Atypical Presentation of Non-Uremic Calciphylaxis in Advanced Lung and Prostate Cancer Patient
Ana Sanchez de Torre1*, Pedro Pablo Garcia Montero2, Alejandro Estrada Santiago3, Nuria Garcia Pons6, Coralia Bueno Muino1, Elsa Bernal Hertfelder1, Maria Garcia Ferron1, Alejandro Riquelme Oliveira1, Maria del Camino Medina Puente4, Laura Muniz Pacios5 and Francisco Javier Teigell Munoz3
1Medical Oncology, Hospital Universitario Infanta Cristina, Madrid, Spain
2Dermatology, Hospital Universitario Infanta Cristina, Madrid, Spain
3Internal Medicine, Hospital Universitario Infanta Cristina, Madrid, Spain
4Pathology department, Hospital Universitario Infanta Cristina, Madrid, Spain
5Nephrology, Hospital Universitario Infanta Cristina, Madrid, Spain
6Nurse practitioner. Hospital Universitario Infanta Cristina, Madrid, Spain
Submission: April 01, 2024; Published: April 16, 2024
*Corresponding Address: Ana Sanchez de Torre, Medical Oncology, Hospital Universitario Infanta Cristina, Madrid, Spain
How to cite this article: Ana Sanchez de Torre*, Pedro Pablo Garcia Montero, Alejandro Estrada Santiago, Nuria Garcia Pons, Coralia Bueno Muino, et al. Atypical Presentation of Non-Uremic Calciphylaxis in Advanced Lung and Prostate Cancer Patient. Canc Therapy & Oncol Int J. 2024; 26(3): 556190. DOI:10.19080/CTOIJ.2024.26.556190
Abstract
Calcipylaxis is a rare and highly morbid disorder characterized by vascular calcification and subsequent cutaneous tissue necrosis and ulceration. It is usually seen in patients with chronic kidney disease treated by dialysis but is also described in patients with normal kidney function. Histopathology from skin biopsy remains the goal standard diagnostic tool. Evidence of treatment is limited. We report an unusual case of calciphylaxis in association with metastatic lung and prostate cancer in the absence of end-stage renal or parathyroid disease successfully treated with long-term sodium thiosulfate and wound care. This case demonstrates the importance of considering calciphylaxis in the differential diagnosis in patients presenting with painful skin ulcerations, despite normal laboratory levels.
Keywords: Non-uremic calciphylaxis; Cancer; Ulceration; Renal function; Sodium tiosulphate; Hospital at home
Abbreviations: PTH: Parathyroid Hormone; CT: Computed Tomography; IV: Intravenous
Introduction
Calciphylaxis is an uncommon, life-threatening syndrome described by Selye in 1962 [1]. It is characterized by calcification and occlusion of small blood vessels in the subcutaneous adipose tissue and dermis [2,3]. Clinically, it presents with bilateral painful, indurated, and violaceous skin rash, most often on the extremities. Then, rash progresses to bullae or well-demarcated nonhealing ulcerations with jagged black eschar formation, necrosis, and gangrene [4]. Patients often develop infections within the necrotic areas and death from fulminant sepsis is common [5].
The pathogenesis of calciphylaxis remains uncertain. Calciphylaxis is thought to be due to derangement of the calcium-phosphorus metabolism leading to deposition of calcium phosphate crystals. The elevated calcium-phosphorus product acts as a sensitizer in a patient later exposed to a challenger, resulting in vascular calcification and increased susceptibility to thrombosis and infarction [6]. It is most frequently associated with patients with end-stage renal disease, hemodialysis, and hyperparathyroidism. However, it has also been reported in patients with both normal renal and parathyroid function [7] and a variety of other associations, including metastatic tumors and antineoplastic drugs. Once calciphylaxis has been diagnosed, the prognosis is generally poor (survival, <1 year) [8-10]. Due to its high mortality, early identification and aggressive multidisciplinary management are necessary to improve patient outcomes.
Case Report
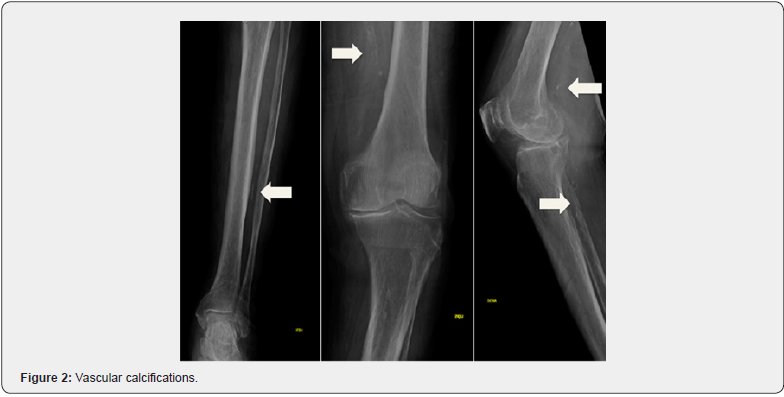
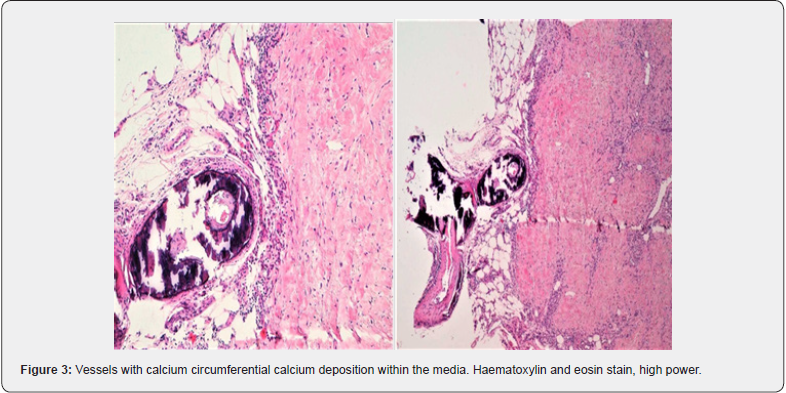
A 73-year-old male patient presented our institution with painful and extensive leg ulcers that had progressed over 2 months. He was diagnosed with metastatic non-small cell lung cancer on treatment with atezolizumab for 4 years without evidence of progression disease and castration resistant prostate cancer with bone lesions, a condition for which he was receiving androgen deprivation therapy and enzalutamide for 2 years. Additional past medical history included hypertension and type 2 diabetes mellitus on treatment with amlodipine and sitagliptin respectively. Dermatological examination found large retiform leg ulcers with a necrotic background and superinfection signs, surrounded by a purplish rim on his lower limbs (Figure 1). The lesions were extremely painful to palpation. Swabs taken from the ulcers revealed infection with Pseudomonas aeruginosa and Staphylococcus aureus highly sensitive to fluoroquinolones. Leg X-rays showed several arterial calcification (Figure 2) and skin biopsy revealed calcification in muscular arteries with vascular necrosis, compatible con calciphylaxis diagnosis (Figure 3).

An extensive laboratory investigation showed calcium, phosphorous, parathyroid hormone (PTH) and PTH-related protein to all be within normal limits. Computed tomography (CT) and bone scan showed stable oncological disease. High-dose 2-week course of levofloxacin, pain medication and intravenous (IV) sodium thiosulfate 3 times a week (12.5 g IV) was initiated and well tolerated. The dose was then increased to 25 g 3 times a week. A specialized nurse performed skin cures initially daily and subsequently every 48 hours. Due to initial favorable evolution and considering the need for long-term therapy, hospital at home support was proposed to avoid repeat hospital visits. After 4 months of treatment, the size of the wounds was reduced by more than 50% (Figure 4). Sodium thiosulfate was progressively reduced to 1 administration each week. Complete healing was achieved within 8 months (Figure 5), allowing definitive stop of treatment without recurrence to this day.


Discussion
Calciphylaxis is a rare and serious condition characterized by the calcification of small- to medium- sized blood vessels, leading to ischemia and necrosis of the surrounding tissues. While calciphylaxis is most frequently associated with end-stage renal disease, there have been sporadic cases in individuals with normal renal function, including cancer patients. A systemic review by Nigwekar in 2008, described 36 cases of non-uremic calciphylaxis, out of which eight cases were reported malignancies such as metastatic breast cancer, cholangiocarcinoma, myeloma, and malignant melanoma [11]. However, our case is the first one published of calciphylaxis in association with metastatic prostate and lung cancer. Calciphylaxis etiopathogenesis remains unclear. Moreover, the association between calciphylaxis and cancer is not fully understood, and the condition is often considered idiopathic in non-uremic patients. Nevertheless, there are several mechanisms and risk factors that may contribute to the development of calciphylaxis in cancer patients with normal renal functions that are important to recognize and screen for.
Cancer patients may experience abnormalities in calciumphosphorus metabolism. Hypercalcemia can promote vascular calcification, contributing to the development of calciphylaxis. Also, disruption of PTH regulation can impact calcium homeostasis and contribute to soft tissue calcification. In this case, despite the absence of alteration in laboratory parameters, bone involvement secondary to castration resistant prostate cancer could be likely a significant risk factor. Chronic inflammation, common in cancer patients, may play a role in the development of calciphylaxis. Inflammatory processes can contribute to vascular damage and calcification. Also, treatments used in cancer patients, such as certain chemotherapeutic agents and corticosteroids can affect calcium metabolism and potentially contribute to the development of calciphylaxis [12]. Our patient was on treatment with enzalutamide and atezolizumab. No data regarding skin toxicity from this combination, except rash [13].
In our patient, the differential diagnosis of non-uremic calciphylaxis includes immune related toxicity, peripheral vascular disease, other inflammatory diseases, infections, and iatrogenic disorders [14]. However, histopathology from skin biopsy confirmed calciphylaxis diagnosis. Treatment of calciphylaxis in cancer patients with normal renal function involves addressing underlying causes and providing wound care. Unfortunately, there is no approved therapy for the management of calciphylaxis. Treatment is focused on preventing complications and symptom control. Pain should be adequately controlled and disruptions in the skin should be promptly managed with appropriate wound care and if necessary, antibiotics. Sodium thiosulphate has been found to be beneficial in managing both uremic and non-uremic calciphylaxis [15]. Calciphylaxis often carries a poor prognosis. The one-year mortality of calciphylaxis is 50%, but this increases to 80% in presence of ulceration with superinfection and sepsis [16]. Fortunately, our patient experienced progressive improvement after a few sodium thiosulfate infusions.
It’s essential for healthcare providers to be vigilant in monitoring cancer patients for signs and symptoms of calciphylaxis, even in the absence of renal impairment. Early diagnosis is crucial for better outcomes, as the condition can progress rapidly and lead to severe complications, including skin ulcers, tissue necrosis, infection, and death. Multidisciplinary collaboration between oncologists, internists, nephrologists and dermatologists is often necessary to tailor an effective treatment plan. Hospital at home support is proposed as a tool to provide a response to the increasing health care demands. It consists of providing hospital clinical attention at the patient’s home instead of institutional care. Robust evidence suggests that hospital at home intervention is a new option to treat and monitor patients. Outcomes equivalent to in-patient stays with no mortality difference and cost reduction makes this model a viable option for patient care outside of the hospital [17].
Conclusion
While calciphylaxis is more commonly associated with renal impairment, it can occur in cancer patients with normal renal function due to various factors. Further research is needed to better understand the specific mechanisms linking cancer and calciphylaxis in patients without kidney disease and to develop targeted therapeutic approaches. Mainstays of treatment include sodium thiosulphate, wound care and infection control. The Hospital at home model remains a new opportunity to provide hospital-level services to eligible patients at home, with favorable results, improvement in quality of life and important cost reduction.
Conflicts of Interest
No conflicts of interest to declare.
Acknowledgement
To the patient and his family.
Informed Consent
Informed consent was obtained by the patient.
References
- Dieudonne JM, Veilleux R, Selye H (1962) Calciphylaxia. Presse Med 70: 1068-1070.
- Beus KS, Stack BC (2004) Calciphylaxis. Otolaryngol Clin North Am 37(4): 941-948.
- Mathur RV, Shortland JR, el-Nahas AM (2001) Calciphylaxis. Postgrad Med J 77(911): 557-561.
- Weenig RH, Sewell LD, Davis MDP, McCarthy JT, Pittelkow MR (2007) Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol 56(4): 569-579.
- Trent JT, Kirsner RS (2001) Calciphylaxis: diagnosis and treatment. Adv Skin Wound Care 14(6): 309-312.
- Chen TY, Lehman JS, Gibson LE, Lohse CM, El-Azhary RA (2017) Histopathology of Calciphylaxis: Cohort Study With Clinical Correlations. Am J Dermatopathol 39(11): 795-802.
- Kalajian AH, Malhotra PS, Callen JP, Parker LP (2009) Calciphylaxis with normal renal and parathyroid function: not as rare as previously believed. Arch Dermatol 145(4): 451-458.
- Nigwekar SU, Zhao S, Wenger J, Hymes JL, Maddux FW, et al. (2016) A Nationally Representative Study of Calcific Uremic Arteriolopathy Risk Factors. J Am Soc Nephrol JASN 27(11): 3421-3429.
- McCarthy JT, El-Azhary RA, Patzelt MT, Weaver AL, Albright RC, et al. (2016) Survival, Risk Factors, and Effect of Treatment in 101 Patients with Calciphylaxis. Mayo Clin Proc 91(10): 1384-1394.
- Fine A, Zacharias J (2002) Calciphylaxis is usually non-ulcerating: risk factors, outcome and therapy. Kidney Int 61(6): 2210-2217.
- Nigwekar SU, Wolf M, Sterns RH, Hix JK (2008) Calciphylaxis from nonuremic causes: a systematic review. Clin J Am Soc Nephrol CJASN 3(4): 1139-1143.
- Seethapathy H, Noureddine L (2019) Calciphylaxis: Approach to Diagnosis and Management. Adv Chronic Kidney Dis 26(6): 484-490.
- Powles T, Yuen KC, Gillessen S, Kadel EE, Rathkopf D, et al. (2022) Atezolizumab with enzalutamide versus enzalutamide alone in metastatic castration-resistant prostate cancer: a randomized phase 3 trial. Nat Med 28(1): 144-153.
- Brasileiro A, Ribeiro R, Silva PE, Fidalgo A (2015) Stellate ulceration in a nonuremic patient. Cleve Clin J Med 82(11): 719-20.
- Ning MS, Dahir KM, Castellanos EH, McGirt LY (2013) Sodium thiosulfate in the treatment of non- uremic calciphylaxis. J Dermatol 40(8): 649-652.
- Altman K, Shinohara M (2019) Demographics, Comorbid Conditions, and Outcomes of Patients With Nonuremic Calciphylaxis. JAMA Dermatol 155(2): 251-252.
- Gaillard G, Russinoff I (2023) Hospital at home: A change in the course of care. J Am Assoc Nurse Pract 35(3): 179-182.






























