neoplasia.
Keywords:Gall bladder; Neoplasm; ICPN (Intracholecystic Papillary Neoplasm)
Abbreviations: WHO: World Health Organization, GB: Gall bladder, PGA: Pyloric Gland Adenoma; iIIN: Biliary Intraepithelial Neoplasia; IPN: Intraductal Papillary Neoplasm of the Bile Duct; IPMNs: Intraductal Papillary Mucinous Neoplasms; ITPNs: Intraductal Tubulopapillary Neoplasms in the Pancreas
Introduction
Gall bladder cancer is one of the most common cancers in northeastern region of India predominantly affecting females [1]. The incidence of gallbladder cancer shows marked geographic and ethnic variations with moderate to high incidence in India, East Asian countries and some central and eastern European countries with highest incidence reported in the indigenous Mapuche people of Chile [2]. The age standardized rate for GB carcinoma is 17.1/100,000 population in women of northeast India [1] which is like the high incidence areas such as Chile and Bolivia [2]. Gall bladder adenocarcinoma has dismal prognosis [3] and thereby clinicopathological and molecular research to understand the pathogenesis and carcinogenesis is extremely essential. Fifth edition of WHO classification of the digestive system has introduced 3 benign epithelial tumors and precursor lesions of gall bladder: pyloric gland adenoma (PGA), Biliary Intraepithelial neoplasia (BilIN) and Intracholecystic papillary neoplasm (ICPN) [4].
ICPN is a new and relatively rare entity which has been introduced in 5th Edition and is characterized as a grossly visible mass forming non-invasive epithelial neoplasm arising from mucosa of gall bladder projecting into the lumen. ICPNs are found in 0.4% of cholecystectomies [5]. The rarity of ICPN and the difficulties associated with detecting it can be explained by relatively ambiguous diagnostic criterias, incidental nature of diagnosis, non-specific symptoms, and difficulty of radiological investigations to distinguish between a gall bladder stone and a tumour.
ICPNs are classified as low grade and high grade based on the highest cytoarchitectural atypia in the epithelium. ICPN may have invasive carcinoma components and in such cases, they are termed as ICPN with associated invasive carcinoma [4]. ICPN with no associated invasive component has a good prognosis. Adenocarcinoma of gall bladder is known to have miserable prognosis but ICPN with invasion has comparatively better prognosis compared to the conventional gall bladder carcinomas [4]. Four subAbstract types of ICPN have been described in WHO (2019) with biliary being the most common phenotype followed by gastric, intestinal and oncocytic being the least common.
Aim
This study aims to investigate the pathological characteristics of ICPN based on 5th Edition of WHO classification of tumours of the digestive system (2019).
Materials and Method
This is a prospective study of 1 year and 4 months duration. All the cholecystectomy cases were examined from January 2023 to April 2024. A total number of 6663 gall bladder biopsies were examined. Cases were examined by 2 pathologists, and the findings of gross examination and microscopic examination were correlated to avoid interobserver variation in diagnosis. They were analyzed for distribution of age, sex, invasiveness, histological differentiation and grade of dysplasia.
Inclusion Criteria
Gall bladder cases with the diagnosis of pyloric gland adenoma, Biliary intraepithelial neoplasia, ICPN and gall bladder malignancy were included in our study.
Exclusions from this Study
All benign inflammatory conditions of gall bladder, including reactive atypia associated with Acute Cholecystitis were excluded from this study.
Results and Observations
102 cases were found to have neoplastic pathology out of 6663 cases of gall bladder biopsies. Of the 102 cases, 20(19.6%) cases were pyloric gland adenoma, 27 (26.5%) cases had isolated BilIN, 14 (13.7%) cases were ICPN and 41 (40.2%) cases had invasive gall bladder malignancy. Of the 14 ICPN cases, 10 cases had associated invasive adenocarcinoma (Figure 1).

Pyloric gland adenoma
20 cases out 102 neoplastic GB cases were pyloric gland adenoma. 2 out of 20 cases had associated low grade dysplasia. None of the cases had associated high grade dysplasia or invasive malignancy.
Biliary Intraepithelial Neoplasia
Biliary Intraepithelial Neoplasia (BilIN) is a flat microscopic or micropapillary lesion without invasion [4]. Previously BilIN was classified into 3 types, now WHO 5th Edition has classified BilIN in two-tiered system with low- and high-grade dysplasia. The former low and intermediate grade dysplasia is now classified as low grade. In our study, 21 cases had isolated low grade BilIN and 6 cases had isolated high grade BilIN.
Intracholecystic Papillary Neoplasm: 14 cases were ICPN in our study out of 102 neoplastic GB cases
Age and Sex Distribution of ICPN
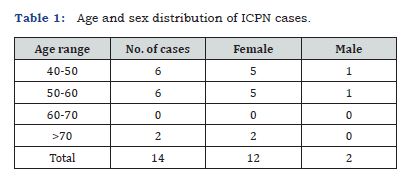
ICPN cases had the age range of 40-73 years with a mean age of 52 years. In our study, they are 5.5 times more common in females than male (Table 1).
Macroscopic Findings of ICPN
ICPNs were seen as exophytic growth or as granular, friable excrescences within the gall bladder [4]. In few of our cases the friable excrescences were loosely attached to the wall and may be mistaken as sludge or debris in the lumen. The size range of ICPN in our study was from 0.5 to 6cm (Figure 2).

Histological Types of ICPN
Four histological types have been described in WHO i.e. biliary, gastric, intestinal and oncocytic. ICPNs may have more than one histological type in the same tumour. When the tumour contains considerable areas of 2 or more subtypes, it was classified as mixed subtype [6-9]. In our study, out of 14 ICPN cases, 9 cases were of intestinal subtype and rest of 5 cases showed mixed subtype comprising of intestinal and biliary differentiation. Intestinal type shows presence of tall columnar cells with stratified elongated cigar shaped nuclei and resembles intestinal adenomas. Biliary type shows cuboidal to low columnar, non-mucinous cells. Gastric type and oncocytic type (least common) were not seen in our study.
Grades of Dysplasia in ICPN

Dysplasia in ICPNs were graded by two-tiered grading system – low grade and high-grade dysplasia. All the cases in our study showed presence of high-grade dysplasia except for 1 case which had only low-grade dysplasia. Few of the cases showed presence of both low grade and high-grade dysplasia. All the 10 cases of ICPNs that were associated with adenocarcinoma showed presence of high-grade dysplasia (Figure 3).
Associated Carcinoma and Stages of the Tumour seen in ICPN:
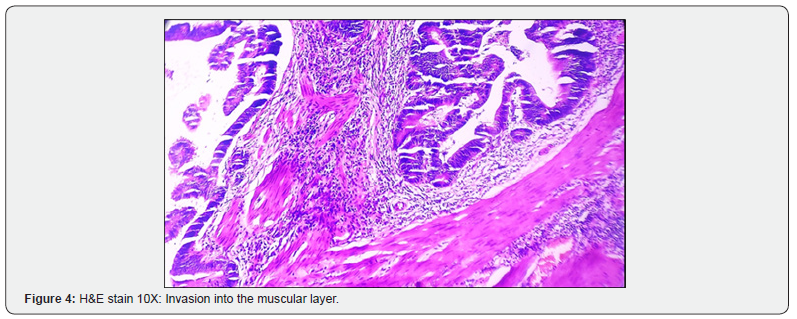
Out of 14 cases, 4 were non-invasive and 10 (71.4%) cases showed presence of associated adenocarcinoma of GB. 5 out of 10 cases were of stage pT1b, 4 cases were of stage pT2 and 1 case was of stage pT3 (Table 2) (Figure 4).

Invasive carcinoma of Gall bladder
Gall bladder malignancies were seen in 51 (50%) cases out of 102 neoplastic GB cases. Of the 51 cases, 10 cases were associated with ICPN and high-grade dysplasia. Rest of the 41 cases were adenocarcinoma of gall bladder with 3 of the cases being Mucinous adenocarcinoma.
Discussion
In the fourth edition of WHO’s tumor classification of the digestive system (2010), tubular adenoma of intestinal type, papillary adenoma of biliary type, and tubular adenoma of pyloric gland type (PGA) were grouped into one “adenoma” category [10]. On the contrary, in the WHO 2019 edition, adenomas other than PGA were grouped under the ICPN category, and only PGA was independently classified as one of the three precursor neoplastic lesions of the gallbladder [4]. Gallbladder PGAs show some histological similarities with PGAs of other organs, especially the stomach, duodenum, and pancreas. However, molecular abnormalities are quite different between PGAs in the gallbladder and in other areas. Gallbladder PGAs frequently have the CTNNB1 mutation and only rarely have the KRAS mutation, and they lack the GNAS mutation.
On the contrary, PGAs of the stomach, duodenum, and pancreas frequently have KRAS and GNAS mutations [11]. In 2012, Adsay et al. [5] first proposed the term ICPN (Intracholecystic papillary tubular neoplasm) and defined it as mass-forming (≥1cm) preinvasive neoplasms of the GB that share common features and exhibit many similarities to biliary IPNs and pancreatic IPMNs and ITPNs. They also stated that ICPNs and even the invasive cases appear to have a significantly better overall prognosis than pancreatobiliary- type adenocarcinomas unaccompanied by ICPNs [5].
In a study by Akita et al. they compared ICPNs defined by the more stringent criteria and other papillary carcinomas of the GB and they found ICPNs to show more frequent mucin hypersecretion, lacked lymphovascular invasion, nodal metastasis, and were recurrence-free. Using whole exome and Sanger sequencing, stringently defined ICPN were found to harbor mutations in STK11 and CTNNB1 but not in other papillary or non-papillary carcinomas of the gallbladder. The authors also stated that ICPNs share clininopatholgical features with their pancreatic counterpart [12].
Nakanuma et al. [6] referred to all papillary growing tumors as ICPNs, except for BilINs, PGAs, and invasive carcinomas of the gallbladder with considerable intraluminal papillary components, and proposed separating ICPNs into type 1 and 2, as in IPNBs [6]. Our study showed ICPN component in 0.21% of cholecystectomies which is less compared to Adsay et al. [5] (0.4%). 13.7% of gall bladder neoplasms were ICPN which is less compared to Hazarika et al. [6] which was 23.5% of gall bladder neoplasm. 50% (51/102) of the cases showed malignancy. 19.6% (10/51) of malignant GB cases showed presence of ICPN component in our study which is more compared to Adsay et al. [5] (6.4%).
As described in the above table (Table 3), our study showed highest association of ICPN with invasive malignancy compared to other studies. In addition, high grade dysplasia was present in all the cases of ICPN with invasive malignancy. Pure intestinal phenotype was seen in 9 of 14 of our ICPN cases (64%) and remaining 5 had mixed intestinal and biliary differentiation. This is contrary to the findings in other studies like Hazarika et al and Y. Nakamuna et al. In Hazarika et al, biliary and pyloric subtypes were most common constituting 37% each. In Nakunuma et al., gastric subtype (28.9%) was most common followed by biliary subtype (18.4%). In Adsay et al. [5], biliary (50%) was most common followed by gastric (36%) subtype.

Conclusion
The pathological features of three neoplastic precursor lesions of GB documented in WHO 2019 were discussed here and of them ICPN is a relatively rare and new entity. Acknowledging the pathology of these precursor lesions is extremely important not only for pathologists but also for physicians, radiologists and surgeons. Few striking observations that were made in our study were firstly, the high association of ICPN with invasive malignancy. Secondly, the most common histological type was ICPN with intestinal differentiation. Thirdly, high grade dysplasia was present in all the cases of ICPN that had associated invasive components. We hope new technologies will provide more valuable data regarding precursor neoplastic lesions of the gallbladder soon.
References
- National Cancer registry programme (2012) Consolidated report of population-based cancer registries: 2012-14.
- Freddie Bray, Jacques Ferlay, Isabelle Soerjomataram, Rebecca L Siegel, Lindsey A Torre, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6): 394-424.
- Hundal R, Shaffer EA (2014) Gallbladder cancer: epidemiology and outcome. Clin Epidemiol 6: 99-109.
- WHO Classification of Tumours Editorial Board (2019) WHO Classification of Tumours. In Digestive System Tumours, 5th ; International Agency for Research on Cancer: Lyon, France.
- Adsay V, Jang KT, Roa JC, Dursun N, Ohike N, et al. (2012) Intracholecystic papillary tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥0 cm): Clinicopathologic and immunohistochemical analysis of 123 cases. Am J SurgPathol 36(9): 1279-301.
- Nakanuma Y, Nomura Y, Watanabe H, Terada T, Sato Y, et al. (2021) Pathological characterization of intracholecystic papillary neoplasm: A recently proposed preinvasive neoplasm of gallbladder. Ann Diagn Pathol 52: 151723.
- Hazarika P, Sharma MK (2018) Intracholecystic papillary tubular neoplasm of gallbladder: A 5-year retrospective pathological study. Indian J Pathol Microbiol 61: 516-519.
- Argon A, Barbet FY, Nart D (2016) The relationship between intracholecystic papillary tubular neoplasms and invasive carcinoma of the gallbladder. Int J Surg Pathol 24(6): 504-511.
- Bennett S, Marginean EC, Paquin-Gobeil M, Wasserman J, Weaver J, et al. (2015) Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder. HPB (Oxford) 17(17): 811-818.
- Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO classification of tumours. In Digestive System Tumours, 4th ed.; International Agency for Research on Cancer: Lyon, France 3.
- He C, Fukumura Y, Toriyama A, Ogura K, Sasahara N, et al. (2018) Pyloric gland adenoma (PGA) of the gallbladder. Aunique and distinct tumor from PGAs of the stomach, duodenum, and pancreas. Am J Surg Pathol 42(9): 1237-1245.
- Akita M, Fujikura K, Ajiki T, Fukumoto T, Otani K, et al. (2019) Intracholecystic papillary neoplasms are distinct from papillary gallbladder cancers: A clinicopathologic and exome-sequencing study. Am J Surg Pathol 43: 783-791.






























