The Glistening Beret- Osteochondroma
Anubha Bajaj*
Histopathologist in A B Diagnostics, New Delhi, India
Submission: June 27, 2021;; Published: August 04, 2021
*Corresponding Address: Anubha Bajaj, Histopathologist in A B Diagnostics, New Delhi, India
How to cite this article: Anubha B. The Glistening Beret- Osteochondroma. Canc Therapy & Oncol Int J. 2021; 19(3): 556015. DOI: 10.19080/CTOIJ.2021.19.556015
Preface
Osteochondroma is a commonly discerned bone tumour appearing upon superficial bone surface and is constituted of cortical and medullary bone displaying a superimposed cap of hyaline cartilage. Tumefaction is comprised of cortical bone and a contiguous medullary cavity, features which are pathognomonic of the benign neoplasm. The benign, surface neoplasm demonstrates an exophytic growth composed of stalk of mature bone and cartilaginous cap. Marrow space and cancellous bone of tumour stalk appears contiguous with the underlying bone. Osteochondroma may emerge as a solitary neoplasm or demonstrate multiple lesions. Solitary osteochondroma is additionally denominated as osteocartilaginous exostosis. Multiple osteochondromas configure an autosomal dominant syndrome designated as hereditary multiple exostosis or familial osteochondromatosis.
Disease Characteristics
Osteochondroma is a common, benign tumour constituting around 20% to 50% of benign bone tumours and roughly 10% to 15% of comprehensive benign or malignant bone neoplasms. Nearly 1% to 2% of individuals with radiographic evaluation demonstrate an incidental solitary osteochondroma [1,2]. Osteochondroma may emerge as a benign, irradiation induced tumour with a prevalence of around 6% to 24%. Post-radiation osteochondroma usually appears following a latent period of 3 years to 17 years [1,2]. Majority (85%) of osteochondromas are solitary and asymptomatic. Approximately 75% to 80% lesions are characteristically discovered in childhood, prior to 20 years. Symptomatic lesions generally manifest within younger individuals. A male predilection is observed with a male to female proportion of 2:1 [1,2].
Around 50% neoplasms occur within long bones, predominantly within lower extremities with a proportion of 2 :1 w.r.t upper extremities. Femur is implicated in roughly 30% instances wherein distal lesions are frequent. Tibia and humerus are incriminated in nearly 10% to 20% subjects. Proximal tibia is frequently involved, in contrast to distal tibia. Therefore, osteochondroma emerging adjacent to the knee is extremely common [1,2]. Generally, the neoplasm arises within metaphysis of long bones such as femur followed in frequency by humerus and tibia. Flat bones such as ilium and scapula may display the neoplasm whereas small bones of hands, feet, ribs, or vertebrae are exceptionally incriminated [1,2]. Solitary osteochondroma is categorized into •primary osteochondroma which develops spontaneously in the absence of a precipitating event •secondary osteochondroma which occurs on account of radiation exposure in childhood or trauma such as surgery or fracture [1,2]. Skeletally immature subjects depict lesions of enhancing magnitude. Nevertheless, tumour growth or altered tumour morphology following skeletal maturity may be indicative of malignant metamorphosis. Tumefaction may be sessile or pedunculated wherein pedunculated lesions extend away from the adjacent joint [3,4].
Osteochondroma is associated with complications such as osseous deformities, fracture, compromised vascular articulations, neurologic symptoms, configuration of bursa along with or absence of concurrent bursitis or malignant transformation [3,4]. Solitary osteochondroma is associated with simple cosmetic deformities, serious neurological complications, and malignant metamorphosis. Cosmetically disfiguring lesions are exemplified as a painless swelling [3,4]. Osteochondroma can engender impingement of neurovascular bundles with compression of adjacent neurovascular structures, neuropathy, and vascular insufficiency. Irritation of abutting soft tissue can generate an inflamed, painful bursa [3,4]. Neurological impingement with osteochondroma is accompanied by diverse clinical representations as peripheral neurological symptoms, radiculopathy due to nerve root compression, serious myelopathy, and spinal stenosis contingent to tumour site [3,4].
Osteochondroma can compromise vascular supply to adjacent soft tissues by configuring a pseudo-aneurysm or by direct compression of abutting blood vessels with consequent hindrance with vascular outflow. Pseudo-aneurysm is articulated on account of chronic, repetitive mechanical compression and friction of vascular arrangements. Thus, pseudo-aneurysm of popliteal vessels and peroneal nerve entrapment are commonly discerned [3,4]. Restriction of joint mobility, premature osteoarthritis, and osseous deformities with disruption of daily routine may also ensue. Malignant metamorphosis occurs in an estimated 1% of solitary osteochondroma. Enlargement of tumefaction or altered radiographic appearance may indicate a malignant transformation [3,4]. Grade 1 or grade 2 conventional chondrosarcoma is a commonly discerned malignant neoplasm occurring subsequent to transformation of osteochondroma. Emergence of osteosarcoma is also documented [4].
Disease Pathogenesis
As osteochondroma manifests as a solitary lesion or as a component of numerous osteochondromas with multiple hereditary exostoses, it is posited that osteochondroma is a developmental lesion engendered from cellular segregation of epiphyseal growth plate [5,6]. As osteochondroma develops from displaced cartilage cells constituting growth plates, it is hypothesized that endochondral ossification of articulated bone may configure an osteochondroma. Solitary osteochondroma is engendered due to a developmental anomaly, rather than arising as a true neoplasm. Possibly, a fragment of growth plate herniates through the periosteum which evolves perpetually with consequent emergence of a sessile or pedunculated lesion, commonly within the metaphyseal region. Detached fragment of growth plate can spontaneously appear as primary osteochondroma or a secondary osteochondroma may emerge because of irradiation, surgical intervention, or fracture [5,6].
Osteochondroma emerging because of trauma or irradiation is documented. Nevertheless, a contemporary hypothesis indicates the osteochondroma to be a true neoplasm as genetic mutations are known to occur within solitary neoplasms and lesions of multiple hereditary osteochondromatosis [5,6]. Solitary osteochondroma is posited to represent a true, benign neoplasm as specific genetic mutations within genes encoding exostosin 1 (EXT1) are exemplified. Solitary, sporadic osteochondroma is associated with loss of function chromosomal mutations within EXT1 (8q24) and EXT2 (11p11) genes. Solitary lesion delineates somatic inactivation of EXT gene within tumour cells confined to the cartilaginous cap [5,6].
Clinical Elucidation
Solitary osteochondroma is usually asymptomatic and lesions are discovered incidentally upon employment of plain radiography adopted for unrelated conditions. Although frequently asymptomatic, osteochondroma may engender clinical symptoms pertaining to fracture, tumour progression or impingement of adjacent neurovascular structures [5,6]. Symptomatic lesions appear secondary to factors such as a palpable mass, fracture, malignant transformation, compression of adjacent neurovascular bundle, formation of bursa or concomitant bursitis. Cross-sectional imaging is optimally indicated to evaluate aforesaid complications arising within symptomatic lesions [5,6].
Histological Elucidation
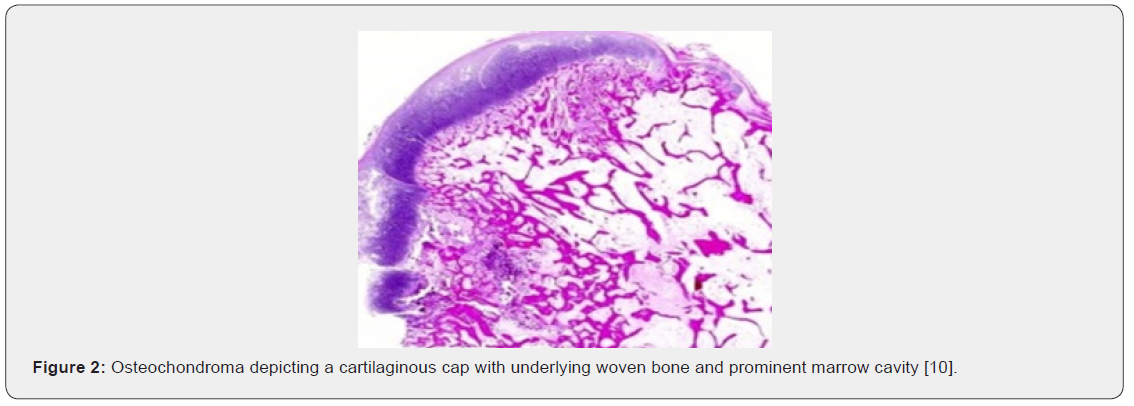
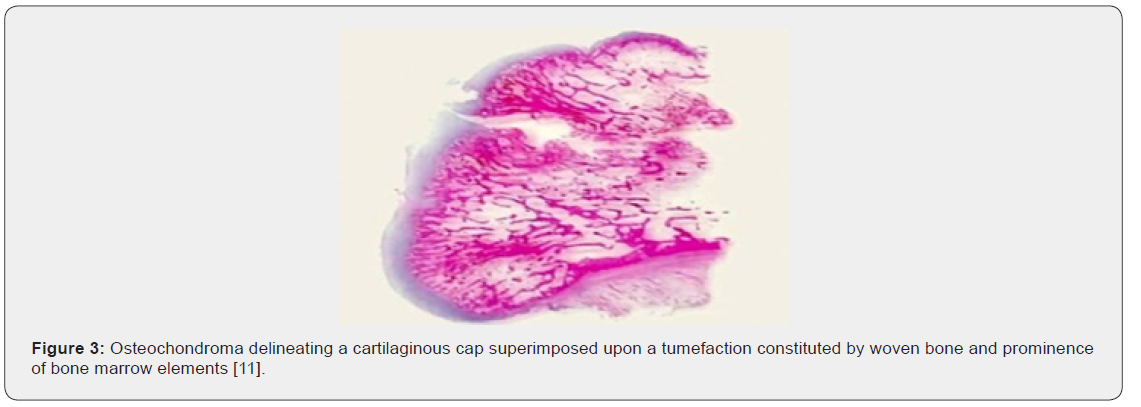
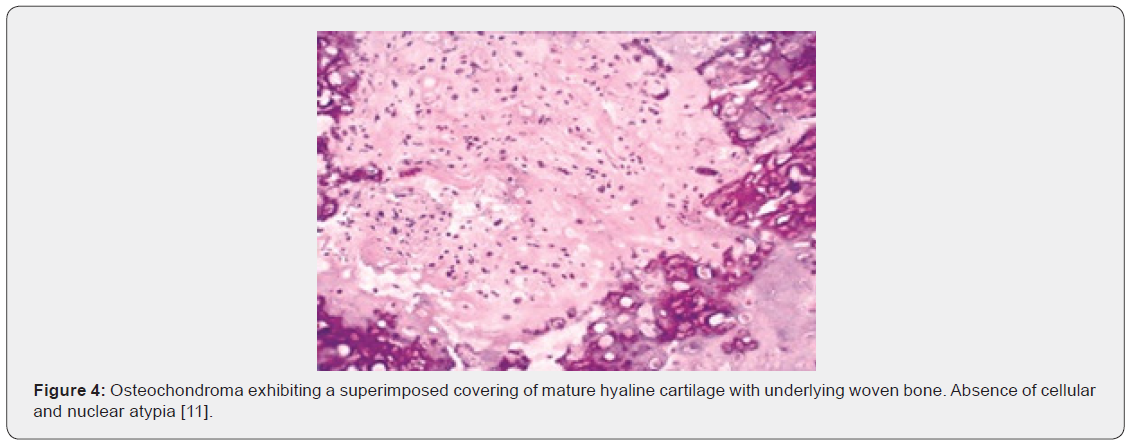
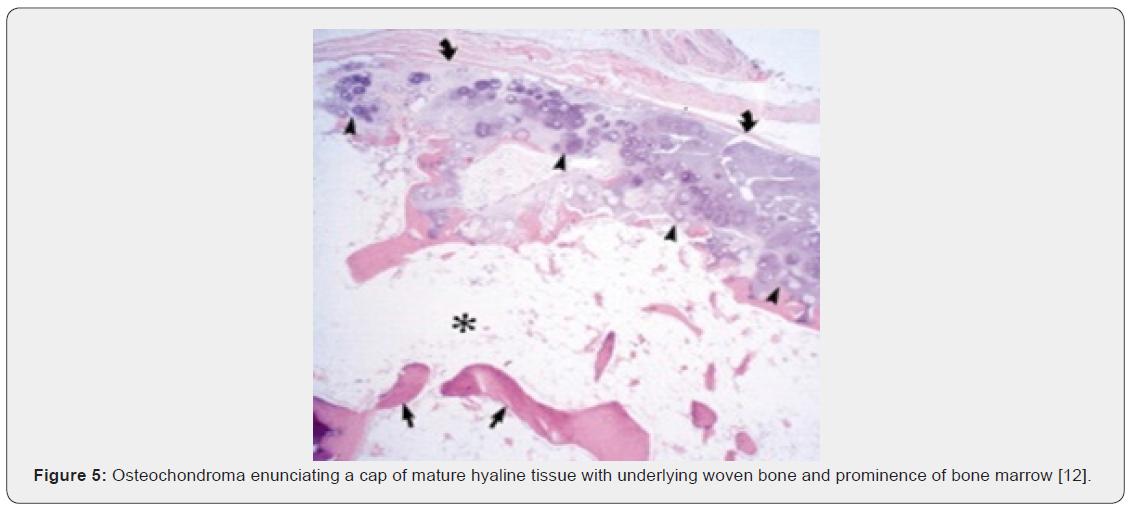
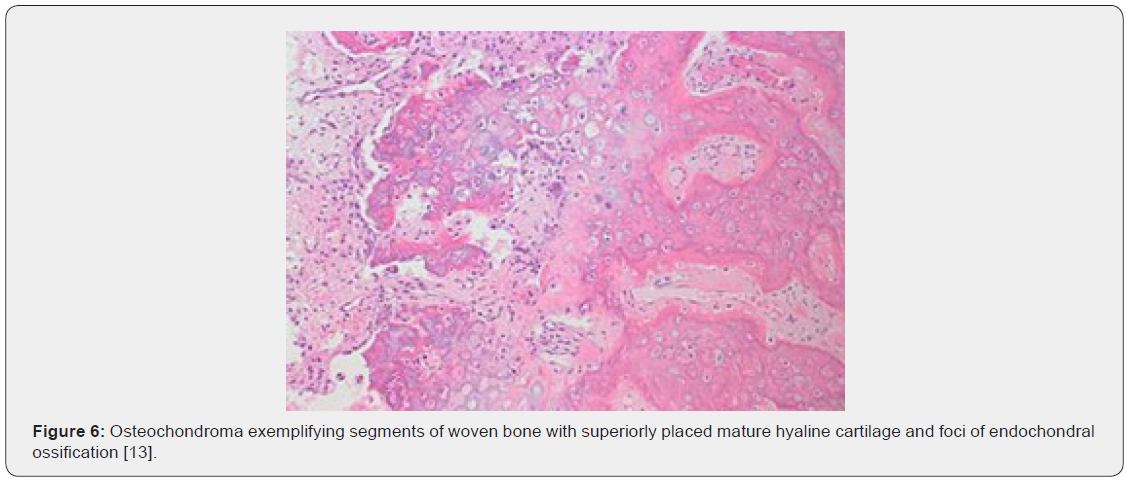
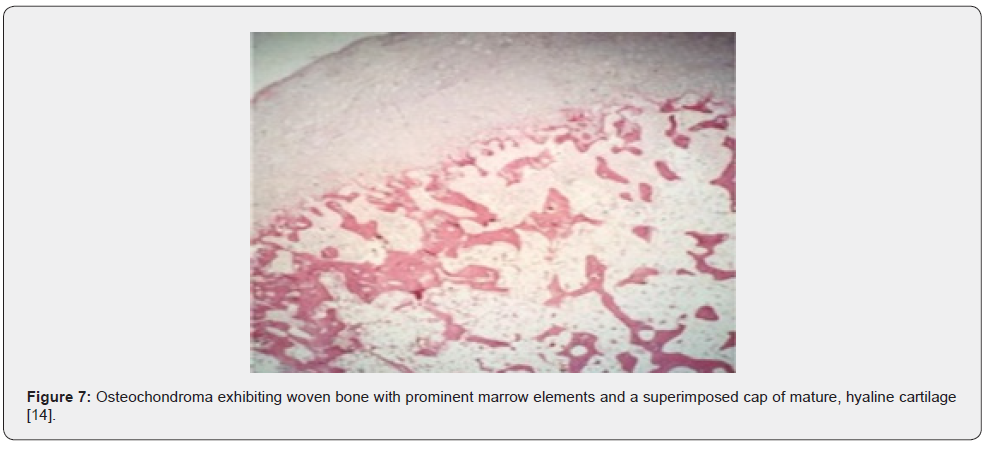
On gross examination, osteochondroma appears as a lobulated, cauliflower-like, sessile, or pedunculated lesion arising from the bone surface. The cartilaginous cap is glistening, shiny and bluish grey. A thin fibrous capsule or perichondrium appears to be continuous with underlying bony periosteum. Macroscopically, a pedunculated or sessile bony lesion with a superimposed hyaline, cartilaginous cap is observed [4,6]. Cartilaginous cap normally demonstrates a thickness of 1 centimetre to 3 centimetres, especially in children due to ongoing bone evolution whereas cartilaginous cap is absent or minimally thick in a mature skeleton. Cartilaginous cap thickness exceeding >2 centimetres in an adult may indicate malignant metamorphosis within an osteochondroma. Variable mineralization within the cartilaginous cap may ensue [4,6]. Perichondrium, cortex, and medulla of osteochondroma are contiguous with underlying bone. On microscopy, cartilaginous cap superimposed upon and within peripheral region of the tumefaction delineates an identical morphology as the growth plate. Endochondral ossification is discernible at the junction of cartilaginous cap and underlying bone [4,6]. Medullary segment of the tumefaction is configured by yellow, non - hematopoietic marrow engendered due to endochondral ossification. Cartilaginous cap is composed of mature hyaline cartilage with encompassing fibrous perichondrium [4,6].
Tumours appearing in younger subjects depict a transition between bone and cartilaginous cap simulating the growth plate with endochondral ossification and metamorphosis into mature bone. In older lesions, eventually the cartilaginous cap diminishes and disappears. Elements of bone marrow may arise within the bony stalk wherein bone marrow space or cancellous bone appears contiguous with underlying native bone [5,6]. Solitary osteochondroma is associated with chromosomal mutations of EXT1 and EXT2 genes [4,5] (Figures 1-8).
Differential Diagnosis
Conditions which morphologically recapitulate an osteochondroma are multiple osteochondromas, subungual exostosis, dysplasia epiphysealis hemimelica or Trevor’s disease, Turret’s exostosis, traction exostosis, bizarre parosteal osteochondroma, Tous proliferation and florid reactive periostitis [7,8]. Segregation is also necessitated from sub-periosteal hematoma, parosteal osteosarcoma or juxtacortical chondroma, lesions which lack contiguity with the medullary canal [7,8]. Osteochondroma mandates a segregation from benign and malignant lesions such as
•subungual exostosis or Dupuytren’s exostosis which is a commonly discerned lesion of obscure aetiology posited to arise secondary to preceding trauma or infection. Classically, a painful, surface lesion emerges from dorsal aspect of distal phalanx abutting the nail bed and is associated with cutaneous ulceration. Subungual exostosis lacks contiguity with medullary space [1,2].
•dysplasia epiphysealis hemimelica (Trevor’s disease) is an exceptional disease associated with occurrence of multiple osteochondromas usually within the epiphyseal region of lower extremities. A male predominance is observed with a male to female proportion of 3:1. The condition arises within young individuals who demonstrate alteration of gait, osseous deformities, or palpable tumefaction. Malignant metamorphosis of emerging neoplasms is absent [1,2].

•Turret’s exostosis delineates an extra-cortical mass situated upon the dorsum of middle or proximal phalanx. Contiguity with underlying medullary spaces is absent [1,2].
•bizarre parosteal osteochondromatous proliferation (Nora’s lesion) is a lesion situated upon superficial bone surface and commonly incriminates osseous structures situated upon distal extremities as the hands or feet. Of obscure aetiology, the condition is posited to arise because of preceding trauma. Contiguity with medullary spaces and malignant metamorphosis is absent. The lesion denominates a disorganized growth of bone and cartilage with characteristic occurrence of blue bone [1,2].
•parosteal osteosarcoma is a subcategory of osteosarcoma arising from surface of long bones. Plain radiographs demonstrate an enlarged, lobulated, dense, osseous mass devoid of contiguity with medullary spaces. Advanced lesions can infiltrate medullary spaces. The neoplasm commonly emerges from metaphysis of long bones wherein posterior perimeter of distal femur is a singular, frequently discerned location.
The neoplasm depicts an identical location and age of disease emergence as osteochondroma. Tumefaction delineates foci of aggressive tumour growth with areas of neoplastic woven bone and fibroblastic tissue. An estimated 25% of neoplasms exhibit a cartilaginous cap [1,2].
•juxtacortical chondroma is a tumefaction commonly discerned between 20 years to 40 years. Lesion is situated upon the bone surface with consequent “saucer-shaped” deformity of adjacent bone cortex and associated periosteal reaction [1,2].
•subperiosteal hematoma is a neoplasm confined to the bone surface demonstrating a smooth, elliptical, superficial cortical perimeter wherein the tumefaction lacks contiguity with medullary space. Centric segment of the lesion demonstrates heterogeneity with occurrence of cystic areas, mineralization, or adipose tissue deposition. Tumefaction arises in subjects with history of preceding trauma [1,2].
•florid reactive periostitis is a condition which typically arises within periosteum of fingers. Lesion is composed of an admixture of reactive woven bone and fibrous tissue with the absence of pertinent zonation [1,2].
•secondary chondrosarcoma enunciates an infiltrative pattern of tumour growth with permeation of bone or extension into adjacent soft tissue. Generally, tumefaction is well differentiated although infiltration into circumscribing soft tissue is discerned [1,2].
Investigative Assay
Plain radiographs can adequately discern the neoplasm. However, cross-sectional imaging is indicated for assessment of associated complications, evaluating the cartilaginous cap or establishing contiguity with medullary canal [7,8]. Contiguity with medullary spaces is minimally discernible upon plain radiography of solitary osteochondroma arising within flat bones such as pelvis, scapula and vertebral column. In aforesaid instances, cross-sectional imaging is necessitated to adequately characterize the neoplasm [7,8]. Solitary osteochondroma is discovered incidentally upon plain radiography. Osteochondroma incriminating the long bones generally depict a pathognomonic appearance. Sessile or pedunculated lesions are localized upon bony surface within the region of metaphysis and appear contiguous with cortex and medullary canal. Pedunculated lesions are directed away from the adjacent joint. Characteristic cartilaginous cap may not be discernible on plain radiography [7,8]. On plain radiography, pedunculated or sessile neoplasms depict a stalk of mature bone which is contiguous with bone cortex wherein cancellous bone communicates with the underlying bone. The attenuated, lobulated cartilaginous cap may contain foci of calcification. Tumour extension is perpendicular to long axis of the bone [7,8].
Tumefaction arising in skeletally immature subjects may gradually enhance in magnitude. However, osteochondroma appearing in skeletally mature subjects is stable and enlarging lesions require cogent evaluation for malignant metamorphosis [7,8]. Malignant transformation is indicated by altered morphology, periostitis or indistinct perimeter of bone cortex. Also, an irregular bone surface, radiolucent areas, heterogeneous mineralization, and a thickened cartilaginous cap exceeding > 2-centimetre magnitude are indicative of malignant transformation on plain radiography. Aforesaid instances are appropriately managed by surgical eradication or cogent tissue sampling [8,9]. Osteochondroma arising within flat bones such as scapula, pelvis or vertebral column may be indistinguishable upon radiography and necessitate additional evaluation to demonstrate a contiguous cortico-medullary junction [8,9].
Symptomatic subjects or tumefaction with distinctive, concerning radiographic features or potential complications mandate further evaluation with diverse cross-sectional imaging techniques such as magnetic resonance imaging (MRI), computerized tomography (CT) or ultrasonography (US) [8,9]. Magnetic resonance imaging (MRI) is optimally indicated for assessing the cartilaginous cap. A thickened cartilaginous cap may indicate malignant transformation. Cartilaginous cap delineates an intermediate to enhanced signal intensity upon T2 weighted imaging and proton density (PD) weighted imaging [8,9]. A thick cartilaginous cap discerned within tumefaction arising in skeletally immature subjects appear one centimetre to 3 centimetre in magnitude. In contrast, osteochondroma emerging in skeletally mature individuals demonstrate a cartilaginous cap few millimetres in thickness. Cartilaginous caps exceeding 2 centimetres in skeletally mature individuals require evaluation for malignant metamorphosis with cogent tissue sampling [8,9]. Magnetic resonance imaging (MRI) is employed to assess inflamed bursae and tumour impingement or displacement of neurovascular bundles. Incriminated nerves with associated neurologic findings may be displaced, enlarged, or delineate a hyper-intense signal upon T2 imaging or proton density imaging. Additionally, nerve innervated musculature may demonstrate oedema with acute denervation injury or infiltration of mature adipose tissue with chronic denervation injury. MRI can also depict bone marrow oedema, periosteal reaction and degree of healing in fractures appearing in chronic lesions [8,9]. Vascular complications of osteochondroma are pseudo-aneurysm, vascular compression or occlusion contingent to incrimination of arterial or venous articulations [8,9]. Bone scintigraphy is not recommended as benign and malignant lesions may exhibit enhanced radiotracer activity [8,9].
Therapeutic Options
Treatment of osteochondroma is individualistic and varies in diverse individuals. Solitary, miniature, asymptomatic osteochondroma with distinctive imaging features can be managed with appropriate follow-up [8,9]. Tumour evolution ceases following skeletal maturity and lesions may undergo spontaneous involution. Surgical extermination of solitary lesions is characteristically curative and localized tumour reoccurrence is exceptional [8,9]. Enlarged, symptomatic lesions with suspicious features on imaging such as tumour progression with extensive cartilaginous cap in skeletally mature subjects, irregular or indistinct tumour margins, focal areas of radiolucency and osseous erosions or destruction require evaluation with cross sectional imaging and cogent surgical extermination [8,9]. Surgical excision of pedunculated lesions is simpler than sessile lesions. An estimated 2% reoccurrence is documented following surgical resection [8,9]. Majority of miniature, asymptomatic, solitary osteochondromas are associated with a superior prognosis wherein malignant metamorphosis occurs in around 1% individuals. Possible complications of the tumefaction are fracture, impingement upon neurovascular bundles and configuration of bursa [8,9]. Symptomatic lesions can be managed with cogent surgical excision. Neoplasms subjected to surgical extermination may be followed by tumour reoccurrence, injury to neurovascular bundles and compartment syndrome. Spontaneous retrogression of solitary lesions may ensue [8,9].
References
- Alabdullrahman LW, Byerly DW (2020) Osteochondroma” Stat Pearls International, Treasure Island, Florida, USA.
- Garcia RA, Inwards CY, Krishnan K Unni (2011) Benign bone tumours- recent developments” Semin Diagn Pathol 28(1): 73-85.
- Motamedi K, Seeger LL (2011) Benign bone tumours. Radiol Clin North Am 49(6): 1115-1134.
- Hakim DN, Pelly T, Myutan Kulendran, Jochem A Caris (2015) Benign tumours of the bone: A review. J Bone Oncol 4(2): 37-41.
- Duarte Silva J, Ferreira M, Marina Neto, Jose Teixeira, Filipe Duarte (2018) Pseudo-aneurysm of the popliteal artery associated with tibial osteochondroma. Rev Port Cir Cardiotorac Vasc 25(1-2): 103-104.
- Henry JC, Mouawad NJ, Laura Phieffer, Michael R Go (2015) Tibial osteochondroma inducing popliteal artery compression. J Vasc Surg 61(6): 1595-1598.
- Douis H, Saifuddin A (2012) The imaging of cartilaginous bone tumours. I. Benign lesions. Skeletal Radiol 41(10): 1195-1212.
- Aiba H, Yamada S, Norio Yamamoto, Katsuhiro Hayashi, Shinji Miwa,et al. (2018) Spontaneous shrinkage of solitary osteochondromas. Skeletal Radiol 47(1): 61-68.
- Heyworth PB, Rashid M (2019) Regression of a solitary osteochondroma of the distal humerus in a toddler following trauma. Radiol Case Rep 14(2): 187-189.
- Image 1 Courtesy: You tube
- Image 2 Courtesy: com
- Image 3 and 4 Courtesy: Pathology outlines
- Image 5 Courtesy: RSNA publications online
- Image 6 Courtesy: Libre pathology
- Image 7 Courtesy: Orthobullets.com
- Image 8 Courtesy: Atlas of Genetics and Cytogenetics.






























