Treatment Delivery within a Helical Geometry in Whole-Breast Radiotherapy on Tomotherapy Machine: is it efficient over Radiation Delivery at Discrete Angles with a Fixed Gantry?
Akkineni Naga Prasanthi1, Lakshmi Venkataramana Puriparthi2*, Anil Kumar Talluri2, Nagarjuna Reddy Bomidika3, Madhusudhana Sresty4 and Krishnam Raju Alluri5
1Consultant Radiation Oncologist, Department of Radiation Oncology, Basavatarakam Indo American Cancer Hospital and RI, India
2Sr. Medical Physicist, Department of Radiation Physics, Basavatarakam Indo American Cancer Hospital and RI, India
3Sr.Consultant Radiation Oncologist, Department of Radiation Oncology, Basavatarakam Indo American Cancer Hospital and RI, India
4Head of Radiation Physics, Department of Radiation Physics, Basavatarakam Indo American Cancer Hospital and RI, India
Submission: June 15, 2022; Published: July 07, 2022
*Corresponding Address: Lakshmi Venkataramana Puriparthi, Sr. Medical Physicist, Department of Radiation Physics, Basavatarakam Indo American Cancer Hospital and RI, Hyderabad, India
How to cite this article: Akkineni N P, Lakshmi V P, Anil K T, Nagarjuna Reddy B. Treatment Delivery within a Helical Geometry in Whole-Breast Radiotherapy on Tomotherapy Machine: is it efficient over Radiation Delivery at Discrete Angles with a Fixed Gantry?. Canc Therapy & Oncol Int J. 2022; 21(5): 556074. DOI:10.19080/CTOIJ.2022.21.556074
Abstract
Introduction: After breast-conserving surgery (BCS), the common site of recurrence is the conserved breast. Adjuvant radiotherapy is an important part of the treatment of breast cancer. Tomotherapy delivers intensity - modulated radiation therapy (IMRT) with better dosimetry and onboard mega voltage computed tomography(MVCT) imaging. A Study comparing tomohelical (TH) and tomodirect (TD) showed both produce acceptable dose coverage in chest wall RT. To our knowledge data evaluating helical tomotherapy technique in comparison to direct technique especially in whole-breast radiotherapy without nodal irradiation is limited. The present study aims to analyse the effect of TH technique with comparison to TD technique in left breast cancer patients requiring breast radiotherapy without nodal irradiation after BCS.
Material and Methods: This is a single institute observational study. Twenty left breast cancer patients were included. Patients were immobilized and underwent planning CT scans. Target volumes and organs at risk were delineated by the same radiation oncologist. TD IMRT and TH IMRT plans were generated to whole-breast by the same medical physicist, a dose of 50 Gy in 25 fractions.
Results: Results showed that the conformity index was better with the TH IMRT. In contrast, the homogeneity index was better with TD IMRT. Dose to the patient’s body registered high in TH IMRT. The volumes receiving 5Gy, 10 Gy, 20 Gy, and 30 Gy(V5, V10, V20 and V30) were analyzed and found variations were significant. In addition, Heart and ipsilateral lung doses were significantly low in TD IMRT. Mean dose to contralateral lung, contralateral breast, and esophagus also favourable to TD IMRT.
Conclusion: TH IMRT provides better dose conformity. But the body’s low dose volumes are high and less dose homogeneity with TH IMRT. TD IMRT provides good protection for OARs.
Keywords: Tomodirect IMRT; Tomohelical IMRT; Whole-breast radiotherapy; Left breast cancer
Introduction
After breast-conserving surgery (BCS), a common site of local recurrence is the conserved breast itself. Adjuvant whole-breast radiation therapy (WBRT) is an essential part of the standard multimodality treatment in early-stage breast cancer patients [1]. Conventional breast radiotherapy is based on two opposing tangential beams, resulting in high dose heterogeneity [2]. Intensity - modulated radiation therapy (IMRT) has been shown to improve dose homogeneity and to reduced dose to organs at risk (OAR) [3]. Tomotherapy delivers IMRT with a better dose homogeneity in the target volume, with reduced doses to organs at risk [4], and a precise patient set-up using the onboard megavoltage computed tomography (MVCT) system. Helical tomotherapy or tomohelical (TH)) is a technique to treat as the patient advances through the ring gantry slowly while a linear accelerator (LINAC) rotates around the patient and a binary multileaf collimator (MLC) with fixed fan beam width for fluence modulation allowing dose escalation to target and sparing of organs at risk (OAR) for various types of cancer. Tomodirect (TD) is a fixed beam mode allowing for planning and delivery at static beams, with the couch moving at a constant speed. TD IMRT appeared to give better dose distribution for WBRT compared to Tomodirect 3-dimensional conformal radiation therapy (3DCRT) with low toxicity and acceptable tumour control [5]. Dosimetric studies of TH in breast cancer showed an improvement in target dose homogeneity, conformity, and reduction in high doses of organs at risk compared to standard techniques [6-8].
The IMRT helical plan can improve the target coverage and reduces the dose to certain OARs compared to the 3D helical plan [9]. A Dosimetric study comparing TH and TD IMRT plans showed both produced acceptable target dose coverage in chest wall RT. Considering the risk of low dose to the critical organs; the TD plan improves dose distribution [10]. Studies comparing TH IMRT with TD IMRT techniques are available in the setting of post mastectomy radiotherapy, bilateral breast cancer, and unilateral breast radiotherapy with nodal irradiation. Data comparing TH IMRT with TD IMRT technique in whole-breast radiotherapy without regional nodal irradiation is limited. This study aims to evaluate tomohelical technique dosimetrically in early stage left breast cancer patients requiring radiation to the whole-breast without nodal irradiation after breast conservative surgery.
Material and Methods
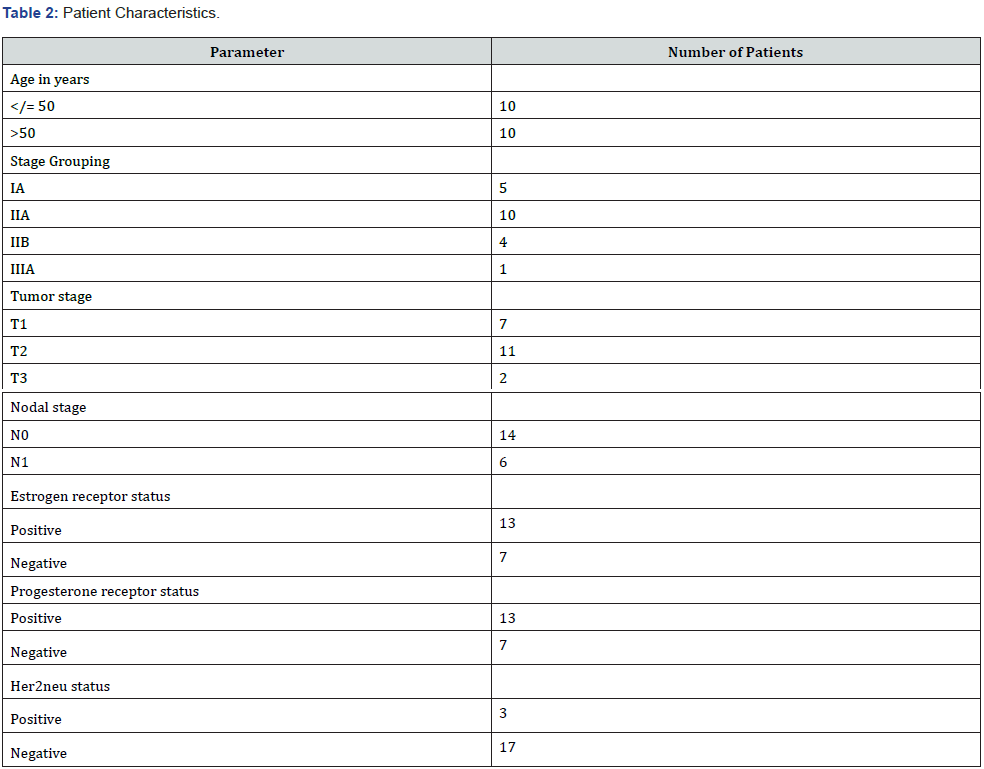
Single Institute observational study done over a period of 12 months from February 2020 to February 2021, and included female left breast cancer patients who were treated with whole breast radiotherapy. Primary objective is to analyse target volume coverage with tomohelical technique in comparison to tomodirect technique. Secondary objective is to analyse OAR doses with tomohelical technique. Patient inclusion criteria consists of females of age ranged from 20 years to 80 years with tumour stages I, II and IIIA (T3N1M0). All included patients underwent whole-breast adjuvant radiation therapy with or without adjuvant chemotherapy. The patients excluded from the study were who had recurrent breast cancer, received radiation therapy to breast previously, and bilateral breast cancer patients. In addition, left breast cancer patients with tumor staging IIIA (with N2 disease), IIIB, IIIC, and IV as well as right breast cancer patients were also excluded.
Radiotherapy Planning
Twenty left breast cancer patients were included for this study. Patients were positioned using a breast board with their head turned towards contralateral side and ipsilateral arm raised above their head in the supine position. The Brilliance computed tomography (CT) Big Bore (Philips Healthcare, Cleveland, OH) was used to scan patients with a slice thickness of 5mm and axial images were exported to the Eclipse treatment planning system of version 15.6.8(Varian Medical System, USA). Target volumes and OARs were delineated by the same radiation oncologist as per RTOG contouring guidelines [11]. Axial CT images along with structure set were exported to TomoHTM planning station of version 5.1.1.6 (Accuray, Sunnyvale, CA) for planning. Both TD IMRT and TH IMRT plans were generated by the same medical physicist with prescription Dose of 50 Gy in 25 fractions to whole breast for each patient.
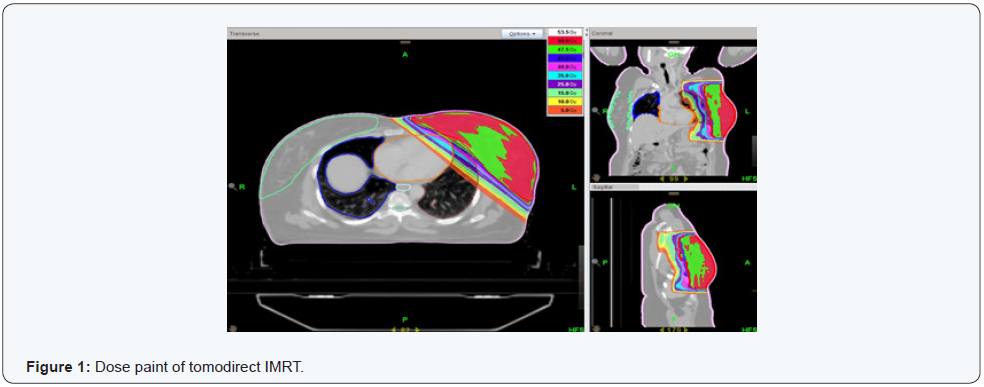
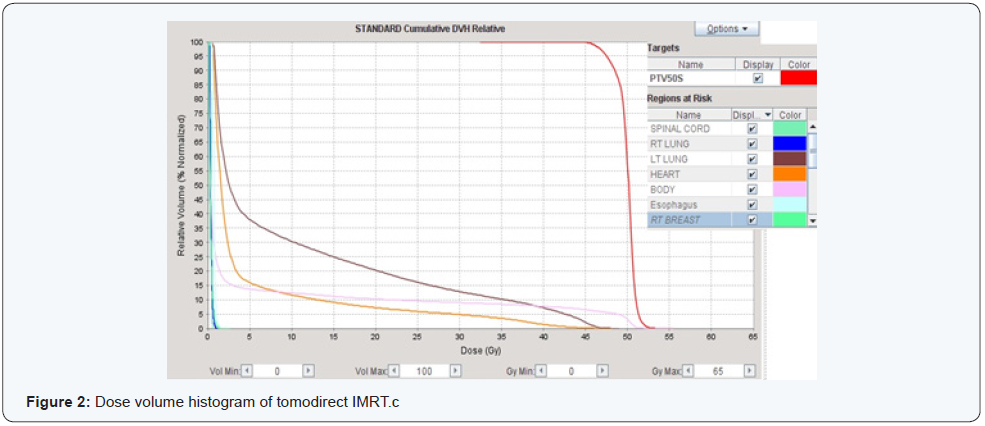
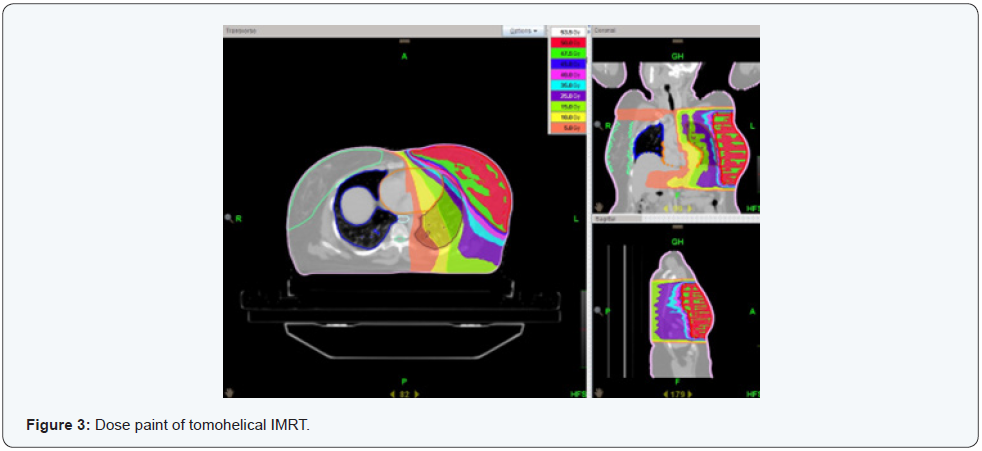
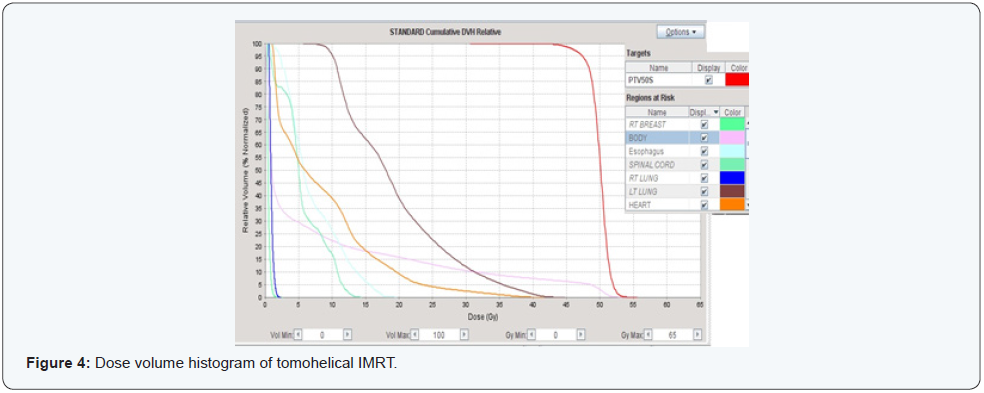
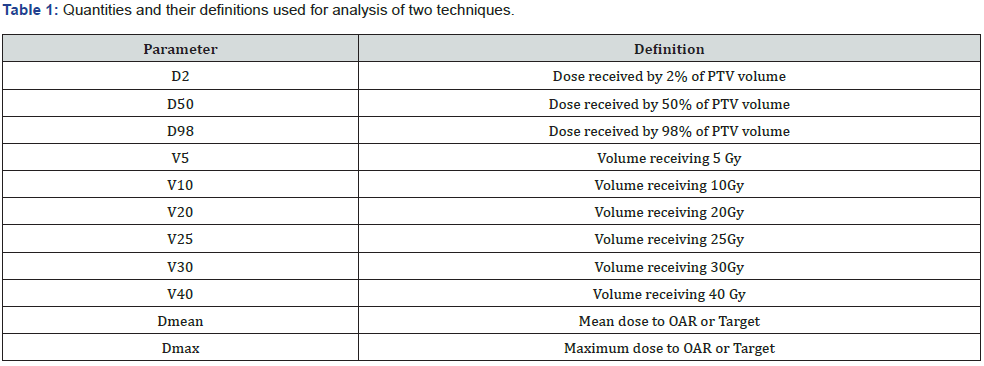
TD plans were generated by using multiple tangential fields. Beam angles of tangential fields were modified for each patient to cover planning target volume (PTV) appropriately and to reduce OAR doses. Plan parameters of pitch 0.5, modulation factor of 2, and field width– of 5.048 cm were considered for all twenty patients. Figure 1 shows dose coverage with TD IMRT plan and Figure 2 corresponding dose volume histogram (DVH). TH plans were generated with following plan parameters like TD IMRT of pitch 0.5, modulation factor 2 and field width 5.048 cm. As the LINAC rotates around the patient during beam delivery, right lung and right breast were blocked completely and spinal cord directionally to reduce doses. Figure 3 shows dose coverage with TH IMRT plan and Figure 4 corresponding DVH. Plan acceptance was based on International Commission on Radiation Units and Measurements (ICRU) report number 83 guidelines [12]. DVH of both TH IMRT and TD IMRT plans were analysed dosimetrically for each patient. Table 1 summarizes quantities and their definitions used for analysis and comparison of plans.
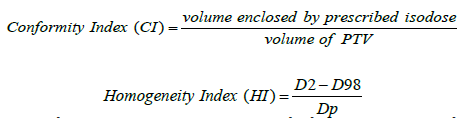
Quantities such as conformity index (CI) and homogeneity index (HI) were used to find the plan quality which could be calculated from following equations where D2 and D98 are doses received by 2% and 98 % of PTV volumes respectively, and Dp is prescribed dose.
PTV dose coverage parameters which were compared between TH and TD IMRT plans are D50 (dose received by 50 percent of PTV volume), D98 (dose received by 98 percent of PTV volume), D2 (dose received by 2 percent of PTV volume), CI, and HI. Volumes of the patient’s body receiving different level of doses, 5 Gy, 10 Gy, 20 Gy, 30 Gy, and 40 Gy (V5, V10, V20, V30, and V40) were also compared. For heart, the volumes receiving more than 10Gy, 25 Gy (V10, V25), and Dmean were compared. For contralateral lung, contralateral breast and esophagus mean dose, and for spinal cord max dose was compared. In case of ipsilateral lung V5, V20, V30, and mean dose were considered. In addition, treatment time which is important factor also evaluated between two techniques.
Statistical Analysis
Kolmogorov-Smirnov test was used to find normal distribution of data. Student’s t - test and Mann-Whitney U test were used to find statistical significance of differences between two techniques. Differences were considered significant for p value less than 0.05.
Results
Patient characteristics
Table 2 highlights the patient and tumour characteristics of the twenty patients who were enrolled in the current study. Of note, the median age was 50 years (range from 31 years to 71 years). Most common stage was stage II A (50%) followed by stage IA (25%).
Target dose – volume parameters
Results showed that conformity index was better for TH IMRT technique as compared to TD IMRT. Mean CI was 1.06 ± 0.06 and 1.10 ± 0.06 (p = 0.006) for TH IMRT and TD IMRT respectively. Homogeneity index was best achieved with TD IMRT technique. Mean HI was 0.15± 0.04 in TH IMRT whereas 0.10± 0.02 in TD IMRT (P <0.001). D98 and D2 were better with TD IMRT as compared to TH IMRT, mean dose of 46.3Gy± 0.93Gy, 51.2Gy ± 0.34Gy and 45.2Gy ± 1.5Gy, 52.6Gy ± 0.34Gy were registered respectively. There was no considerable difference in mean D50 between two techniques, Table 3 summarizes the results. The patient’s body showed remarkable difference in 5 Gy dose volumes (V5) between two techniques. Mean V5 were 20.5% ± 5.6% and 9.9% ± 1.9% (p <0.001) for TD IMRT and TH IMRT respectively. Similar results were observed for mean volumes of V10, V20, and V30. However, V40 showed no considerable difference, Table 3 summarizes results. It was observed that treatment time was shorter for TD IMRT as compared to TH IMRT, 4.30 minute ± 0.42 minute and 5.35 minute ± 0.37minute respectively (p < 0.001).
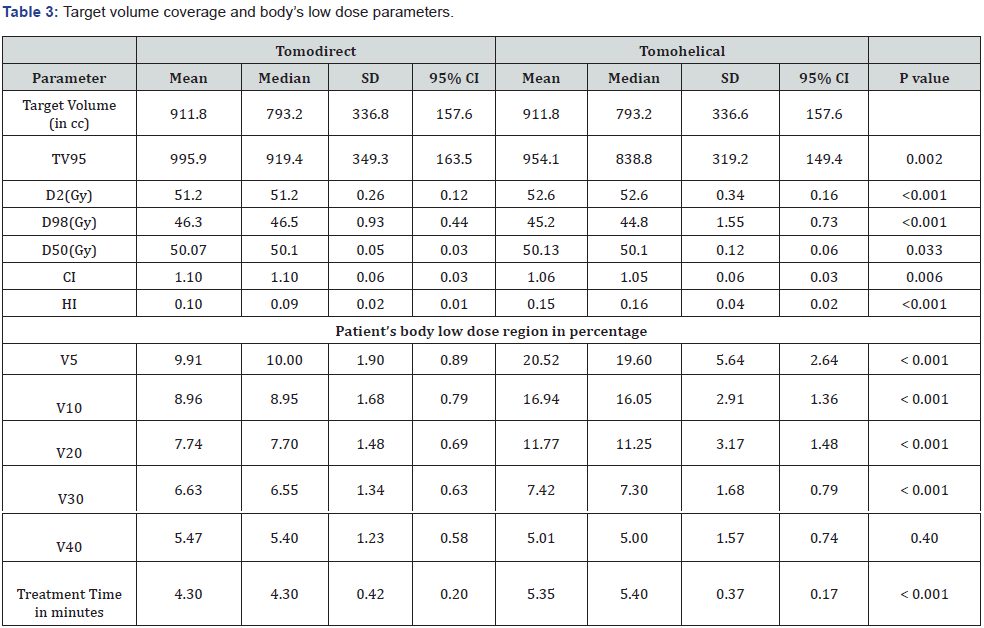
CC = centimetre cube; D2 = dose received by 2% volume; D98 = dose received by 98% volume; D50 = dose received by 50% volume; CI = Conformity Index; HI = Homogeneity Index; V5 volume receiving 5 Gy; V10 volume receiving 10 Gy; V20 volume receiving 20 Gy; V30 volume receiving 30 Gy; V40 volume receiving 40 Gy; 95% CI = 95% Confidence Interval; SD = Standard Deviation.
Organs at risk dose - volume parameters
Results showed that heart dose was substantially less for TD IMRT, the mean doses were 5Gy ± 1.27Gy and 9.2Gy ± 1.8Gy (p < 0.001) for TD IMRT and TH IMRT techniques respectively. The mean volume of the heart receiving 10 Gy was 2.84 times higher for TH IMRT as compared to TD IMRT. However, the difference was very narrow for 25 Gy volume, close to absolute difference of 1%. Similarly, the ipsilateral lung also registered low dose for TD IMRT as compared to TH IMRT. The mean Dmean were 8.8Gy ± 2.04Gy and18.4Gy ± 2.06Gy (p < 0.001) for TD IMRT and TH IMRT techniques respectively, and volumes receiving 5 Gy and 20 Gy were 3.3 and 2 times low for TD IMRT. However, volume receiving 30 Gy did not show significant difference. The contralateral lung mean dose was significantly less for TD IMRT compared to TH IMRT technique, 0.31Gy ± 0.08Gy and 0.68Gy± 0.14Gy(P <0.001) respectively. The contralateral breast mean dose was significantly low for TD IMRT technique by 33% compared to TH IMRT technique. The spinal cord mean Dmax was less in TD IMRT (0.48Gy±0.13Gy) compared to TH IMRT technique (16Gy± 3.7Gy) with P value <0.001. The esophagus mean Dmean was significantly less in TD IMRT (0.04Gy ± 0.18Gy) compared to TH IMRT technique (39Gy± 19.2Gy) with P value <0.001. Table 4 summarizes dose to critical OARs.
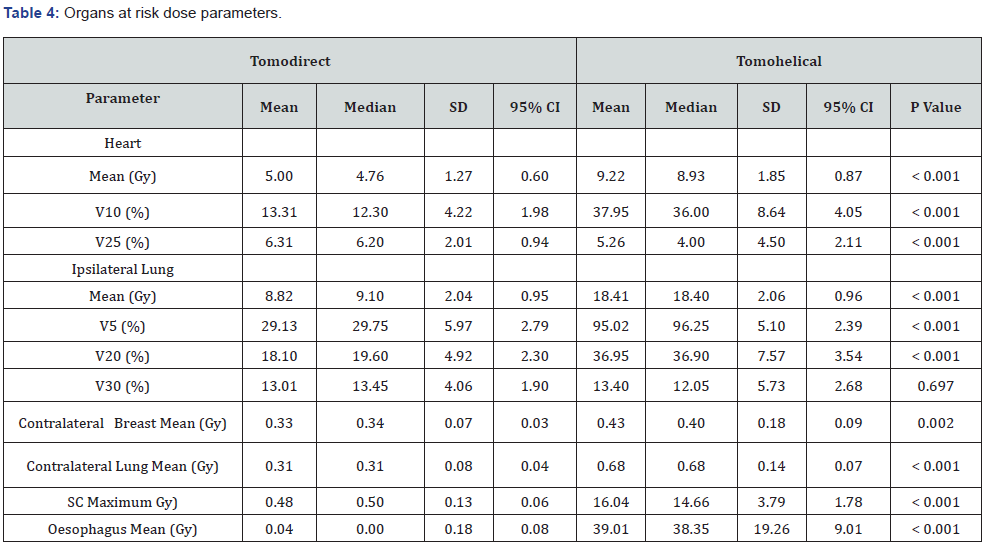
V5 volume receiving 5 Gy; V10 volume receiving 10 Gy; V20 volume receiving 20 Gy; V25 volume receiving 25Gy; V30 volume receiving 30 Gy; 95% CI = 95% Confidence Interval; SD = Standard Deviation; SC = Spinal Cord.
OAR: Organ at risk; PTV: Planning Target Volume
Discussion
In the present study, we analysed different tomotherapy techniques dosimetrically (direct and helical IMRT) for wholebreast radiotherapy to evaluate the effect of treatment delivery within a helical geometry for each patient’s condition from multiparameter comparison results. Tomohelical often offers superior results over tomodirect technique. In a series of 14 patients with bilateral breast cancer, Ekici and colleagues showed that helical tomotherapy was well-tolerated with high homogeneity and coverage indexes and low doses to the lungs and heart [13]. Study by Wadasadawala and colleagues showed that helical tomotherapy provided better target coverage and more homogeneous dose distribution than direct tomotherapy in treatment of synchronous bilateral breast cancer patients [14]. In a case report of bilateral synchronous stage 1 and grade 1 breast cancer patients, helical tomotherapy appeared to be more suitable than direct tomotherapy, providing better planning target volume coverage with higher D90%, D95%, D98%, and Dmean and a lower homogeneity index. No hot spots were seen with both techniques. Helical tomotherapy and direct tomotherapy showed similar dosimetric results for OARs, but the left lung V4Gy and all spinal cord parameters were better with direct tomotherapy plan. Helical tomotherapy was better for RVR V100% [15]. Regarding the Unilateral whole breast irradiation, Clinical results from both helical IMRT and helical 3D plans are acceptable in target volume coverage and dose to OAR. Even though IMRT helical planning is superior to 3D helical planning in improving the target coverage and reduction in OAR doses, acceptable and high-quality plans can be generated by using 3D helical, when treatment using helical IMRT is not an option [9].
Studies particularly comparing tomodirect IMRT and tomohelical IMRT in unilateral breast cancer patients who required whole-breast radiation therapy without nodal irradiation are very limited. To our knowledge, turkish study by Erdiş et al. [16] is the only study till date which compared tomohelical IMRT and tomodirect IMRT during intact breast irradiation in patients with negative lymph nodes and showed better dose distribution with tomohelical and tomodirect IMRT. Conformity index was similar in both helical and direct plans, but homogeneity index was best achieved with tomohelical IMRT. Low dose volumes were high with tomohelical IMRT and it showed lower ipsilateral lung and heart doses in breast irradiation but showed an increase in contralateral breast dose and for right breast irradiation it causes an increase in heart dose. Nobnop W et al. [17] studied tomohelical IMRT and tomodirect IMRT for post mastectomy patients showed that helical tomotherapy plans showed to be superior in target coverage, homogeneity index, and conformity index for all situations of chest wall and regional node treatment.
Tomodirect plans showed significantly lower doses for contralateral lung, breast, and spinal cord in all situations of patient treatments. Helical tomotherapy plans showed lower dose for ipsilateral lung. Another study by F Teke et al. [10] in patients treated with chest wall irradiation showed that tomodirect and tomohelical IMRT plans have similar conformity and homogeneity for target. However, considering larger low-dose radiation regions on normal tissue which can cause increased risk of secondary malignancies, heart, and lung disease, the tomodirect technique can give similar dose distribution and better protection of critical organs during chest wall irradiation. More importantly, the total treatment time is considerable low for the tomodirect technique as compared to the tomohelical technique. However, total treatment delivery time may change as tomodirect technique involves multiple times couch movement of in and out into the machine bore to deliver multiple direct beams. Samantha Dicuonzo et al. [18] studied tomohelical IMRT and tomodirect IMRT in the setting of hypo fractionated post mastectomy radiotherapy with immediate breast reconstruction and showed that tomodirect plan reached acceptable target volume coverage, with an optimal sparing of OARs. Shoko Takano et al. [19] compared tomodirect with tomohelical techniques in left breast cancer patients received radiation therapy to chest wall/residual breast tissue and level II–III axial and supraclavicular lymph node area. They showed that tomodirect can provide better target dose distribution with optimal normal-organ sparing.
To our best knowledge, present study is the first study evaluating tomohelical technique in comparison to tomodirect technique specifically in unilateral (left) breast cancer patients who were treated with whole-breast radiotherapy without lymph nodal irradiation in Indian setting. In the present study results showed that left breast cancer patients who underwent breast conservation surgery and treated with adjuvant radiotherapy to whole-breast, conformity is better for the tomohelical as compared to the tomodirect technique which is in good agreement with other studies [17]. However, homogeneity was best achieved with the tomodirect IMRT technique which is opposite with previous studies [16,17]. Considering the risk of secondary malignancies increased with low dose volumes, tomodirect technique resulted in producing less low dose volumes as compared to tomohelical which is in good agreement with other studies [10,16]. The patient’s body receiving 5 Gy is reduced by 50% for the tomodirect as compared to the tomohelical technique. However, the difference reduced gradually for 10 Gy, 20 Gy, and 30 Gy volumes, and no considerable difference at 40 Gy volumes.
In this study heart mean dose is significantly lower in the tomodirect IMRT as compared to the tomohelical IMRT. This finding is in good agreement with previous studies [10,16,17]. Volume receiving 10 Gy is 38% for the tomohelical IMRT technique against 13.3% for the tomodirect IMRT technique. Option of selection of suitable gantry angles with the tomodirect IMRT technique could be the reason for the observed difference whereas for the tomohelical IMRT technique such a provision is not available. However, Heart V25 found to be not in agreement with previous studies [10,16], and observed difference is minimal. Similar to previous studies [10], the present study showed ipsilateral lung mean dose, V20, and V5 are found to be significantly low in the tomodirect IMRT technique. The increase in low dose volume for the tomohelical IMRT technique is due to increased exposure of large volume to helical beam. Similar to study by Erdis et al. [16], contralateral lung registered less dose with the tomodirect IMRT technique. We found less Contralateral breast mean dose with the tomodirect IMRT technique which is on similar lines with previous studies [10,16,17]. Higher dose to contralateral breast in the tomohelical IMRT technique could be resulted from increased scattered radiation in spite of application of a complete beam block. Similar to other studies [10,17], spinal cord and esophagus doses are significantly low in the tomodirect IMRT technique as compared to the tomohelical IMRT technique. Main limitation of this study is that clinical effects of the dosimetric findings of different tomotherpy techniques were not evaluated. Patients treated with different tomotherapy techniques need to be followed up clinically for an appropriate time to assess for the difference in locoregional control and toxicity.
Conclusion
Compared to the tomodirect IMRT technique, it is possible to achieve better dose conformity with the tomohelical IMRT technique. However, the body’s low dose volumes are high and less target dose homogeneity with the tomohelical IMRT technique. For critical organs at risk, tomodirect planning provides good protection. Treatment time is promisingly low for the tomodirect IMRT technique. Considering the risk of secondary malignancies, normal tissue toxicities the tomodirect IMRT is the preferable technique.
References
- Clarke M, Collins R, Darby S, et al. (2005) Early Breast Cancer Trialists Collaborative Group. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomized trials. The Lancet 366(9503): 2087–2106.
- Barnett G, Wilkinson J, Moody A, Wilson C, Sharma R, et al. (2009) A randomised controlled trial of forward-planned radiotherapy (IMRT) for early breast cancer: Baseline characteristics and dosimetry results. Radiotherapy and Oncology 92(1): 34-41.
- Kestin L, Sharpe M, Frazier R, Vicini F, Yan D, et al. (2000) Intensity modulation to improve dose uniformity with tangential breast radiotherapy: Initial clinical experience. International Journal of Radiation Oncology Biology Physics 48(5): 1559-1568.
- Coon A, Dickler A, Kirk M, Liao Y, Shah A, et al. (2010) Tomotherapy and Multifield Intensity-Modulated Radiotherapy Planning Reduce Cardiac Doses in Left-Sided Breast Cancer Patients WithUnfavorable Cardiac Anatomy. Int J Radiat Oncol Biol Phys 78(1): 104-110.
- Nagai A, Shibamoto Y, Yoshida M, Inoda K, Kikuchi Y (2017) Intensity-modulated radiotherapy using two static ports of tomotherapy for breast cancer after conservative surgery: dosimetric comparison with other treatment methods and 3-year clinical results. Journal of Radiation Research 58(4): 529-536.
- Caudrelier J, Morgan S, Montgomery L, Lacelle M, Nyiri B, et al. (2009) Helical tomotherapy for locoregional irradiation including the internal mammary chain in left-sided breast cancer: Dosimetric evaluation. Radiotherapy and Oncology 90(1): 99-105.
- Goddu S, Chaudhari S, Mamalui-Hunter M, Pechenaya O, Pratt D, et al. (2009) Helical Tomotherapy Planning for Left-Sided Breast Cancer Patients with Positive Lymph Nodes: Comparison to Conventional Multiport Breast Technique. Int J Radiat Oncol Biol Phys 73(4): 1243-1251.
- Lauche O, Kirova Y (2014) Helical tomotherapy in breast cancer treatment. Breast Cancer Management 3(5): 441-449.
- Yadav P, Yan Y, Ignatowski T, Olson A (2017) Dosimetric aspects of breast radiotherapy with three-dimensional and intensity-modulated radiotherapy helical tomotherapy planning modules. Medical Dosimetry 42(1): 42-46.
- F Teke, M H Dogan, M A Kaya, M Gumus (2017) Dosimetric comparison of TomoDirect and TomoHelical plans in post-mastectomy chest wall radiation therapy. Int J Radiat Res 15(3): 259-266.
- Li X, Arthur D, Buchholz T, MacDonald S, Marks L, et al. (2007) Variability of Target and Normal Structure Delineation for Breast-Cancer Radiotherapy: A RTOG Multi-Institutional and Multi-Observer Study. International Journal of Radiation Oncology Biology Physics 69(3): S72-S73.
- The International Commission on Radiation Units and Measurements (2010) Report 83. Journal of the ICRU 10(1): NP.1-NP.
- Ekici K, Gokce T, Karadogan I, Aysun Fatma Eraslan, Cimen Akcay, et al. (2016) Is helical tomotherapy-based intensity-modulated radiotherapy feasible and effective in bilateral synchronous breast cancer? A two-center experience. J BUON 21(1): 46–52.
- Wadasadawala T, Visariya B, Sarin R, Upreti R, Paul S, et al. (2015) Use of tomotherapy in treatment of synchronous bilateral breast cancer: dosimetric comparison study. Br J Radiol 88(1048): 20140612.
- Lancellotta V, Iacco M, Perrucci E, Zucchetti C, Dipilato A, et al. (2017) Comparison of Helical Tomotherapy and Direct Tomotherapy in Bilateral Whole Breast Irradiation in a Case of Bilateral Synchronous Grade 1 and Stage 1 Breast Cancer. American Journal of Case Reports 18: 1020-1023.
- Erdiş e, Birsen Yücel, Betül Özyürek, Recep Bozca (2020) The Comparison of Helical-IMRT, Direct-IMRT and 3D Radiotherapy Modalities in Breast Radiotherapy Planning. Turkish Journal of Oncology 35(3): 257–265.
- Nobnop W, Phakoetsuk P, Chitapanarux I, Tippanya D, Khamchompoo D (2020) Dosimetric comparison of TomoDirect, helical tomotherapy, and volumetric modulated arc therapy for postmastectomy treatment. J Appl Clin Med Phys 21(9): 155-162.
- Dicuonzo S, Patti F, Luraschi R, Frassoni S, Rojas D, et al. (2021) Comparing TomoHelical and TomoDirect in postmastectomy hypofractionated radiotherapy after immediate breast reconstruction. Physica Medica 90: 66-72.
- Takano S, Omura M, Suzuki R, Tayama Y, Matsui K, et al. (2019) Intensity-modulated radiation therapy using TomoDirect for postoperative radiation of left-sided breast cancer including lymph node area: comparison with TomoHelical and three-dimensional conformal radiation therapy. Journal of Radiation Research 60(5): 694-704.






























