Case Report: Epithelioid Hemangioma of Distal Femur
Abdullah Alhazmi1, Dhafer Almuffarh1, Sulaiman Hushlul2, Faisal Alrefaei3*, Albara’a Alsubahi4, and Ahmad Kaneetah4
1Orthopedic Consultant at King Abdulaziz Medical City, Jeddah, KSA
2Orthopedic resident at King Abdullah Medical City, Makkah, KSA
3Orthopedic resident at King Fahad general hospital, Jeddah, KSA
4Orthopedic resident at King Abdulaziz Medical City, Jeddah, KSA
Submission: January 02, 2022; Published: January 12, 2022
*Corresponding Address: Faisal Alrefaei, Orthopedic resident at King Fahad general hospital, Jeddah, KSA
How to cite this article: Abdullah A, Dhafer A, Sulaiman H, Faisal A, Albara’a A, et al. Case Report: Epithelioid Hemangioma of Distal Femur. Canc Therapy & Oncol Int J. 2022; 20(4): 556042. DOI:10.19080/CTOIJ.2022.20.556042
Abstract
Background: Epithelioid hemangioma (EH) is a rare benign vascular lesion of soft tissue and bone, characterized by endothelial cells with epithelioid or histiocytoid appearance. Though tubular bones, flat bones, vertebra and short bones are common sites for this lesion, the epiphyseal involvement is extremely rare. We present an unusual case of EH of the distal femur in a young female.
Report: A 22-year-old lady medically free presented to the clinic complaining of mild left knee pain for one year, on physical examination revealed limping and muscular atrophy of the left lower limb and a moderately tender swelling in the medial aspect of the left knee without restriction of knee movement. An X-ray revealed an osteolytic lesion, which appeared iso- and hypointense on T1W and hyperintense on T2W MRI images in the distal left femur. A radiological diagnosis of chondroblastoma was entertained. The patient was treated with curettage and bone grafting. Histopathology showed a tumor composed of thin-walled arteriolar capillaries lined by large, polyhedral epithelioid endothelial cells with vesicular nuclei, finely distributed nuclear chromatin, and moderate amount of eosinophilic cytoplasm. diagnosis of EH was made. EH is a benign lesion and it should be differentiated from its histologically similar malignant counterparts such as epithelioid hemangioendothelioma and epithelioid angiosarcoma as the lesion can be successfully treated with curettage or resection.
Keywords: Epithelioid hemangioma; Congenital talipes equinovarus; Chondroblastoma; Femoral epiphysis
Introduction
Epithelioid hemangioma (EH) is an uncommon benign vascular tumor, which was first described by Wells & Whimster in 1969 [1]. It is usually found in the dermis, subcutis, lymph nodes, and rarely in visceral organs [2-4]. The tumor typically occurs during early adulthood and is more common in women [5]. Osseous epithelioid hemangiomas are rare and may occur in any bone [6]. Rarely it can be multifocal involving multiple bones and extra skeletal tissues [6]. Some authors believe that osseous EH is a variant of hemangioendothelioma, which has malignant potential [7]. However, clinical and radiological features, and follow-up studies suggest that it is a benign lesion [6]. The common sites of osseous EH are long and short tubular bones, flat bones, vertebra and small bones of hands [4]. The epiphysis, however, is an unusual site for this lesion. We present a case of EH of the distal femur in a young female.
Case Presentation
A 22-year-old female presented with a history of progressively increasing pain in the left lower thigh for 12 months. There was no history of trauma, fever, cough, night sweat or weight loss. Physical examination revealed atrophy of muscles of the left lower limb and a moderately tender swelling in the medial aspect of the left knee. There was no restriction of knee movement. Examination of the other systems was unremarkable. An X-ray of the left lower thigh (Figure1) showed an osteolytic lesion in the distal left femur. Chest X-ray, complete blood count and erythrocyte sedimentation rate (ESR) were within normal limits. Magnetic resonance imaging (MRI) scan (Figure 2) revealed: a large multilobulated multifocal mass noted at the distal femur involving the metadiaphysis and patella, articular surface of lateral condyle and small focus noted at the proximal posterior tibia, it demonstrates low T1 signal intensity and heterogeneous high signal intensity in STIR images with avid enhancement in post contrast images with areas of necrosis. The mass causing large medial cortical destruction with soft tissue extension involving the vastus medialis muscle as well as extension to the lateral tenaculum.

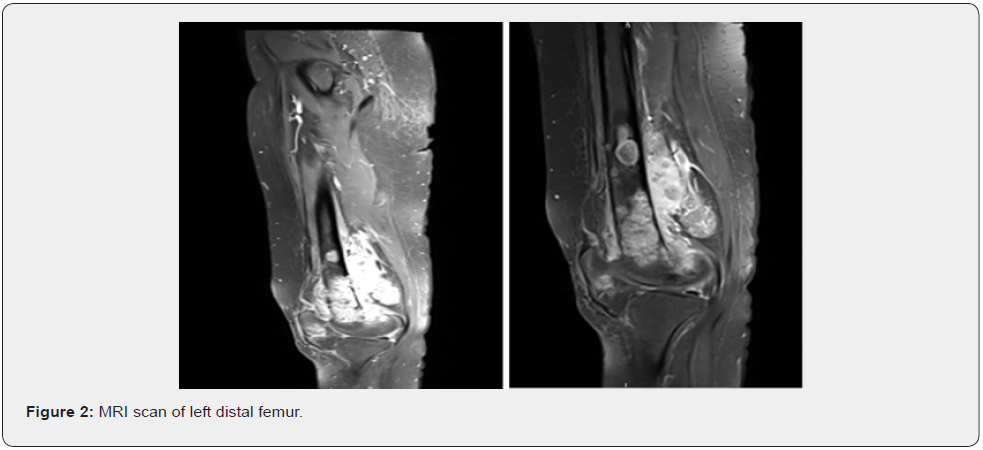
The mass is abutting the neurovascular bundle, however there is no clear extension. The mass is measuring around 6 x 12 cm in transverse and CC dimension. There are two small lesions noted at the articular surface of lateral condyle and proximal tibia posteriorly. They are measuring around 1 x 0.8 cm. They are representing similar signal intensity to the primary mass, however there is no matching abnormality seen in the bone scan or in the X-ray. Large popliteal lymph node is noted measuring 3 x 2 cm. Extensive lymphadenopathies are noted at the left group, inguinal and femoral, the largest is noted at the iliac region measures around 2.4 x 3.4 cm. Extensive surrounding soft tissue edema with post gad enhancement is noted. Impression: Aggressive bony lesion of the left distal femur as described likely representing sarcoma for histopathological correlation.
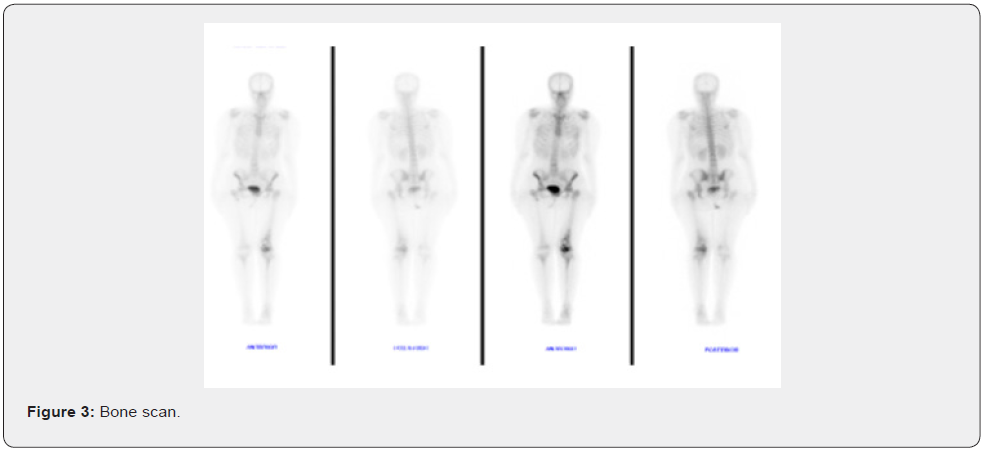
Bone scan (Figure 3) showed: abnormal heterogeneous uptake involving the distal one third of the left femur with multiple areas of photopenia. A small, rounded focus is seen overlying the right upper thigh likely representing a contamination. No other focal abnormality is seen in the rest of the skeleton. The right hemipelvis is relatively small. Impression: distal left femur pathology under investigation, no evidence of multiplicity or distant active bone metastases.
CT Angio reported as: The bilateral common iliac, external iliac, common femoral, superficial femoral, popliteal, anterior tibial, posterior tibial and peroneal arteries are patent. No significant interval changes are noted regarding the left distal femoral lesion, multiple perilesional and left inguinal lymph node enlargement. The solid organs appear unremarkable in an arterially enhanced study. The lungs appear unremarkable.
CT scan of the abdomen and pelvis: The liver, spleen, pancreas, adrenals and kidneys are homogeneously enhancing with no focal lesions. No free air. Mild physiologic free fluid is noted. Bowel is unremarkable. The previously noted left inguinal, external iliac, common iliac and para-aortic lymph nodes show interval increase in size - left inguinal lymph node is measuring in the current exam 1.1 cm and was 0.9 cm in maximum cross-sectional diameter. The left external and middle ear. His measuring 1.8 cm in greatest diameter and was around 1.6 cm in greatest diameters]. No neurologic lesions detected. Visualized bones show no suspicious bony lesions. Impression: Patient is known case of the femoral sarcoma with interval increase in the left inguinal, pelvic and para-aortic lymph node metastasis.
Patient then presented with slowly growing painful mass in the left distal femur, imaging and biopsy done which reported as epithelioid hemangioma with multiple pelvic and paraaortic lymph nodes. biopsy taken from the lymph nodes and reported similar pathology. The case was discussed in the tumor board twice and since there is no evidence of any malignant changes the plan was not to give any systemic therapy and proceed with surgical resection.
Left distal femur biopsy which consists of twelve separate loose strips of grayish-brown, thin cores of soft tissue of variable length measuring from 0.5 x0.1 x 0.1 cm up to 2 x 0.2 x 0.2 cm. Four cores submitted in each block. Microscopic Description Sections show cores of biopsy tissue with involvement by vascularized lesions with focal areas of necrosis. There is a predominant vascular pattern lined by epithelioid to spindle cells with round nucleoli and prominent nucleoli and moderate eosinophilic cytoplasm (hob-nail pattern). Another part of the biopsy there is a portion of trabeculae and sheets of epithelioid cells with nuclear monomorphism, vesicular chromatin, inconspicuous nuclei, nuclear groups. There is intense background infiltration by eosinophils. Focal aggregates of lymphoid cells are noted. Scattered fragments show germinal center formation around blood vessels. Immunohistochemistry: Endothelial cells are positive for ERG, CD34, CD31 and show focal positivity for CKAE1/AE3, while CD1a and S100 are both negative.
Left inguinal lymph node biopsy done consists of six elongated strips of thin, slender cores of grayish-tan, soft tissue measuring 0.6 x 0.2 x 0.2cm up to 1.7x 0.2 x 0.2 cm. Three cores submitted in each block. Wrapped and all submitted in two blocks. Immunohistochemistry: Microscopic Description: Target cells: CD31++, CD34++, ERG++, CD3 and CD20 highlight background of reactive T and B cells. (All positive and negative controls are examined and show appropriate reactivity). Flow Results: WBC Count 23.6 x 10^3/uL. Viability: 85%. Flow ytometric analysis of lymphoid cells in the left inguinal lymph node shows around 52% mature T-cells with no aberrant loss or aberrant expression of -cell markers with CD4/CD8 ratio of 2.79, 1% NK cells and 45% polyclonal B-cells.
Procedure Details
Under general anaesthesia in supine position the leg was preped and draped in sterile fashion. a medial skin incision was done over the distal femur and extended anteriorly. dissection done down the facia and the fibres of the vastus medialise elevated off the posterior intermuscular fascia. the distal femur fully exposed and meticulous haemostasis insured. after that intralesional resection was done utilising currets and bur. found to have significant involvement of the distal femur with cortical breakthrough anteriorly and posteriorly. the lesion was thoroughly curettage and all lesion tissue sent for histopathology. after that the lesion was filled with bone cement and medial distal femoral locked plate applied and fixed with 4 distal and approximal locking screws.
C-arm was utilised to ensure proper filling of the defect and fixation was done in all views, after that we turned out attention to the patella and curettage of the lesion was done and found significant damage to the patella with only the articular surface was left with very thin shell cortical bone. the defect was then filled with cancellous bone chips and gently impacted, the wound was thoroughly irrigated and heamostatayses insured, at the time of closure there was no obvious bleeding, and the wound was closed in layers, and covered with sterile dressing and a long back slab. She was shifted to recovery where she was reviewed again and found to have normal vitals, intact distal pulses and was moving her toes.
Surgical Pathology Final Report
Diagnosis: consistent with epithelioid hemangioma
Discussion
Epithelioid hemangioma is a rare benign, slow growing vascular lesion that typically occurs in the head and distal extremities. The possible pathogenesis is benign vascular neoplasm or reactive process to a preceding trauma. It occurs in mid-adult life and is slow growing, with an average time between appearance and excision of four and a half months [8]. Osseous hemangiomas account for less than 1% of all primary bone tumors and most often involve vertebral bodies and calvarium [9]. Peripheral tubular bones and the ribs are infrequently affected [9]. The histopathological subtypes of osseous hemangiomas are cavernous, capillary, arteriovenous, venous and epithelioid variants [2]. Most of the solitary hemangiomas of bone are asymptomatic and diagnosed as an incidental finding on radiographs. Middle-aged patients are usually affected with a predilection for females [5]. Hemangioma of the tubular bone may be periosteal, intracortical, or medullary type which is further subdivided into the diaphyseal (48%), metadiaphyseal (30%), metaphyseal (12%), metaepiphyseal (4%), epimetadiaphyseal (3%) and epiphyseal type (1%) [10]. Epiphyseal or juxta-articular hemangiomas are rare [11]. Capillary and cavernous hemangiomas are the most common in bone, whereas EH, also known as histiocytic hemangioma, and angiolymphoid hyperplasia with eosinophilia is less common. The endothelial cells of EH are referred to as ‘histiocytoid’ because of their lobated nuclei, decreased alkaline phosphatase and increased acid phosphatase content compared to normal endothelium [5].
The etiology of EH remains unknown. Boudousquie et al reported that epithelioid hemangioendothelioma which is the lowgrade malignant counterpart of EH has a complex translocation between chromosome 7 and 22 [12]. Osseous EH should be distinguished from some histologically similar low grade malignant tumors like epithelioid hemangioendothelioma and epithelioid angiosarcoma [2,13]. Many of the tumors previously reported as low- grade hemangioendothelial sarcoma indeed represented EH [13]. Microscopically EH has lobular organization of capillaries lined by large polyhedral epithelioid endothelial cells with oval to bean shaped nuclei having fine chromatin. The cytoplasm is usually abundant and deeply eosinophilic. Occasional one or more round, clear spaces containing red blood cells are seen. The endothelial cells may be plump and intruding into the lumen like a tombstone [6]. As EH is a benign tumor, the cells have low mitotic index and absent cellular atypia [14].
Prominent inflammatory infiltrate including eosinophils, lymphocyte and plasma cells may be present. Occasionally a central parent vessel can be identified in the center of the lesion [2,6]. Epithelioid hemangioendothelioma on the other hand is a borderline malignant tumor with less vascular differentiation and a tendency to recur and metastasize. It is more often multifocal and tends to have a more aggressive clinical course. Unlike EH, in haemangioendothelioma the endothelial cells are usually arranged in cords and nests in a distinct myxohyaline or chondroid background without prominent inflammatory component. There is nuclear atypia, and the eosinophils are generally absent [15]. Epithelioid angiosarcoma is a malignant tumor, which usually shows larger cell size, larger, irregular nucleoli, higher nucleocytoplasmic ratio, greater mitotic activity and frequent necrosis [2,13]. It has a more aggressive clinical course than epithelioid hemangioendothelioma. Proliferation markers like Ki-67 labelling index will be higher in epithelioid hemangioendothelioma and angiosarcoma as against EH. In our case there was minimal cellular atypia with low mitotic index.
Radiologic examination classically demonstrates osteolytic lesion with or without surrounding sclerosis. MRI is helpful in evaluating osseous lesions. EH on T1-weighted MRI images shows areas of decreased signal intensity, while on T2-weighted images the vascular components demonstrate markedly hyperintense signal. Cortical expansion and cortical destruction have been described in rare cases [11]. T1-weighted image is based on relaxation properties of various protons thereby assessing the marrow involvement by the tumor, identifying fatty tissue, and hemorrhage. T2- weighted image is created based on decay properties of various protons in the body and is useful for detecting abnormalities like oedema, soft tissue component and skip lesions. The radiological differential diagnoses may be giant cell tumor, aneurysmal bone cyst, plasmacytoma, osteoblastoma, infection, benign vascular lesion etc [11,16]. The radiologic diagnosis of our case was chondroblastoma.
Nielsen et al reported 50 cases of osseous EH with ages ranging from 10 to 75 years with a mean of 35 year. Most of the lesions were in long and short tubular bones (58%), and 18% of patients had more than one bone involvement [6]. In our case there was a single lesion that involved the epiphysis, epiphyseal plate and adjacent metaphysis of the distal femur. The patient in addition had congenital talipes equinovarus, which is a poorly understood developmental disorder of the lower limb with fixation of the affected foot in adduction, supination and varus and concomitant soft tissue abnormalities. The coexistence of EH and talipes equinovarus in our case could be an incidental association. The patients with EH are treated with curettage or by local resection depending on the location and extent of the lesion [2]. Complications of this entity includes local recurrence though rare [5].
EH of bone is a distinct vascular tumor, which should be distinguished from epithelioid hemangioendothelioma and epithelioid angiosarcoma as it is a benign lesion which can be successfully treated with curettage or marginal en block resection.
References
- Wells GC, Whimster IW (1969) Subcutaneous angiolym- phoid hyperplasia with eosinophilia. Br J Dermatol 81(1): 1-14.
- Enzinger FM, Weiss SW (2008) Benign tumors and tu- morlike lesions of blood vessels. In: Enzinger FM, Weiss SW, editors. Soft tissue tumors. 5th St Louis: Mosby. p. 633-680.
- Ismail M, Damato S, Freeman A, Nigam R (2011) Epithelioid hemangioma of the penis: case report and review of literature. J Med Case Rep 5: 260.
- Fernandes BF, Al-Mujaini A, Petrogiannis-Haliotis T, Al-Kandari A, Arthurs B, et al. (2007) Epi- thelioid hemangioma (angiolymphoid hyperplasia with eosinophilia) of the orbit: a case report. J Med Case Rep 1: 30.
- Wold LE, Swee RG, Sim FH (1985) Vascular lesions of bone. Pathol Annu 20 Pt 2: 101-137.
- Nielsen GP, Srivastava A, Kattapuram S, Vikram Deshpande, John X O'Connell, et al. (2009) Epi- thelioid hemangioma of bone revisited: a study of 50 cases. Am J Surg Pathol 33(2): 270-277.
- Floris G, Deraedt K, Samson I, Brys P, Sciot R (2006) Epithelioid hemangioma of bone: a potentially metastasizing tumor? Int J Surg Pathol 14(1): 9-15.
- Fetsch JF, Weiss SW (1991) Observations concerning the pathogenesis of epithelioid hemangioma (angi- olymphoid hyperplasia) Mod Pathol 4(4): 449-455.
- Dorfman HD, Czerniak B (1998) Vascular lesions. In: Dorfman HD, Czerniak B, editors. Bone tumors. St. Louis, Mosby, USA, pp. 729-814.
- Kaleem Z, Kyriakos M, Totty WG (2000) Solitary skeletal hemangioma of the extremities. Skeletal Radiol 29(9): 502-513.
- Chawla A, Singrakhia M, Maheshwari M, Modi N, Parmar H (2006) Intraosseous haemangioma of the prox- imal femur: imaging findings. Br J Radiol 79(944): e64-e66.
- Boudousquie AC, Lawce HJ, Sherman R, Olson S, Magenis RE, et al. (1996) Complex translocation [7;22] identified in an epithelioid hemangioen- dothelioma. Cancer Genet Cytogenet 92(2): 116–121.
- O’Connell JX, Kattapuram SV, Mankin HJ, Bhan AK, Rosenberg AE (1993) Epithelioid hemangioma of bone: A tumor often mistaken for low-grade an- giosarcoma or malignant hemangioendothelioma. Am J Surg Pathol 17(6): 610-617.
- Calonje E, Fletcher CDM (2000) Tumors of blood vessels and lymphatics. In: Fletcher CDM, editor. Diagnos- tic Histopathology of Tumors. London: Hartcourt Publishers Limited. p. 55-56.
- Mentzel T, Beham A, Calonje E, Katenkamp D, Fletcher CD (1997) Epithelioid hemangioendothelioma of skin and soft tissues: clinicopathologic and im- munohistochemical study of 30 cases. Am J Surg Pathol 21(4): 363-374.
- Ling S, Rafii M, Klein M (2001) Epithelioid hemangioma of bone. Skeletal Radiol 30(4): 226-229.






























