The Cyclopean Muzzle-Central Giant Cell Granuloma
Anubha Bajaj*
Histopathologist in A B Diagnostics, New Delhi, India
Submission: October 20, 2021; Published: November 01, 2021
*Corresponding Address: Anubha Bajaj, Histopathologist in A B Diagnostics, New Delhi, India
How to cite this article: Anubha B. The Cyclopean Muzzle-Central Giant Cell Granuloma. Canc Therapy & Oncol Int J. 2021; 20(1): 556030. DOI: 10.19080/CTOIJ.2021.20.556029
Preface
Initially scripted by Jaffe in 1953, central giant cell granuloma is a benign, intraosseous lesion composed of cellular fibrous tissue admixed with multinucleated tumour giant cells, trabecular bone, and multiple foci of haemorrhage [1]. The condition is additionally denominated as giant cell reparative granuloma. An estimated 7% of benign jaw tumours are comprised of central giant cell granuloma. Of obscure aetiology, the lesion may emerge as a reactive condition, a developmental anomaly, or a benign neoplasm. Precise discernment of the condition is contingent to accurate interpretation of clinical, radiographic, and histological features.
Disease Characteristics
Central giant cell granuloma is essentially configured by intraosseous lesions, gradual, repetitive, minute haemorrhages or may be associated with trauma. Besides, central giant cell granuloma may delineate a genetic basis of origin [2,3]. Central lesions are unique to the jaw region and especially incriminate the anterior mandible. Mandible is frequently implicated, in contrast to maxilla wherein lesions may be confined to anterior or posterior jaws. Tumefaction is often restricted to tooth-bearing areas of the jaw although lesion may expand beyond the midline [2,3]. Sites such as extra-gnathic bones of craniofacial region and miniature, tubular bones of hands and feet may be implicated. Mandibular condyle is infrequently incriminated. A female preponderance is observed, possibly on account of hormonal secretion, with a female to male proportion of 2:1 [2,3]. The condition is generally discerned in children and young adults below < 30 years. Nearly 70% of lesions are predisposed to occur before < 30 years as osteogenesis, exfoliation, and eruption of teeth within the craniofacial skeleton develop significantly in young subjects whereas aforesaid processes are terminated in adulthood [2,3]. Multinucleated giant cells are posited to arise from peripheral blood mononuclear cells recruited from spindle-shaped cells of the stroma. Configuration of osteoclasts is contingent to interaction between stromal cells, immune reactive to receptor activator of nuclear factor kappa-B ligand (RANKL) and mononuclear precursors of osteoclasts, immune reactive to receptor activator of nuclear factor kappa-B (RANK) [2,3]. Giant cells appear to be a derivative of subset of mononuclear phagocytes. As giant cells of central giant cell granuloma are osteoclasts in nature, osteolytic expansion within the lesion may be curbed by therapeutic agents which prohibit concurrence between receptor activator of nuclear factor kappa-B ligand (RANKL) and receptor activator of NF-ḱB (RANK) such as osteoprotegerin and AMG162 [2,3]. Central giant cell granuloma demonstrates a minimal localized reoccurrence with absence of distant metastasis [2,3].
Clinical Elucidation
Majority of lesions manifest an expansible mass engendering facial asymmetry. Accompanying pain or extensive haemorrhage is infrequent [4,5]. Lesions are categorized into aggressive and nonaggressive subtypes contingent to occurrence of pain, brisk tumour progression, resorption to tooth root, perforation of bone cortex and possible localized tumour reoccurrence. Approximately 70% of central giant cell granulomas are nonaggressive and appear as asymptomatic, gradually progressive, painless masses [4,5]. An estimated 30% neoplasms are aggressive with destruction of circumscribing bone and soft tissue [4,5]. Around 20% individuals represent pain or paraesthesia whereas tumour swelling is a predominant (100%) clinical representation [4,5].
Histological Elucidation
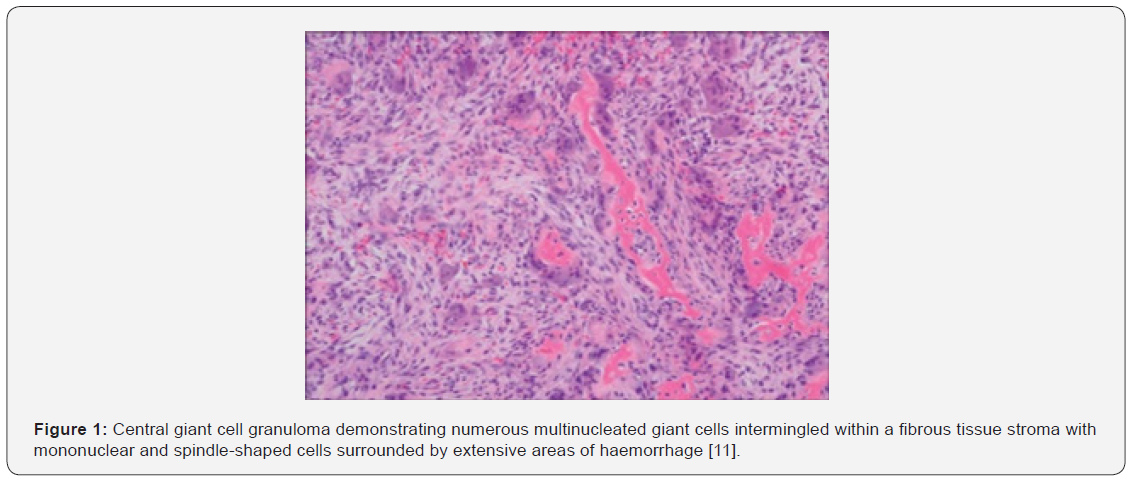
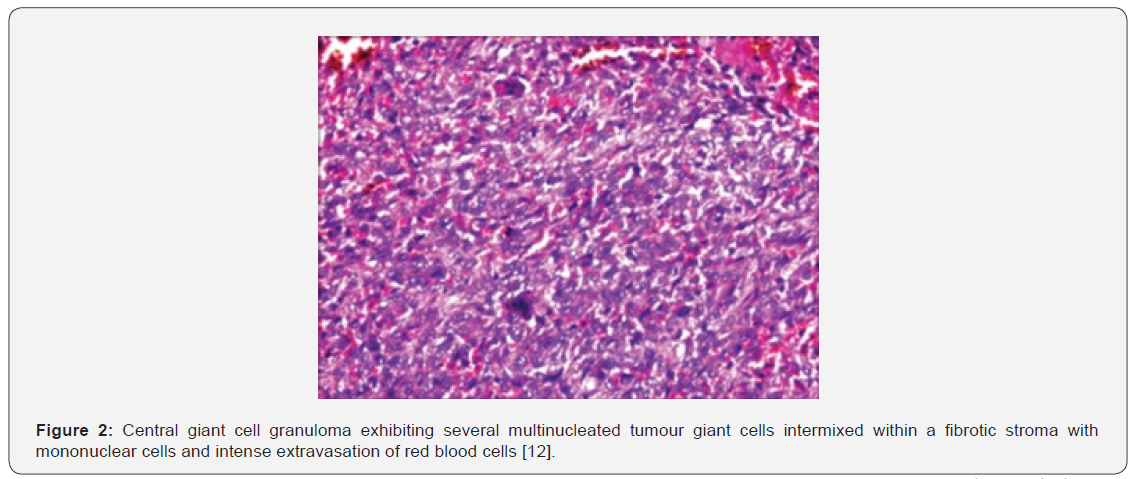
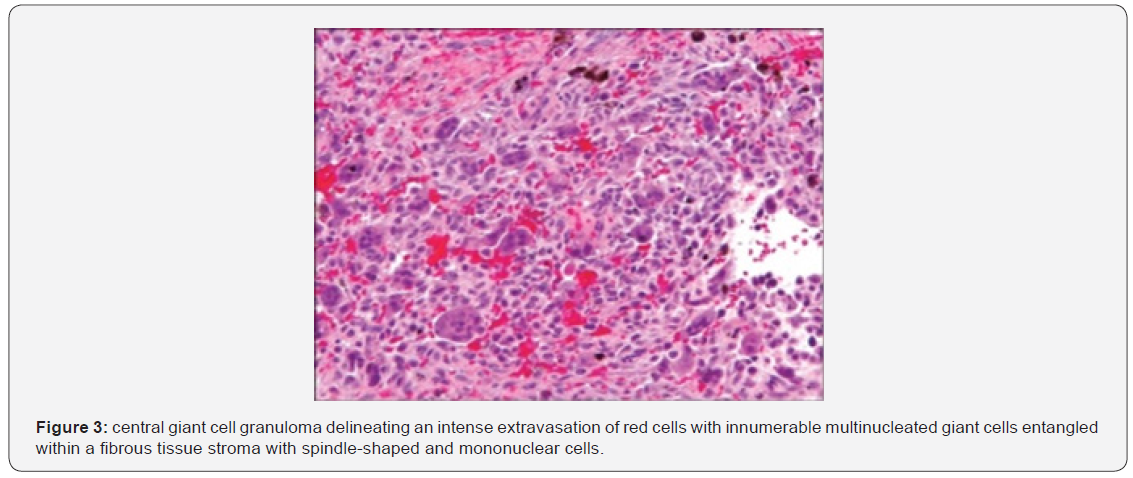
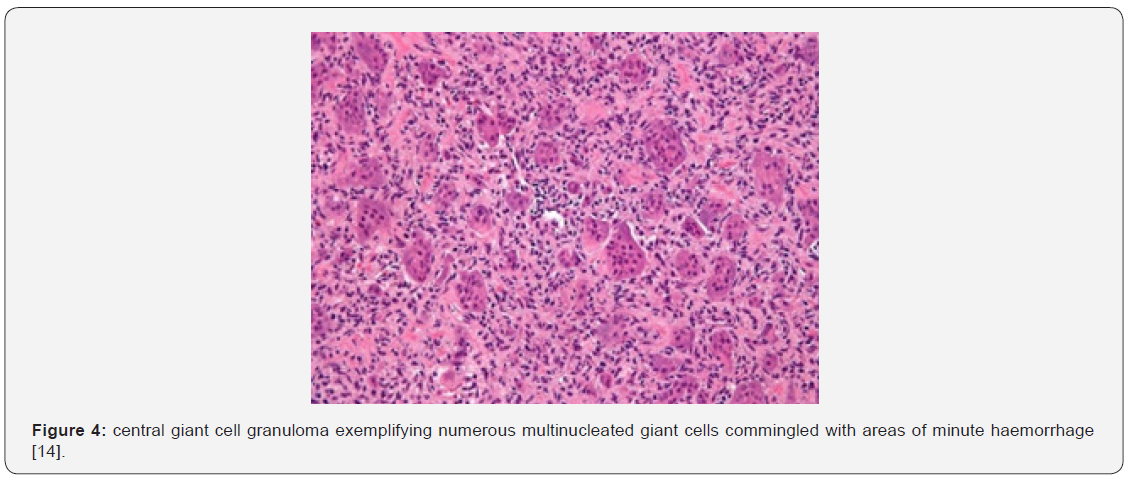
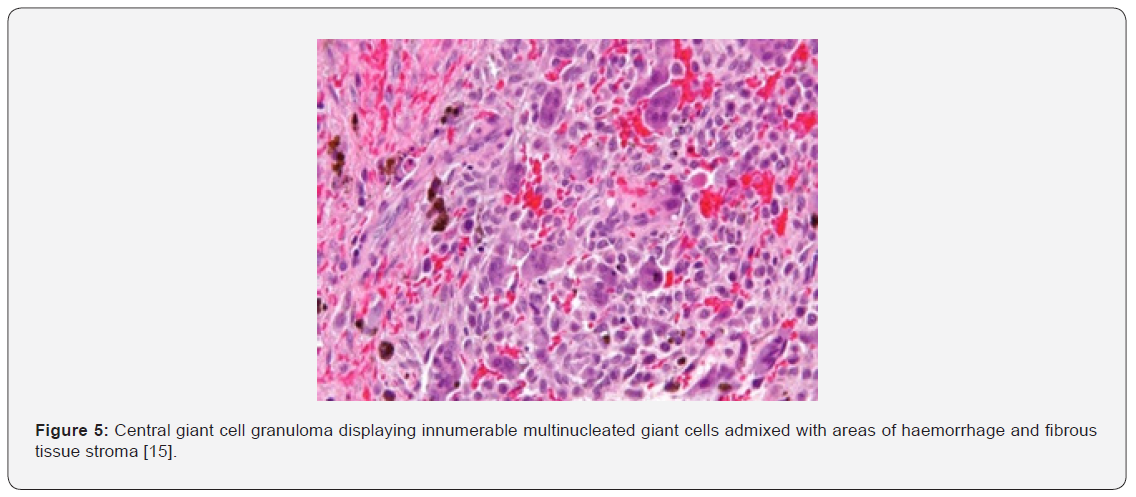
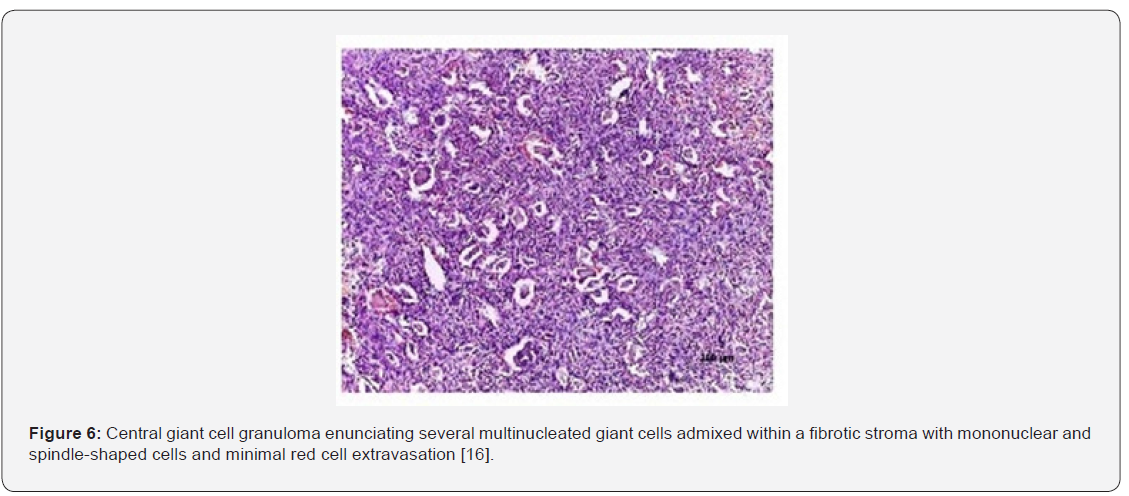
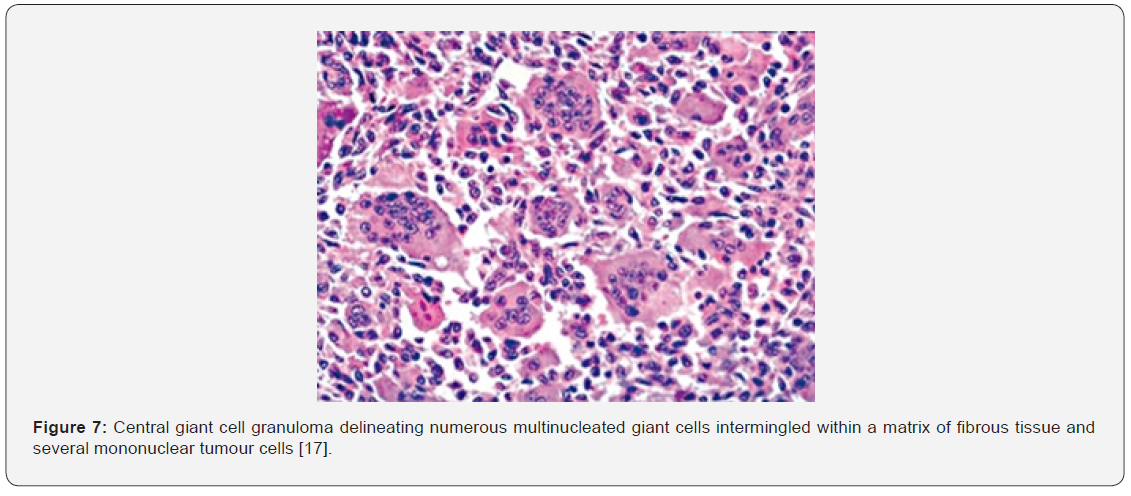
On gross examination, a cystic bone lesion is exemplified. Microscopically, several osteoclast-like, multinucleated giant cells appear adjacent to zones of haemorrhage and are admixed within a cellular, vascular, and fibrous tissue stroma. Foci of new bone formation are discernible upon perimeter of the lesion. Mitotic figures are frequently discerned although foci of necrosis are absent [5,6]. Majority of instances demonstrate classical features. Variations such as myxoid alterations, fibrosis or osteoid appear in around one third (~30%) subjects. Aggressive manifestations such as uniformly disseminated tumour giant cells or nuclei exceeding > 20 per cell may be observed [5,6]. Central giant cell granuloma represents as a non-neoplastic reactive condition posited to arise from intraosseous haemorrhage, trauma, defectively engendered or aberrantly repaired bone. Occasionally, the reactive disorder is concordant to pre-existing bone lesions such as fibrous dysplasia, Paget's disease of bone, central odontogenic fibroma, traumatic bone cyst and ossifying fibroma. Syndromic subcategories of central giant cell granuloma of the jaws may display systemic manifestations [5,6]. On microscopy, the intraosseous lesion is comprised of fibrous tissue admixed with aggregates of multinucleated giant cells. Majority of instances depict a classical morphology of mononuclear, elliptical to spindle-shaped tumour cells. Multiple foci of haemorrhage are intermingled with occasional bony trabeculae [5,6].
Aggressive lesions demonstrate significantly enhanced quantities of uniformly distributed, enlarged multinucleated giant cells with nuclei more than >20 per cell, prominent mitotic activity, and elevated fractional surface area. However, relapsing, and non-reoccurring lesions are morphologically identical [6,7]. Peripheral dissemination of osteoid functions as a barrier of reactive osteogenic tissue, is discernible in non-aggressive lesions and circumvents thorough curettage of the lesion [6,7]. On ultrastructural examination, the tumefaction is composed fibroblasts, myofibroblasts and histiocytes [6,7] (Figures 1-8).
Immune Histochemical Elucidation
Tumour giant cells are immune reactive to CD68. Intense, diffuse immune reactivity to receptor activator of NF-ḱB (RANK) and receptor activator of nuclear factor kappa-B ligand (RANKL) is exemplified within mononuclear and multinucleated giant cells. Tumour cells of central giant cell granuloma of the jaw are immune reactive to RANK and RANKL. Mononuclear and multinucleated tumour cells are immune nonreactive to p63 [2,3].
Differential Diagnosis
Central giant cell granuloma necessitates a segregation from diverse lesions such as hyperparathyroidism, ameloblastoma, giant cell tumour of long bones and odontogenic tumour [8,9]. Differentiation is required from •aneurysmal bone cyst is as lesion which demonstrates fluid- filled levels upon plain radiography. Morphologically, giant cells are unevenly dispersed and are accumulated around blood- filled, cystic spaces. Also, fibrous tissue septa comprised of bland, spindle-shaped cells, fibroblasts, myofibroblasts and fragments of woven bone traverse the neoplasm. Miniature, irregularly dispersed giant cells are commonly articulated within an aneurysmal bone cyst wherein solid foci are fibrotic. Genomic rearrangements of USP6 gene are discerned in an estimated 70% instances [8,9].
•Giant cell tumour of bone or osteoclastoma is a predominantly osteoclastogenic, stromal neoplasm composed of mononuclear cells, macrophages and innumerable, osteoclast-like, multinucleated giant cells uniformly distributed throughout the tumefaction. Osteoclastoma demonstrates foci of evenly disseminated, elongated, elliptical or polygonal mononuclear cells. Giant cells do not circumscribe haemorrhagic areas, in contrast to central giant cell granuloma, giant cell lesion of small bones or aneurysmal bone cyst [8,9].
•Hyperparathyroidism engendering the classic “brown tumour” is composed of fibrous tissue admixed with aggregates of multinucleated giant cells. Mononuclear, elliptical to spindle-shaped tumour cells are intermingled with multiple foci of haemorrhage. Tumefaction demonstrates enhanced activity of osteoclasts associated with tunnelling of osteoclasts into the circumscribing bone matrix. A significantly enhanced configuration of bone ensues along with prominent peri-trabecular fibrosis [8,9]. Additionally, central giant cell granuloma necessitates segregation from genetically concurrent giant cell lesions such as cherubism, Noonan syndrome and neurofibromatosis type 1. Tumours, cysts, and tumour-like conditions arising within the pre-auricular region also mandate a demarcation [8,9].
Investigative Assay
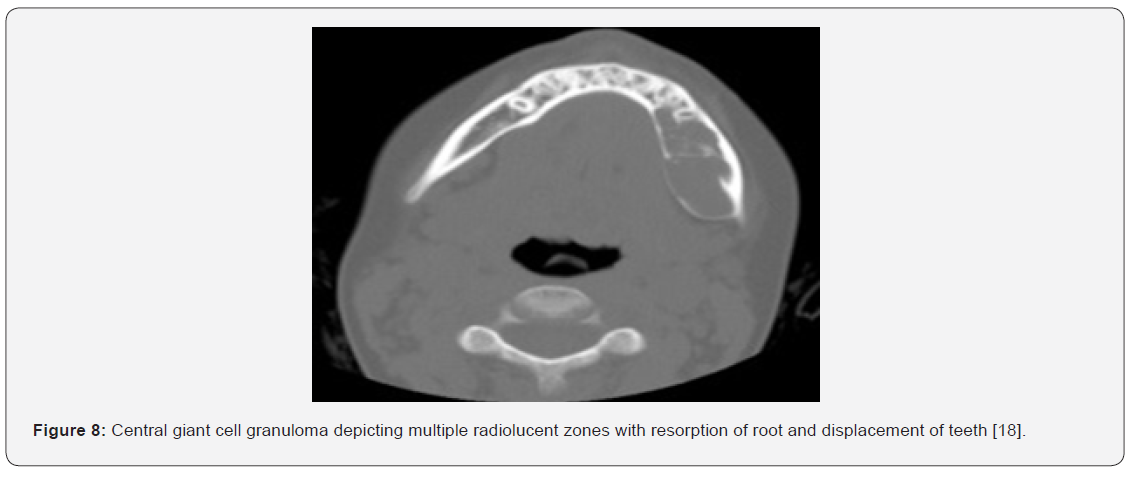
Upon plain radiography, multi-loculated or well circumscribed, unilocular or diffuse, radiolucent tumour zones are observed. Majority of lesions (50%) demonstrate multi-locular radiolucency [9,10]. Well demarcated, unilocular or multilocular radiolucent lesions discernible upon plain radiography are circumscribed by an undulating perimeter. Aggressive, rapidly progressive lesions occurring in younger individuals are poorly demarcated and exhibit variable destruction of bone cortex [9,10]. Computerized tomography (CT) is optimal for assessing tumour location, expanse, anatomical configuration, and adherence to adjoining structures [9,10]. Features of tumour aggression emerging within central giant cell granuloma of the jaw such as cortical expansion, displacement of tooth, resorption of root, perforation of bone cortex, incrimination of maxillary sinus and disintegrated inferior margin of the mandible may be exhibited. Localized tumour reoccurrence is observed in roughly 13% to 49% individuals. Multiple reoccurrences may ensue. Serum alkaline phosphatase may be elevated [9,10].
Therapeutic Options
Comprehensive surgical extermination of the neoplasm is optimal. Alternatively, simple curettage of the lesion along with peripheral bone osteotomy may be adopted. En bloc surgical extermination is recommended in instances with extensive neoplasms. Conventional therapy for jaw lesions is localized curettage of the neoplasm although the procedure is accompanied by extended proportionate reoccurrence of around 70%, especially within aggressive tumefaction [9,10]. Central giant cell granuloma of the condylar region may be treated with simple curettage or surgical resection of the lesion. Extensive surgical manoeuvers may culminate in significant mutilation of jaws, face, deprivation of teeth and occurrence of dental germs [9,10].
Surgical therapy of central giant cell granuloma is contingent to tumour magnitude and location. Manoeuvers such as simple excision, curettage, en bloc surgical resection and reconstruction of tumour site may be adopted. Around 30% lesions demonstrate localized tumour reoccurrence upon employment of aforesaid methodologies [9,10]. Alternative, contemporary nonsurgical treatment methodologies such as intra-lesional injection of steroids and subcutaneous injection of calcitonin or interferon-α may be adopted. Aforesaid procedures are beneficial in accomplishing tumour resolution or decimation of tumour magnitude along with sparing of surgical mutilation [9,10].
References
- Jaffe H (1953) Giant-cell reparative granuloma, traumatic bone cyst, and fibrous (fibro-oseous) dysplasia of the jawbones” Oral Surg Oral Med Oral Pathol6(1): 159–175.
- Hosur MB, Puranik RS, Shreenivas S Vanaki, Surekha R Puranik, Pramod S Ingaleshwaret al. (2018) Clinicopathological profile of central giant cell granulomas: An institutional experience and study of immunohistochemistry expression of p63 in central giant cell granuloma. J Oral Maxillofac Pathol 22(2): 173-179.
- Bocchialini G, Salvagni L, Agostino Guerini, Andrea Castellani(2019) Central giant cell granuloma of the mandibular condyle: A rare case and a literature review. Heliyon 6(1): e03085.
- Gustavo de la Roza (2011) P63 expression in giant cell-containing lesions of bone and soft tissue. Arch Pathol Lab Med 135(6): 776–779.
- Vered M, Buchner A, Dan Dayan (2008) Central giant cell granuloma of the jawbones - New insights into molecular biology with clinical implications on treatment approaches” Histol Histopathol 23(9): 1151-1160.
- Bilodeau E, Chowdhury K, Bobby Collins (2009) A case of recurrent multifocal central giant cell granulomas. Head Neck Pathol 3(2): 174-178.
- Saw S, Thomas N, Michael J Gleeson, Istvan Bodi, Steve Connor, et al. (2009) Giant cell tumour and central giant cell reparative granuloma of the skull: do these represent ends of a spectrum? A case report and literature review. Pathol Oncol Res15(2): 291-295.
- Dickson BC, Li SQ, Jay S Wunder, Peter C Ferguson, Behnam Eslami, et al. (2008) Giant cell tumour of bone express p63. Mod Pathol 21(4): 369-375.
- Farrier SL, Farrier JN, M K Smart, E S Nash (2006) A 10-year review of the occurrence and treatment of central giant cell granulomas, in a District General Hospital. J Oral Pathol 35(6): 332-337.
- Daroit NB, de Marco RG, Manoel Sant’ Anna Filho, Guilherme G Fritscher (2017) The challenge in the treatment of central giant cell granuloma - What is the best approach? J Oral Maxillofac Surg Med Pathol 29(2): 122-128.
- Image 1 Courtesy: Annals of Maxillofacial Surgery.
- Image 2 Courtesy: Natl Journal of Maxillofacial Surgery.
- Image 3 Courtesy: Journal of Clinical Practice.
- Image 4 Courtesy: com
- Image 5 Courtesy: Wikipedia
- Image 6 Courtesy: com
- Image 7 Courtesy: Pathology outlines.
- Image 8 Courtesy: Journal of Oral and Maxillofacial Surgery.






























