Accidental Administration of Doxorubicin Cured a Pediatric Patient with Immune Thrombocytopenic Purpura (ITP)
Basil kadhim Abdullah Al odda1*, Zainab Basil Kadhim Al odda2, Ghada Basil Kadhim Al odda3 and Zena Jameel Ahmed Hussein Al byatee4
1Consultant Basil kadhim Abdullah Al odda, M.B.Ch.B, D.C.H, CABP pediatric (consultant subspecialty pediatric heamato-oncology)-Hiwa teaching hospital, Supervisor of adult clinical Hematology-KBMS Sulaymaniyah, Iraq
2Medical student, School of medicine, Amman University, Jordan
3First stage dentistry student, Al-khatab University, Sulaymaniyah-Iraq
4Teacher, Al-Jwahery primary school, Sulaymaniyah-Iraq
Submission: March 05, 2021; Published:March 16, 2021
*Corresponding Address:Basil kadhim Abdullah Al odda, M.B.Ch.B, D.C.H, CABP pediatric (consultant subspecialty pediatric heamato-oncology)-Hiwa teaching hospital, Supervisor of adult clinical Hematology-KBMS Sulaymaniyah, Iraq
How to cite this article:Basil k A Al o, Zainab B K A o, Ghada B K A o, Zena J A H A b. Accidental Administration of Doxorubicin Cured a Pediatric Patient with Immune Thrombocytopenic Purpura (ITP). Canc Therapy & Oncol Int J. 2021; 18(3): 555987.DOI: 10.19080/CTOIJ.2019.18.555987
Abstract
Immune thrombocytopenic or what is called Idiopathic Thrombocytopenic Purpura (ITP is the most common cause of thrombocytopenia in well appearing Children. The outcome of pediatric ITP is better than that of adult-onset ITP with most pediatric patients with ITP enter spontaneous remission within few months. However still significant percentage of them (approximately 20%) may develop persistent or chronic course of ITP which may associated with increasing risk of bleeding which in turn may affecting the quality of life and causing concerning morbidity and mortality. In general patients with ITP treated with steroid, IVIG, thrombopoietin analogs, rituximab (antiCD20) and possible splenctomy. The use of chemotherapy is restricted to selected cases because of their short- and long-term adverse effects. Doxorubicin is an anthracycline that used commonly in treatment of malignancy especially solid tumor. We reported a young child, male patient who went into long time remission from his chronic refractory ITP after accidental administration of doxorubicin chemotherapy.
Keywords: Chronic ITP; Pediatric; Doxorubicin; Chemotherapy; Iraq
Abbreviations: ITP: Immune Thrombocytopenia Purpura; IVIG: Intravenous Immunoglobulin; CD: Cluster of differentiation; L: Liter; IV: Intravenous; Anti-D: Anti-D (rh) Immunoglobulin; mm: milliliter; h: hour; PT: Prothrobine Time; PTT: Partial Thromboblastine Time; mg/m2: milligram per meter2; HIV: Human Immunodeficiency Virus; IWG: International Working Group
Introduction
Newly diagnosed primary immune thrombocytopenia (ITP) by definition, the platelet count in typical ITP is <100 x 109/L, but most cases have a platelet count of <20 x 109/L, typically occurs in healthy children and is characterized by immune-mediated destruction of otherwise normal platelets. The cause of ITP is not usually known, but the condition can be triggered by a viral infection or other immune phenomenon. ITP affects approximately 5 in 100,000 children per year, most commonly between ages 2 to 5 years [1]. Typical natural history is self- resolution within 6 months, which occurs in 75% to 80% of cases [2]; with some of the remaining children resolving within a year of diagnosis [3]. The pathogenesis of ITP is not fully understood. However, the thrombocytopenia is hypothesized to come from 3 mechanisms: autoantibody-mediated decreased platelet production, autoantibodies directed against platelet membrane antigens that cause increased splenic clearance of platelets and shortened platelet half-life, and deficient platelet formation in the bone marrow. Acute ITP typically occurs after a viral illness, and platelet counts often spontaneously recover within weeks to months [4]. Chronic ITP occurs when thrombocytopenia persists for >12 months [5,6]. The peak incidence of ITP in children is at 5 or 6 years old.
The typical clinical presentation is that of an otherwise healthy child who develops easy bruising and a purpuric rash. Bleeding from mucous membranes, such as nosebleeds or gingival bleeding is seen in about one third of cases. Other sites of bleeding include the gastrointestinal tract, vaginal mucosa, the urinary tract, the retina, and conjunctivae [7]. Treatment includes corticosteroids, splenectomy, immunosuppressants, thrombopoietin receptor agonist drugs, or the spleen tyrosine kinase inhibitor fostamatinib. For life-threatening bleeding, platelet transfusions, IV corticosteroids, IV anti-D immune globulin, or IV immune globulin may be used individually or in combination [8]. Because the majority of pediatric patients with ITP have a self-limiting course and underwent into a spontaneous remission (sometime without treatment) and the treatment lines for those needs to be treated usually included steroid , IVIG, anti-D, thrombopoietin receptor agonist drugs and splenctomy, in addition the limited experience regarding the use of chemotherapy particularly doxorubicin in treatment of patients with ITP, we reported this 4 years male pediatric patient who underwent long term remission after accidental administration of doxorubicin chemotherapy.
Case Report
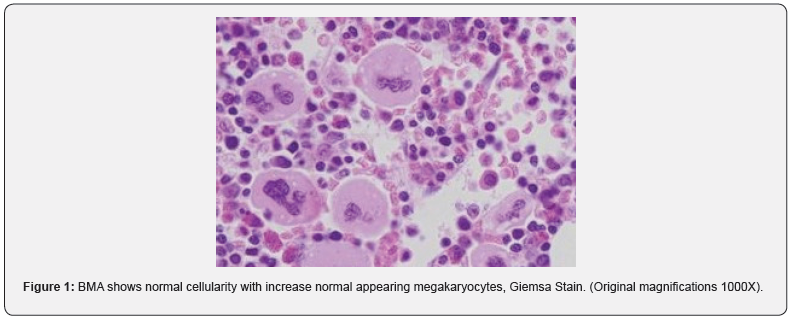
We reported a 4-year-old young child, male patient who is a known case of refractory chronic ITP since the age of 2 year and was treated previously by several courses of different line of treatment including steroid (prednisolone and dexamethasone with a variety of dosage), IVIG, Anti-D, rituximab and thrombopoietin receptor agonist drugs without any subjective response, splenectomy was avoided because of his age (less than 5 year). The patient was admitted to the pediatric hematology unit because of sudden onset spontaneous epistaxis, he had no other symptom. He was fully vaccinated with no consanguinity of parents. Medical and surgical histories were uneventful, family history was negative with no similar condition. On examination, he was afebrile, well looking, no pallor, ecchymosis on both legs and arms, neither hepatomegaly nor lymphadenopathy. Laboratory investigations reveal isolated thrombocytopenia in complete blood picture with Hemoglobin value of 12.4 g/dl, the platelet count was 8,000 per microliter, and a leukocyte count of 9,300 per microliter with 54 % neutrophils, 45% lymphocytes, 1% monocytes, 0.5% basophils and 0% eosinophil, Blood film was normal with neither immature nor abnormal cell, erythrocyte sedimentation rate 14 mm in 1 h. Other laboratory investigations including liver function tests, renal function tests, serum electrolytes (potassium, sodium, calcium, phosphorus); serum uric acid and coagulation profile (PT and PTT), all were normal. Bone marrow aspirate (BMA) and biopsy which was done previously and revealed that morphologically normal hemopoietic cells with increase normal appearing megakaryocytes, this finding is goes with the diagnosis of ITP (Figure 1).
All other investigations which were done previously including viral screen (for HIV, hepatitis B and C), Thyroid function test, Immunoglobulin level and helicobacter pylori (H. pylori) all were negative. We planned to give Him supportive treatment with High dose steroid but accidentally (by mistake) he received approximately 50mg/m2 of doxorubicin (anthracycline chemotherapy) intravenously over one hour, which was prescribed for another patient with malignancy. He was kept in the hospital for one week for observation and follow up, during this period he was well with mild nausea and vomiting for which he received antiemetic, serial CBC was normal apart from the initially low platelet count, slight elevation of liver enzyme from day 3-4 post doxorubicin administration, normal total serum bilirubin, serum troponin level, cardiac echocardiography and ECG all were normal. On day 7 post administration he was discharged from the hospital and then after he kept on regular periodic outpatient follows up. From the second week we observed significant and rapid rising of platelet count which reached approximately 50,000 per microliter on the third week, and more than 100,000 per microliter on the fourth week post-doxorubicin injection. Serial’s liver function test (including Liver enzymes) and echocardiography were normal. Now he is approximately 8 years post the accidental doxorubicin administration without any significant adverse effect.
Discussion
Immune thrombocytopenia (ITP) is commonly encountered by general physicians and pediatricians in their day-to-day practice. With rapid advances in the field of hematology, not only the insight as to the pathophysiology has changed but the terminologies to have changed [9]. The International Working Group (IWG) consensus panel has defined primary ITP as a platelet count less than 100 × 109/L in the absence of other causes or disorders that may be associated with thrombocytopenia. IWG also defines ITP as newly diagnosed (diagnosis to 3 months), persistent (3 to 12 months from diagnosis), or chronic (lasting for more than 12 months). These definitions have not been formally validated and may not apply to patients with secondary forms of ITP [10]. The terminology of ITP is now known as Immune Thrombocytopenic Purpura unlike Idiopathic Thrombocytopenic Purpura in the past and indicates an underlying autoimmune disease in Children [11]. The common age of presentation in children is between 1-7 years of age with an incidence of approximately 5 per 100,000 children [12]. The presentation varies from mild bleeding (most commonly) to life threating bleeding which occur in the minority of the cases, diagnosis usually done from the typical clinical manifestations and by exclusion. There are a variety of treatment modalities (which was described earlier) with not enough evidence to prove that treatment alters the outcome of the disease [9]. There is much controversy about the use of chemotherapy in treating refractory chronic ITP with special concerns regarding the efficacy and safety.
We reported this case of pediatric ITP for two reasons; first because there are only limited knowledges about the use of chemotherapy (namely doxorubicin) in ITP and second because of the potential short (especially chemotherapy induced thrombocytopenia) and long-term complications of this anthracycline chemotherapy.
Our case report, we presented 4 years old boy who was previously confirmed as a known case of chronic ITP refractory to many lines of treatments, presented with bleeding tendency, his clinical examination was normal apart from skin bleeds like petechiae, ecchymosis, and mucosal bleeds as epistaxis. Laboratory investigations also were normal apart from isolated severe thrombocytopenia. Accidentally he received 50 mg/ml doxorubicin chemotherapy which was prepared for other patient, then after he did not develop any significant short- or long-term adverse effects and his platelet count normalized from the third week post doxorubicin administration. Currently he is 8 years post the accidental doxorubicin administration and completely well, free from any long-term complications, with normal platelet count.
Conclusion
This case represents the presentation of a common disease in pediatric patient’s population with hopeful event report scenario. We reported this case Due to the limited studies and knowledge’s regarding the efficacy and safety of doxorubicin. We concluded that single agent short course doxorubicin chemotherapy is a possible effective and safe treatment for selected patients with refractory symptomatic ITP; however, this conclusion needs larger study in both pediatric and adult patients to confirm their efficacy-, short- and long-term adverse effects.
Consent
Written informed consent was obtained from patient’s parent for this case report.
Acknowledgment
We gratefully acknowledge both patient and his family for allowing us to publish their case report.
Authors’ contributions
Consultant Dr. Basil Kadhim Abdallah Al odda has been involved in clinical diagnostic evaluations and management.
Conflict of Interest
The authors declare that they have no conflict of interests.
Funding
Not applicable.
Ethical Consideration
Ethical approval for this case report was obtained from NCI ethical committee. Because of the retrospective nature of this case report, the ethical committee waived the requirement of informed consent.
References
- Witmer CM, Lambert MP, O’Brien SH, Neunert C (2016) Multicenter cohort study comparing U.S. management of inpatient pediatric immune thrombocytopenia to current treatment guidelines. Pediatr Blood Cancer 63(7): 1227-1231.
- Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, et al. (2011) American Society of Hematology. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood 117(16): 4190-4207.
- Imbach P, Kühne T, Müller D, W Berchtold, S Zimmerman, et al. (2006) Childhood ITP: 12 months follow-up data from the prospective registry I of the Intercontinental Childhood ITP Study Group (ICIS). Pediatr Blood Cancer 46(3): 351-356.
- G M Brodeur (2003) Neuroblastoma: biological insights into a clinical enigma. Nature Reviews Cancer 3(3): 203–216.
- Berchtold P, McMillan R, Tani P, Sommerville-Nielsen S, Blanchette VS (1989) Autoantibodies against platelet membrane glycoproteins in children with acute and chronic immune thrombocytopenic purpura. Blood 74(5): 1600–1602.
- McCrae K (2011) Immune thrombocytopenia: no longer idiopathic. Cleve Clin J Med 78(6): 358–373.
- Imbach P, Kühne T, Müller D, W Berchtold, S Zimmerman, et al. (2006) Childhood ITP: 12 months follow-up data from the prospective registry I of the Intercontinental Childhood ITP Study Group (ICIS). Pediatr Blood Cancer 46(3): 351–356.
- Yu-Waye Chu, James Korb, Kathleen M (2000) Sakamoto. Idiopathic Thrombocytopenic Purpura. Pediatrics in Review 21(3): 95-104.
- Neunert C, Terrell DR, Arnold DM, George Buchanan, Douglas B Cines, et al. (2019) American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv 3(23): 3829–3866.
- Dr Priti S Mehta (2001) Immune Thrombocytopenic Purpura In Children, S.L.Raheja Hospital, Saifee Hospital, Surya Children Hospital.
- Cindy Neunert, Wendy Lim, Mark Crowther, Alan Cohen, Lawrence Solberg Jr, Mark A Crowther, et al. (2011) The American Society of Hematology 2011 evidence – based practice guideline for immune thrombocytopenia. Blood 117(16).
- Fogarty PF, Segal JB (2007) The epidemiology of immune thrombocytopenic purpura. Curr Opin Hematol 14(5): 515-519.
- Diane J Nugent (2006) Immune Thrombocytopenic Purpura of Childhood. Hematology Am Soc Hematol Educ Program 1: 1 97-103.






























