Prevalence of Cancer Cachexia and Associated Risk Factors at the Dominican Hospital Centre Saint Martin Porres in the city of Yaounde – Cameroon
Elisée Libert Embolo Enyegue1*, Souriou Soufianou5, Francine Fokam Foka2, Cyrille Bruno Mogo4, Halidou Awalou1, Floride Enstelle Ngono Abondo5, Bertrand Fonuy3, Sagne Zetekouang Dongmo3, Jafarou Mounpou5 and Cedric Tchinda Fossi6
1Laboratory of Cytopathology and Anatomy, Centre for Research on Health Priority Pathology, Institute of Medical Research and Medicinal Plant Studies, Cameroon
2Department of Clinical biology, Estuary Academic and Strategic Institute (IUEs/INSAM), Douala, University of Buea, Cameroon
3Dominican Hospital Centre Saint Martin Porres, laboratory of cytopathology and anatomy, Cameroon
4Institute of Medical Research and Medicinal Plants Studies, Centre of Research on Health and Priority Pathology, Molecular Biology and Biotechnology Laboratory, Cameroon
5Food Study and Quality Control Laboratory, Centre for research on food, food security and nutrition, Institute of Medical Research and Medicinal Plants Studies, Cameroon
6Pharmacology and Drugs Discovery Laboratory, Centre for Research on Medicinal Plants and Traditional Medicine, Institute of Medical Research and Medicinal Plants Studies (IMPM), Ministry of Scientific Research and Innovation, Cameroon
Submission: October 27, 2024; Published: November 08, 2024
*Corresponding Address: Elisée Libert Embolo Enyegue, Laboratory of Cytopathology and Anatomy, Centre for Research on Health Priority Pathology, Institute of Medical Research and Medicinal Plant Studies, Cameroon
How to cite this article: Elisée L E E, Souriou S, Francine F F, Cyrille B M, Halidou A, et al. Prevalence of Cancer Cachexia and Associated Risk Factors at the Dominican Hospital Centre Saint Martin Porres in the city of Yaounde – Cameroon. Canc Therapy & Oncol Int J. 2024; 27(5): 556225. DOI:10.19080/CTOIJ.2024.27.556225
Abstract
Background: Cachexia, a syndrome characterized by weight loss and muscle mass loss, is a common complication in patients with chronic diseases. This study aims to examine the prevalence and associated factors of cachexia in Cameroon among individuals living with solid cancer. Cachexia is poorly studied in Sub-Saharan Africa, despite its clinical relevance and impact on patients’ quality of life. Understanding its prevalence and determinants is crucial for improving healthcare and interventions in this region. The aim of this study was to determine the risk factors of this pathology and to determine the factors associated with it.
Methodology: A cross-sectional study was conducted on 73 patients, stratified by age, sex, marital status, ethnicity, and BMI. Data was collected via questionnaires and clinical measurements, and statistically analysed to identify prevalences and significant associations.
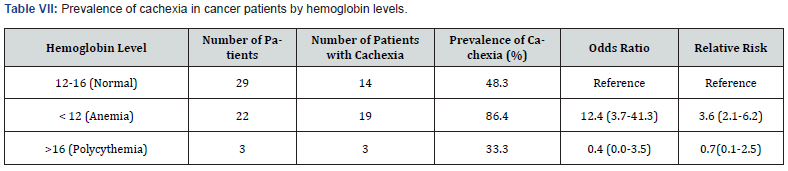
Results: The 73 participants studied were primarily aged 30-39 years (28.4%), followed by 40-49 years (20.3%) and 50-59 years (17.6%). In terms of marital status, 45.2% were married, 43.8% single, 9.6% widowed, and 1.4% in a common-law relationship. The majority ethnicity included Betsi (42.5%) and Bamiléké (37.0%). Women represented 78.1% of the population. The prevalence of cachexia was highest among 60-69-year-olds (83.3%) and lowest among 20-29-year-olds (25.0%), with statistical significance for 50-59 and 60-69-year-olds (p < 0.001). Widowed individuals had the highest prevalence (71.4%), compared to married (42.4%) and single (34.4%) individuals, with statistical significance (p < 0.001 and p = 0.003, respectively). Cachexia was most prevalent among Bassa’a (100%) and Bamiléké (48.1%), with statistical significance (p = 0.001 and p = 0.026, respectively). Women had a prevalence of 47.4%, higher than that of men (37.5%), with a significant difference (p = 0.003). Patients with a BMI below 18.5 had a prevalence of 80%, with a relative risk of 2.7. Those who were overweight/obese had a prevalence of 52.6%, without statistical significance. Cachexia was more frequent in patients with cervical (60%) and colon (40%) cancers, with high odds ratios for cervical and pancreatic cancers (OR = 3.4). Patients with albumin levels below 35 g/L had a prevalence of 83.3% (OR = 5.5). The prevalence increased with CRP levels, reaching 90.9% among those with CRP > 96 mg/L (OR = 19.5). Anemic patients had a prevalence of 86.4% (OR = 12.4), compared to 48.3% for those with normal hemoglobin. Patients with high hemoglobin levels had a prevalence of 100%, but with an OR of 0.4, indicating a reduced risk of cachexia.
Conclusion: This study reveals a significant prevalence of cachexia among solid cancer patients in Cameroon, particularly among older individuals, widowed individuals, women, and those with low BMI. Associated factors include low albumin levels, inflammation, and anemia. These results highlight the need for targeted strategies for the prevention and management of cachexia in this population.
Keywords: Cachexia; Cancer; Prevalence; Risk factors; Dominican Hospital Centre Saint Martin Porres; Cameroon
Introduction
Cachexia remains a major challenge for patients with cancer [1]. It is a systemic metabolic syndrome characterized by involuntary weight loss and muscle and adipose tissue wasting [2]. Cancer cachexia was defined as a multifactorial syndrome defined by an ongoing loss of skeletal muscle mass (with or without loss of fat mass) that cannot be fully reversed by conventional nutritional support and leads to progressive functional impairment. Its pathophysiology is characterized by a negative protein and energy balance driven by a variable combination of reduced food intake and abnormal metabolism. The agreed diagnostic criterion for cachexia was weight loss greater than 5%, or weight loss greater than 2% in individuals already showing depletion according to current bodyweight and height (body-mass index [BMI] <0x7E> 20 kg/m(2)) or skeletal muscle mass (sarcopenia) [3]. Cancer cachexia occurs in 30%-80% of patients, increasing morbidity and mortality and impacting the health-related quality of life also for caregivers. Pharmacological interventions have been studied but have shown inconsistent effects on patients’ lives in terms of relative outcomes and poor adherence to pharmacological treatment [4]. Cachexia occurs also in heart failure. With global aging, the number of patients with heart failure has increased markedly. Heart failure is a complex condition intricately associated with aging, organ damage, frailty, and cognitive decline, resulting in a poor prognosis [5]. Decreased skeletal muscle mass, muscle strength, and function have been reported to have adverse effects on QOL and life expectancy and have recently become widely known as sarcopenia. With the aging population in developed countries, countermeasures against aging-related sarcopenia are attracting attention. On the other hand, cachexia, which is secondary to sarcopenia caused by chronic diseases, remains less recognized among medical professionals compared to sarcopenia, although there are many opportunities to encounter it in daily practice [6].
There are many cases of undiagnosed cachexia in which the nutritional status deteriorates, resulting in further loss of skeletal muscle mass and physical functional decline. In 2011, a consensus definition of cachexia was proposed, and the number of relevant research reports has increased significantly [3]. However, the pathogenesis of cachexia is not fully understood, and there are currently few regulatory-approved standard treatments for cachexia [7]. The main reason for this is that multiple etiologies are involved in the development of cachexia. For a long time, cachexia had been understood as an inevitable condition associated with the progression of underlying diseases and was not subject to treatment or research, but various subsequent studies have gradually revealed that various molecular mechanisms in skeletal muscle, adipose tissue, the digestive system, the central nervous system, and the immune system are involved in the development of cachexia [8]. Having established the background and significance of cachexia in patients with solid cancers in Cameroon, it is essential to explore the specific methods used to investigate this syndrome within the study population. The following section outlines the methodological approach adopted to assess the prevalence and associated risk factors of cachexia among these patients.
Methodology
Justification of study location
Cameroon bears a significant burden of chronic diseases, including cancer, with significant implications for public health. Studying cachexia in this context is relevant to understanding its local impacts and adapting management strategies. Socio-economic conditions and available resources influence the prevalence and management of health conditions like cachexia. The Cameroonian context provides an opportunity to explore these specific dynamics.
Target population: Adult patients diagnosed with solid cancer in Cameroon.
Inclusion criteria: Patients aged 18 years and above. Confirmed diagnosis of solid cancer; Informed consent to participate in the study.
Sampling technique: non-probabilistic sampling, such as convenience sampling or quota sampling based on age, sex, and cancer type.
Data collection: Use of structured questionnaires to collect demographic data (age, sex, marital status, ethnicity), medical history (cancer type, stage), and anthropometric measures (BMI). Blood sample collection for biochemical parameters such as albumin, CRP (C-reactive protein), and hemoglobin.
Parameter assays:
Albumin: Utilize standardized colorimetric methods.
CRP: Assay using immunoturbidimetry.
Hemoglobin: Measurement via spectrophotometry.
Statistical analysis: Statistical tests (chi-square test, logistic regression) to identify prevalence and significant associations between cachexia and studied variables (age, sex, marital status, ethnicity, BMI, cancer types, albumin levels, CRP, hemoglobin) were used.
Results
Population by socio-demographic factors
Table I below presents demographic data on a population, including age distribution, marital status, gender, and ethnicity. The majority of the population is between 30-39 years old (28.4%) and either married (45.2%) or single (43.8%). Females outnumber males, with 78 females and 22 males. The most common ethnicities are Betsi (42.5%) and Bamileke (37%), while the least common are Bassa’a, Douala, and Bamoun (1.4% each). The table also provides 95% confidence intervals for the percentages in each category, indicating the estimated range of the true population percentage with a 95% level of confidence.



Prevalence of cachexia by age
Table II presents data on the prevalence of cachexia in a patient population across different age groups. The prevalence of cachexia increases with age, with the highest prevalence observed in the age group of 60-69 years (83.3%). The lowest prevalence of cachexia was observed in the age group of 20-29 years (25.0%). The p-value of 0.0002 indicates a statistically significant association between age and the prevalence of cachexia. The 95% confidence intervals for the prevalence of cachexia in each age group are also provided, indicating the estimated range of the true population prevalence with a 95% level of confidence.
Prevalence of cachexia by marital status
Table III below presents data on the prevalence of cachexia among patients based on their marital status. The prevalence of cachexia was highest among widowed patients (71.4%), followed by married patients (42.4%), and single patients (34.4%). The p-value of 0.003 indicates a statistically significant association between marital status and the prevalence of cachexia. The 95% confidence intervals for the prevalence of cachexia in each marital status group are also provided, indicating the estimated range of the true population prevalence with a 95% level of confidence.
Prevalence of cachexia by gender
The Figure 1 below presents data on the prevalence of cachexia among patients by sex. The prevalence of cachexia was higher among female patients (47.4%) compared to male patients (37.5%). The p-value of 0.003 indicates a statistically significant association between sex and the prevalence of cachexia. The 95% confidence intervals for the prevalence of cachexia in each sex group are also provided, indicating the estimated range of the true population prevalence with a 95% level of confidence.
Prevalence of cachexia for each group
Table IV shows the number of patients with each type of cancer, the number of patients with cachexia, the prevalence of cachexia, and the relative risk (RR) for each type of cancer. The prevalence of cachexia varies widely across different types of cancer, with the highest prevalence observed in patients with stomach cancer (100%) and pancreatic cancer (100%), and the lowest prevalence observed in patients with cavum cancer (0%) and testicular cancer (0%). However, it is important to note that the small sample size for some types of cancer may limit the generalizability of these findings. The relative risk (RR) indicates the risk of cachexia in patients with a particular type of cancer compared to the risk in patients with other types of cancer.
General prevalence of cachexia
Figure 2 below shows the prevalence of different types of cancers in a given population. Breast cancer is the most common (42.3%), followed by cervical cancer (15.4%) and ovarian cancer (11.5%). Colon, rectal, and stomach cancers each have a prevalence of 7.7%. Lung and cavum cancers are less common, each representing 3.8% of cases. No cases of pancreatic cancer, testicular cancer, endometrial adenocarcinoma with pleural metastasis, or squamous cell carcinoma of the left-hand ulcer were observed (0.0%). In summary, gynecological and digestive cancers dominate the cancer prevalence in this population.





Cachexia and albumin level
This Table V shows the prevalence of cachexia in the study population based on albumin levels. The albumin levels were categorized as normal (35-52 g/l), low (<35 g/l), and high (>35 g/l). The prevalence of cachexia was highest in the low albumin group (83.3%), followed by the normal albumin group (48.3%), and the lowest prevalence was in the high albumin group (33.3%). The odds ratio and relative risk indicate that patients with low albumin levels were more likely to have cachexia compared to those with normal albumin levels, while those with high albumin levels were less likely to have cachexia.
Cachexia and CRP
This Table VI shows the prevalence of cachexia in cancer patients based on their CRP levels. CRP is a marker of inflammation, and elevated CRP levels have been associated with an increased risk of cachexia in cancer patients.
Cachexia and hemoglobin level
Table VII shows the prevalence of cachexia among cancer patients based on their hemoglobin levels. Hemoglobin is a protein in red blood cells that carries oxygen throughout the body, and low hemoglobin levels (anemia) have been associated with an increased risk of cachexia in cancer patients.
Discussion
Cachexia is a complex metabolic disorder characterized by loss of muscle mass and strength, with or without loss of fat mass, that cannot be fully reversed by conventional nutritional support. It is a common complication in cancer patients, affecting up to 80% of advanced cancer patients, and is associated with poor quality of life, reduced response to treatment, and shorter survival. This aimed at evaluating the prevalence of cachexia among people living with cancer. Preliminary results showed that the majority of participants were between 30 and 49 years old (48.7%). The majority of participants were married (45.2%), followed by those who were single (43.8%). The majority of participants were women, while a smaller proportion were men. Vargas and collaborators showed that, highest percentage of cancer patients was observed in the age group of 65 years and more, 48% [9]. The majority of participants being married (45.2%) and single (43.8%) may reflect the general population distribution in the region where the study was conducted. It is also possible that marital status may be associated with certain health behaviors or access to healthcare, which could impact the outcomes of interest in the study.
The majority of participants being women is consistent with previous research showing that cancer incidence and mortality rates are generally higher in men than in women, but the gender distribution varies by cancer type and other factors such as age and geographic region. The higher proportion of women in the study population may be due to the types of cancer being studied or other factors related to the study design or recruitment strategies. Regarding the age distribution, the results presented differ from the findings of Vargas et al. [9], who reported that the highest percentage of cancer patients was observed in the age group of 65 years and older. This discrepancy may be due to differences in the study population, cancer types, or other factors. It is important to consider the specific context and characteristics of the study population when interpreting the results and comparing them to other studies. Overall, the sociodemographic characteristics of the study population can provide valuable insights into the generalizability of the study results and potential subgroup differences in the outcomes of interest. It is important to consider these factors when interpreting the results and drawing conclusions from the study.
The results presented by Johanne Poisson and collaborators [10] and the results of our study suggest that the prevalence of cachexia increases with age. In the study by Johanne Poisson and collaborators, the highest prevalence of cachexia was observed in patients aged 85 years and older (64%), while in the results mentioned in the question, the highest prevalence was observed in the age group of 60-69 years (83.3%). This discrepancy may be due to differences in the study population. Both studies also identified other factors associated with an increased risk of cachexia, such as cancer site and metastatic status. However, the specific factors identified differed between the two studies, which may be due to differences in the study population and methods used.
The results of our study suggest that marital status is significantly associated with the prevalence of cachexia, with the highest prevalence among widowed patients (71.4%) and the lowest among single patients (34.4%). These results differ from those of Takehito and collaborators, who found that sex, age, smoking history, emphysema, performance status, superior vena cava syndrome, clinical stage, site of metastasis, histology, EGFR mutation status, primary treatment method, and serum albumin levels were significantly associated with cancer cachexia [11].
However, our study did not examine these other factors, so it is possible that they also play a role in the development of cachexia. Popi Kasvis and collaborators found that cancer cachexia is common in advanced cancer and is accompanied by negative effects on health-related quality of life (HRQOL). They explored the use of two surrogate measures of HRQOL, feeling of wellbeing (FWB) on the Edmonton Symptom Assessment System (ESAS) questionnaire and the Distress Thermometer (DT), and found that refractory cachexia (RC) patients had a significantly poorer sense of wellbeing than the other cachexia stages [12]. They also found that FWB was negatively affected by worsening appetite in all CC stages except NC, and that cannabinoid treatment improved ESAS score for lack of appetite, but not weight. These results suggest that cancer cachexia has a significant impact on HRQOL, and that a multidisciplinary approach, including cannabinoid therapy, may be useful in improving HRQOL via appetite stimulation. The results of our study suggest that the prevalence of cachexia varies widely across different types of cancer, with the highest prevalence observed in patients with stomach cancer (100%) and pancreatic cancer (100%).
This is consistent with the findings of Søren Fisker Schmidt and collaborators, who noted that cancer cachexia is a multifactorial condition that affects various organs and is increasingly seen as a systemic phenomenon [13]. Our study also found that the prevalence of cachexia was lowest in patients with cavum cancer (0%) and testicular cancer (0%). Our study found that low albumin levels were a risk factor for cachexia in cancer patients, with the highest prevalence of cachexia in the low albumin group (83.3%). Low albumin levels may indicate malnutrition, which is a common comorbidity in cancer patients and a known risk factor for cachexia. In addition, inflammation can reduce albumin synthesis in the liver, leading to low albumin levels. Cancer patients with low albumin levels may have an increased risk of cachexia due to malnutrition and/or inflammation. Therefore, monitoring albumin levels in cancer patients may be useful in identifying those at risk for cachexia and implementing interventions to improve nutritional status and reduce inflammation.
This is consistent with the findings of Natália Fernandes-dos- Santos and collaborators, who found that hypoalbuminemia was associated with cachexia in cancer patients [14]. Our study also found that elevated CRP levels were a risk factor for cachexia, with the prevalence of cachexia increasing with increasing CRP levels. The results of Cristian Orellana López and collaborators found that the prevalence of cachexia in cancer patients was 27.5%, with 45.4% of patients having mild cachexia, 36.3% having severe cachexia, and 18.1% having moderate cachexia. They also found a significant positive correlation between the final scores and the stage of cancer [15]. This is consistent with the findings of Alex F. Bullock and collaborators, who found that percentage monthly weight loss was associated with cachexia in cancer patients [16]. The results of Johanne Poisson and collaborators found that 52% of cancer patients had cachexia, with patients with upper gastrointestinal tract cancers, previous surgery for cancer, metastases, poor performance status, low food intake, unfeasible timed up-and-go test, cognitive disorders or risk of depression being more likely to have cachexia [10].
They also found that cachexia was associated with a higher 6-month mortality risk independently of age, in/outpatient status, cancer site, metastatic status, cancer treatment, dependency, cognition, and number of daily medications. The high prevalence of cachexia in patients with stomach and pancreatic cancer could be explained by the fact that these cancers are often diagnosed at advanced stages, when the disease has already caused significant weight loss and muscle wasting. In addition, these cancers are associated with high levels of inflammation, which is a known risk factor for cachexia. The association between low albumin levels and cachexia could be explained by the fact that albumin is a marker of nutritional status and inflammation. Low albumin levels may indicate malnutrition, which is a common comorbidity in cancer patients and a known risk factor for cachexia.
In addition, inflammation can reduce albumin synthesis in the liver, leading to low albumin levels. The association between elevated CRP levels and cachexia could be explained by the fact that CRP is a marker of inflammation. Inflammation is a known risk factor for cachexia, as it can lead to muscle wasting and anorexia. In addition, inflammation can increase energy expenditure, leading to weight loss and further exacerbating cachexia. The high prevalence of cachexia in patients with anemia could be explained by the fact that anemia is a common comorbidity in cancer patients and is associated with reduced appetite, fatigue, and decreased physical activity, all of which can contribute to muscle wasting and weight loss. The findings from Søren Fisker Schmidt and collaborators suggest that cancer cachexia is a systemic phenomenon that affects multiple organs and is influenced by various factors, including inflammation, metabolic alterations, and tissue crosstalk.
This highlights the need for a comprehensive approach to the management of cancer cachexia, targeting multiple pathways and addressing the underlying mechanisms of the condition. Overall, these studies highlight the complex nature of cancer cachexia and the need for a comprehensive understanding of its etiology and heterogeneity to develop effective intervention strategies. Our study contributes to this understanding by identifying risk factors for cachexia in cancer patients, including low albumin levels and elevated CRP levels. However, further research is needed to determine the underlying mechanisms linking these factors to cachexia and to explore potential interventions for improving albumin levels and reducing inflammation in cancer patients.
Conclusion
Cachexia is a complex metabolic disorder that commonly affects cancer patients, particularly those with advanced stages of the disease. The prevalence of cachexia among cancer patients varies widely depending on the type of cancer, with the highest prevalence observed in patients with stomach and pancreatic cancer. Risk factors for cachexia in cancer patients include low albumin levels, elevated CRP levels, and anemia. Cachexia has a significant impact on health-related quality of life, and a multidisciplinary approach, including cannabinoid therapy, may be useful in improving HRQOL via appetite stimulation. Further research is needed to determine the underlying mechanisms linking risk factors to cachexia and to explore potential interventions for improving albumin levels and reducing inflammation in cancer patients. A comprehensive understanding of the etiology and heterogeneity of cancer cachexia is necessary to develop effective intervention strategies.
Acknowledgement
The authors express their sincere gratitude to the director and staff of the Dominican Hospital Center Saint Martin Porres for facilitating access and data collection.
Research Funding
Not applicable
Availability of data and material
All data generated or analyzed in the course of this study are included in this manuscript.
Author’s contributions
ALEE and FFF: carried out the research work and designed laboratory works, ELEE: prepared the first draft of the manuscript and participated in revision and formatting of the final version.
HA: Collected data and laboratory works. BF and SZD: revised the manuscript. CFT and ELEE conceived the study and revised the final form manuscript. All authors have read, revised and approved the final version of the manuscript.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical Approval Not applicable.
Consent to Participate Not applicable.
Consent to Publish Not applicable.
Conflict of Interest
The authors declare no competing interests.
References
- Mingyang Liu, Yu Ren, Zhijun Zhou, Jingxuan Yang, Xiuhui Shi, et al. (2024) The crosstalk between macrophages and cancer cells potentiates pancreatic cancer cachexia. Cancer Cell 42(5): 885-903.
- Xue Yang, Jianming Wang, Chun-Yuan Chang, Fan Zhou, Juan Liu, et al. (2024) Leukemia inhibitory factor suppresses hepatic de novo lipogenesis and induces cachexia in mice. Nat Commun 15(1): 627.
- Kenneth Fearon, Florian Strasser, Stefan D Anker, Ingvar Bosaeus, Eduardo Bruera, et al. (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5): 489-495.
- E Bertocchi, F Frigo, L Buonaccorso, F Venturelli, MC Bassi, et al. (2024) Cancer cachexia: A scoping review on non-pharmacological interventions. Asia-Pac J Oncol Nurs 11(5): 100438.
- Daichi Maeda, Yudai Fujimoto, Taisuke Nakade, Takuro Abe, Shiro Ishihara, et al. (2024) Frailty, Sarcopenia, Cachexia, and Malnutrition in Heart Failure. Korean Circ. J 54(7): 363-381.
- M Muscaritoli, SD Anker, J Argilés, Z Aversa, JM Bauer et al. (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: Joint document elaborated by Special Interest Groups (SIG) cachexia-anorexia in chronic wasting diseases and nutrition in geriatrics. Clin. Nutr 29(2): 154-159.
- H Wakabayashi, H Arai, A Inui (2021) The regulatory approval of anamorelin for treatment of cachexia in patients with non-small cell lung cancer, gastric cancer, pancreatic cancer, and colorectal cancer in Japan: facts and numbers. J Cachexia Sarcopenia Muscle 12(1): 14-16.
- H Nishikawa, M Goto, S Fukunishi, A Asai, S Nishiguchi, et al. (2021) Cancer Cachexia: Its Mechanism and Clinical Significance. Int J Mol Sci 22(16): 8491
- Y Vargas-Arce, L Abarca-Gómez (2016) Prevalence of cachexia related to cancer in patients at a primary level: a palliative approach. Acta Médica Costarric 58(4): 171-177.
- Johanne Poisson, Claudia Martinez-Tapia, Damien Heitz, Romain Geiss, Gilles Albrand, et al. (2021) Prevalence and prognostic impact of cachexia among older patients with cancer: a nationwide cross‐sectional survey (NutriAgeCancer). J Cachexia Sarcopenia Muscle 12(6): 1477-1488.
- T Shukuya, Kazuhisa Takahashi, Yasushi Shintani, Keita Miura, Ikuo Sekine, et al. (2023) Epidemiology, risk factors and impact of cachexia on patient outcome: Results from the Japanese Lung Cancer Registry Study. J Cachexia Sarcopenia Muscle 14(3): 1274-1285.
- P Kasvis, M Vigano, A Vigano (2019) “Health-related quality of life across cancer cachexia stages. Ann Palliat Med 8(1).
- Pauline Morigny, Doris Kaltenecker, Julia Zuber, Juliano Machado, Lisa Mehr, et al. (2021) Association of circulating PLA2G7 levels with cancer cachexia and assessment of darapladib as a therapy. J Cachexia Sarcopenia Muscle 12(5): 1333-1351.
- N Fernandes-dos-Santos, C Porto-Sabino-Pinho, AJ Pacheco-Ferro-Cardoso, RM Lins-Mendes (2018) Cachexia in hospitalized patients with heart failure. Nutr Hosp 35(3): 669-676.
- Jose Leyton Estéfane, Miguel Ramos Rosales (2023) Prevalence of Cachexia in Cancer Patients. Eur J Cancer Care (Engl) 2023(1): 5743872.
- AF Bullock, MJ Patterson, LW Paton, DC Currow, MJ Johnson (2024) Malnutrition, sarcopenia and cachexia: exploring prevalence, overlap, and perceptions in older adults with cancer. Eur J Clin Nutr 78(6): 486-493.






























