Cutaneous Metastases in Adenocarcinoma of Gastro-Esophageal Junction – A Rare Entity
Dr. Garima Tripathi*
Post-Graduate DNB Trainee, Action Cancer Hospital, Radiation oncology department, India
Submission: February 19, 2021; Published:March 16, 2021
*Corresponding Address:Dr. Garima Tripathi, Post-Graduate DNB Trainee, Action Cancer Hospital, Radiation oncology department, India
How to cite this article:Dr. Garima T. Cutaneous Metastases in Adenocarcinoma of Gastro-Esophageal Junction – A Rare Entity. Canc Therapy & Oncol Int J. 2021; 18(3): 555988.DOI: 10.19080/CTOIJ.2019.18.555988
Abstract
Adenocarcinoma of the gastro-oesophageal (G.E) junction is a rare form of cancer that tends to follow the typical pattern of metastases seen in oesophageal cancers. However, here we present a rare case of a primary adeno carcinoma of G.E junction with cutaneous metastases (CM) to three different locations of right forearm treated with radiotherapy. Patient was a documented case of multiple metastasis to lung, skin, brain, adrenals and liver as per whole body PET CT scan. Cutaneous metastases are very rare and has no specific pattern of occurrence. Cutaneous metastases generally represent advanced stage of the disease, therefore every new skin lesion in such patients should be looked with suspicion and properly investigated by the clinician for management of these lesions in a diagnosed and treated case of cancer.
Introduction
Oesophageal cancer is the seventh most common cancer and sixth leading cause of mortality due to cancers [1]. Squamous cell carcinoma and adenocarcinoma are the two most common histological types of oesophageal cancer, among them adenocarcinoma is more common in lower third of oesophagus and G.E junction [2]. The order of distant metastases to different sites in oesophageal carcinoma is the liver, followed by distant lymph nodes, lung, bone, and brain [3]. Oesophagus as the primary site of tumor with metastases to the skin is a very rare entity with an incidence of less than 0.5% and it is the oesophageal adenocarcinoma, which is more prone to be associated with cutaneous metastases [4]. Cutaneous metastases (CM) is defined as growth of cancer cells in the skin originating from internal cancer. Cutaneous metastases are a rare finding having the incidence ranging from 0.7% to 10% and accounts for 2% of skin tumours [5]. Cutaneous metastases rarely present as initial disease, it usually starts developing after the initial diagnosis of the primary internal malignancy [6]. Cutaneous metastases from lung being the most frequent internal malignancy (28.6%) followed by metastatic melanoma (nonlocal recurrence;18.2%), gastrointestinal malignancy(i.e oesophagus, stomach, colon and rectum) (14.2%), genitourinary malignancy (10.4%), head and neck primary (9.1%),haematological malignancy (5.2%), breast (5.2%), and miscellaneous (<2%)[7]. The incidence of all cutaneous metastases originating from both squamous cell carcinomas and adenocarcinomas of oesophagus is <1% [8]. On examination these cutaneous lesions may reveal inflammatory rashes, papules or patches, erythematous, indurated plaques or skin nodules. Patients with cutaneous metastases to skull, upper lip, scalp, neck, chest, and abdominal wall have been reported in the literature [9].This is a case report of a patient who was referred to our department of radiation oncology with cutaneous metastases in primary gastro-oesophageal junction adenocarcinoma.
Case Report
A 62-year male who was a reformed smoker and alcoholic with no known comorbidities presented with complaints of dysphagia, dyspepsia, and regurgitation since 7 to 8 months before coming to the clinician in July2017. There was dysphagia initially to solid foods followed by liquids. He also had loss of appetite and loss of weight (around 5kgs) in last 5 months (prior to July2017). On upper gastrointestinal endoscopy (july2017), a growth was found in esophagus at 40 cm and extending to lesser curvature of stomach. Biopsy from both the sites were taken which revealed moderately differentiated adenocarcinoma. The patient received 6 cycles of neoadjuvant chemotherapy of 5-Fluorouracil (5-FU) and oxaliplatin. Then he underwent extended gastrectomy , distal pancreatectomy, splenectomy , Roux-en-y oesophagojejunostomy with end to side anastomosis and distal jejunojejunostomy with side to side anastomosis in march 2018.Per operatively a large tumor of 10×8cm in the G.E junction extending upto proximal stomach ,circumferential infiltrating posteriorly into the body and tail of pancreas was found. Multiple enlarged lymph nodes along lesser curvature was found , the largest measuring 2×1cm. Post-operative histopathological examination (HPE) revealed adenocarcinoma along with lymph node involvement-6/38, peripancreatic lymph node-7/8, lymphovascular invasion (LVI) and perineural invasion (PNI) present and retroperitoneal margin was free. Patient was on feeding jejunostomy for approximately 2 months. After that patient received docetaxel and capecitabine based adjuvant chemotherapy for 6 cycles which he completed in July2018. Patient was on follow up after chemotherapy, but he did not receive any adjuvant radiotherapy. The patient then started developing a dark pigmented patch over dorsum of right forearm which was associated with itching after 11 months of treatment completion. Patient took alternative treatment (details of which are unknown) and did not consult any oncologist. Patient presented to us in September2020 with a nodular growth involving the inter-phalangeal area between the thumb and the index finger and two other sites with similar growth in right forearm along with bleeding from the lesions.
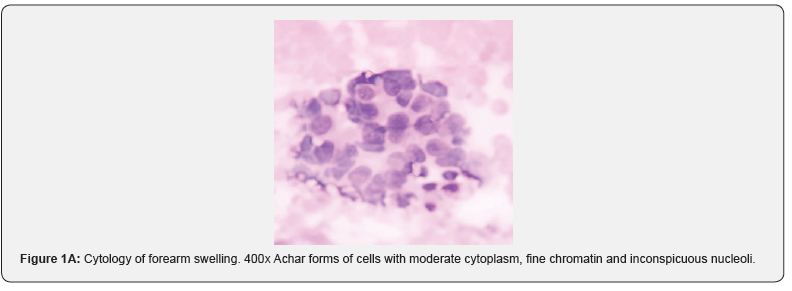
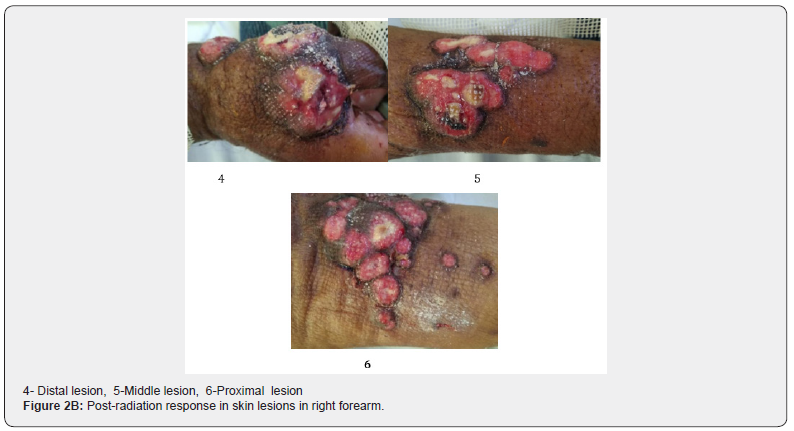
Patient underwent a whole-body positron emission tomography (PET) scan (19/09/2020) which revealed widespread metastases including brain, pulmonary, adrenals and hepatic lesions along with extensive lymphadenopathy. There was also presence of hypermetabolic uptake in right arm, the largest measuring 5.9X5.5cm in the inter-phalangeal area between the thumb and the index finger. Biopsy from the right arm nodular lesion done on 22/09/2020 revealed adenocarcinoma (Figures 1A & B) and immunohistochemistry (CK7 positive, CK20 negative, CDX2 positive and Her 2 neu negative) confirmed its primary to be the same. Patient was then referred to radiation oncology department for opinion. We planned direct external beam radiotherapy to the cutaneous lesions on right forearm (Figure 2A) using 6 mega-electron volt(MeV) electron beams on linear accelerator (Clinac iX Linear accelerator) to a dose of 30Gy in10 fractions (daily once, 5 days a week) from 28/09/2020 to 10/10/2020. The lesion responded with the radiation therapy (Figure 2B) and the bleeding from the lesions also stopped. Thereafter patient started complaints of headache and giddiness. Contrast-enhanced MRI brain was advised which revealed right cerebellar lesion with perilesional oedema. The patient was planned for palliative RT to brain but patient deteriorated due to poor general condition and was admitted in intensive care unit (I.C.U). The patient expired on 31/10/2020 after 2years and 3months from the diagnosis of the primary disease (Figures 1 & 2).


Discussion
Cutaneous metastases from oesophageal cancer are a very rare finding. There are only limited case reports in the literature regarding their incidence. The most common metastases in oesophageal cancer are seen to the lymph nodes, lung, liver, bones, adrenal glands and brain. The average time of development of metastatic disease after onset of the primary disease is approximately 2.9 years [10]. Cutaneous metastases (CM) is a rare phenomenon with an occurrence of <2% of all the tumours that metastasize to the skin [11]. CM is considered a poor prognostic factor due to its aggressive nature. Median survival of patient with CM has been reported to be 4.7 months [12]. CM can occur by lymphatic and hematogenic spread and due to its aggressive nature, it is associated with a grave prognosis. Schoenlaub and colleagues reviewed the clinical findings and overall survival of 200 patients (99 men and 101 women) with cutaneous metastases of various cancers. The incidence of cutaneous metastases from adenocarcinoma of oesophagus was 2 out of the 200 cases studied. The cancers most frequently causing cutaneous metastases were breast cancers (n = 64), pulmonary cancers (n = 36) and melanomas (n = 31). The study revealed that half of patients with cutaneous metastasis died within the first 6 months after the diagnosis. [12] Emily Higgins et al presented a case report of a 67years old male with a non-tender swelling of cheek, from which biopsy was taken. Histology reported metastatic adenocarcinoma, suggesting oesophagus as the primary site. On work up the disease was found to be associated with bone (lumbar and cervical vertebrae) and lung metastases. The cheek lesion and lumbar spine was given radiotherapy (5 fractions) and it responded well. But seeing the extensive nature of the disease, palliative chemotherapy (epirubicin, oxaplatin and capecitabine) was planned and expected survival was 3-6months [13]. Sridhar P et al. presented a case report of a 30years old male patient with squamous cell carcinoma of lower thoracic oesophagus extending up to G.E junction.
Patient was treated with concurrent chemoradiation. Later on patient developed multiple solid skin nodules over left chest which on investigations confirmed its origin from the primary disease. Patient was given palliative radiation to the skin lesions (30Gy/10#) on 6 MeVelectrons at 3cm depth. Patient responded well and was symptom free post palliative therapy [14]. Reingold reported clinical and necropsy findings of 32 cases of cutaneous metastases out of 2,300 internal carcinomas. The most common primary site was the lungs (50%). The oesophagus was the primary tumor site in just one case and that was an adenocarcinoma. The most common sites of skin metastases were on the chest and abdomen. The survival from the appearance of the skin nodules to death averaged about 3 months[15] Tharakaram S et al studied fifty patients (26 men and 24 women) with cutaneous metastases clinically and histologically. Analysis based on the site of the primary tumour showed carcinoma of the lung and oesophagus to be the commonest tumours responsible in men and carcinoma of the breast and ovaries the commonest in women. Metastases occurred in all areas of the skin with the chest wall being the most common site. Most of the cutaneous metastases occurred after the primary malignancy was manifested and was well advanced in stage [16]. In a retrospective series by Shaheen O et al between 1982 and February 2017, a total number of 164 patients were included in the study. The median survival of patients with oesophageal cancer at stage IV was 4 to 6 months, distant metastases was spread to five main anatomical sites: head and neck (42%), thoracic (17%), abdomen and pelvis (25%), extremities (9%), and multiple skin/subcutaneous and muscle metastases (7%). About two-thirds of the unexpected metastases originated from the lower oesophagus, and the two major histological types of the cancer were adenocarcinoma in 40% and squamous cell carcinoma in 60% [10].
A retrospective study by D.P.Lookingbill et.al in 4020 patients with metastatic disease showed that 420 (10%) had cutaneous metastases; out of that 306 patients had skin metastases as the first sign of extranodal metastases. Breast cancer and melanoma were the most common primary sites. Nodules were the most frequent clinical presentation, although inflammatory, cicatricial, and bullous lesions were also noted. Histological findings most frequently revealed adenocarcinoma which was suggestive of the site of origin of disease. After the biopsy proven skin metastases, mean patient survival ranged from 1 to 34 months depending on the tumor type [17]. Patient in the reported case after the diagnosis , was given neoadjuvant chemotherapy, and then underwent surgery followed by adjuvant chemotherapy; but did not receive any adjuvant radiotherapy despite of multiple nodes positive(indication for post-operative radiotherapy). The cutaneous lesions of right forearm of the patient were nodular as mentioned in literature but patient ignored the lesion which might have been be the beginning of widespread metastasis. Lesions were treated with 6 MeV electron beams on linear accelerator (clinac IX LINAC) to a dose of 30Gy in10 fractions. There was obvious response seen in the lesions as shown in above images (Figure-2B). Then the patient succumbed to extensive metastasis after 2years and 3months of the diagnosis of primary malignancy(G.E junction adenocarcinoma) and after 1month and 9 days from diagnosis of cutaneous metastases.
Conclusion
Cutaneous metastases from adenocarcinoma of gastro oesophageal junction is an extremely rare occurrence, therefore proper follow up of the patient is very important. The clinician should be aware of any high-risk skin lesion and should evaluate it properly in a diagnosed and treated case of cancer. Cutaneous metastases may be a first sign of spreading of extensively metastatic gastro oesophageal junction adenocarcinoma.
References
- Freddie Bray; Jacques Ferlay; Isabelle Soerjomataram; Rebecca L Siegel; Lindsey A Torre; et. al. (2018) Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA CANCER J CLIN 68: 394–424.
- Young JL Jr, Percy CL, Asire AJ, Berg JW, Cusano MM, et. al. (1981) Cancer incidence and mortality in the United States, 1973-77. Natl Cancer Inst Monogr (57): 1-187.
- Wu SG, Zhang WW, He ZY, Sun JY, Chen YX, et. al. (2017) Sites of metastases and overall survival in esophageal cancer: a population-based study. Cancer Manag Res 9: 781-788.
- Quint LE, Hepburn LM, Francis IR, Whyte RI, Orringer MB (1995) Incidence and distribution of distant metastases from newly diagnosed esophageal carcinoma. Cancer 76: 1120-1125.
- Scolyer RA, Murali R, Thompson JF (2010) Cutaneous Metastases. Dermatopathology 637–650.
- Nibhoria S, Tiwana KK, Kaur M, Kumar S (2014) A clinicopathological and immunohistochemical correlation in cutaneous metastases from internal malignancies: a five-year study. J Skin Cancer 2014: 793937.
- Sadia Saeed Connie A. Keehn Michael B (2004) Morgan. Cutaneous metastases: a clinical, pathological, and immunohistochemical appraisal 31(6): 419-430.
- Schwartz RA (1995) Cutaneous metastatic disease. J Am Acad Dermatol 33(2 Pt 1): 161–182.
- Doumit G, Abouhassan W, Piliang MP, Uchin JM, Papay F (2013) Scalp metastases from esophageal adenocarcinoma. Ann Plast Surg 71(1): 60–62.
- Shaheen O, Ghibour A, Alsaid B (2017) Esophageal Cancer Metastases to Unexpected Sites: A Systematic Review. Gastroenterol Res Pract 2017: 1657310.
- Robert A Schwartz (1995) Journal of the American Academy of Dermatology. Cutaneous metastatic disease 33(2): 161-185.
- Schoenlaub P, Sarraux A, Grosshans E, Heid E, Cribier B (2001) Survie après métastases cutanées: étude de 200 cas [Survival after cutaneous metastases: a study of 200 cases. Ann Dermatol Venereol 128(12): 1310-1315.
- Higgins, E, Monaghan, L, & Mani, R. R. (2017) Cutaneous metastasis of a primary oesophageal adenocarcinoma to the right cheek. Journal of surgical case reports 2017(9): rjx181.
- Sridhar P, Nihanthy DS, R Pallad S, T N, Khaleel I, et. al. (2016) Cutaneous Metastasis of Esophageal Squamous Cell Carcinoma (ESCC). Int J Med Res Rev 4(9): 1632-1635.
- Reingold IM (1966) Cutaneous metastases from internal carcinoma. Cancer 19(2): 162-168.
- Tharakaram S (1988) Metastases to the skin. International Journal of Dermatology 27(4): 240-242.
- Lookingbill DP, Spangler N, Helm KF (1993) Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol 29(2 Pt 1): 228-236.






























