The Curvilinear Chine-Scheuermann’s Disease
Anubha Bajaj*
Histopathologist in A B Diagnostics, New Delhi, India
Submission: February 10, 2021; Published:March 11, 2021
*Corresponding Address:Anubha Bajaj, Histopathologist in A B Diagnostics, New Delhi, India
How to cite this article:Anubha B. The Curvilinear Chine-Scheuermann’s Disease. Canc Therapy & Oncol Int J. 2021; 18(3): 555986. DOI: 10.19080/CTOIJ.2021.18.555986
Preface
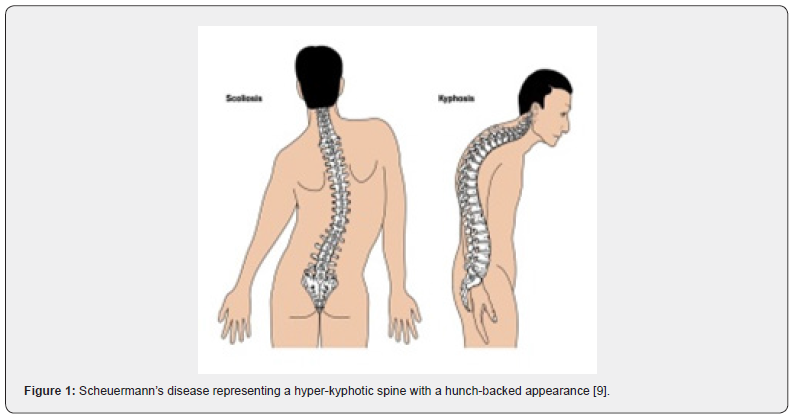
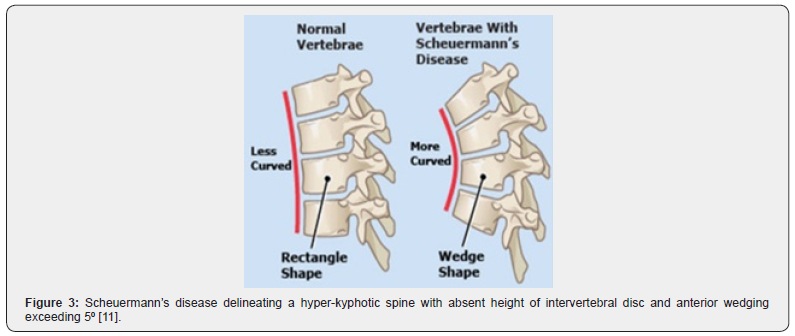
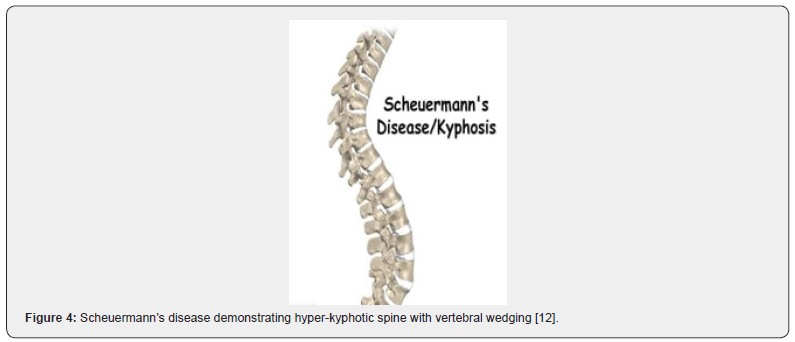
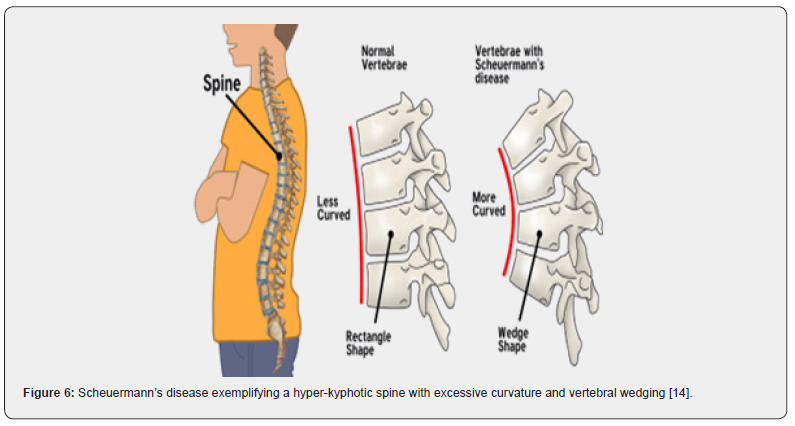
Scheuermann’s disease is a hyper-kyphosis of the spinal vertebrae and intervertebral discs characterized by anterior wedging of ≥ 5⁰ within three or more adjacent vertebral bodies. The thoracic spine is commonly implicated although thoracolumbar or lumbar region can manifest the disease. Scheuermann’s disease is additionally denominated as Scheuermann’s kyphosis, juvenile kyphosis or juvenile discogenic disease.
Disease Characteristics
Disease Characteristics of obscure aetiology, the disease is commonly discerned within adolescents of 12 years to 17 years and is exceptional in children below 10 years. Scheuermann’s disease is the commonest cause of kyphotic deformity in adolescents [1,2]. Mode of disease transmission remains undetermined although a hereditary component contributes to genesis of the disease. Disease incidence is enhanced within monozygotic twins, in contrast to dizygotic twins [1,2].
Disease prevalence appears at around 1% to 8%. A male predominance is observed with a male to female proportion of 2:1 [1,2]. Scheuermann’s disease is categorized as Type I or Classic subtype wherein the thoracic spine is incriminated with curve apex of kyphosis from thoracic vertebral body 7 to vertebral body 9(T7 toT9). Type II wherein the thoracic and lumbar spine is implicated, and curve apex appears at thoracic vertebral body 10 to vertebral body 12(T10 toT12). Type II is likely to progress and engender the disease in adulthood [1,2]. Sorenson et al categorized Scheuermann’s disease as anterior wedging of three or more adjacent vertebrae of around ≥ 5° with an absence of concurrent congenital, infectious, or traumatic disorders of the spine [1,2].
Disease Pathogenesis
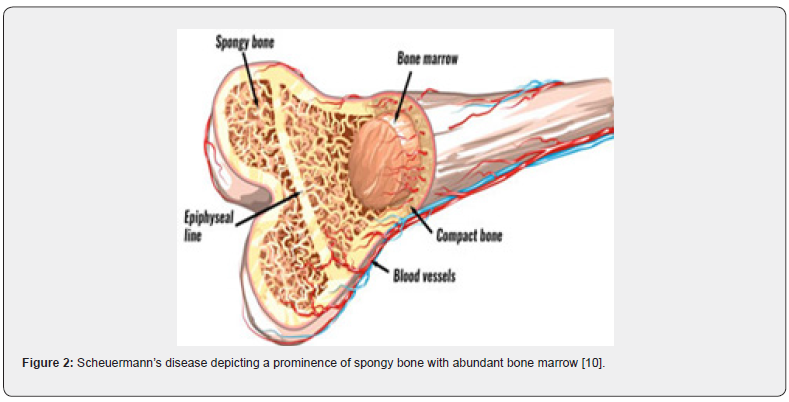
Disease Pathogenesis of obscure pathogenesis, Scheuermann’s disease demonstrates a genetic inheritance. It is posited that mineralization and ossification of vertebral endplate may be discordant during skeletal growth with disproportionate expansion of vertebrae and consequent occurrence of classic wedge-shaped vertebral bodies engendering kyphosis [3,4]. Additional findings include aberrant collagen to proteoglycan ratio, cysts of the dura, osteoporosis occurring during childhood, hypersecretion of growth hormone and appearance of biomechanical stressors as tight hamstring muscles [3,4]. Alternatively, mechanical, metabolic and endocrinologic factors are posited to contribute to occurrence of Scheuermann’s disease [3,4].
Clinical Elucidation
Scheuermann’s disease demonstrates a structural deformity of vertebral bodies and spine wherein kyphosis of thoracic region appears at around 45⁰ to 75⁰ along with vertebral wedging ≥ 5⁰ of 3 or more adjacent vertebrae. Wedge shaped vertebral bodies engender the characteristic, rigid hyper-kyphosis which accentuates upon forward bending and is not relieved with extension or adopting a prone or supine position. However, aforesaid hyper-kyphosis can be counteracted by lumbar and cervical hyper-lordosis [3,4]. Cervical lordosis can be enhanced by protrusion of head wherein shoulders are positioned anteriorly. Mild to moderate scoliosis is an accompaniment. Tight hamstring muscles are exemplified along with muscle stiffness, fatigue, and decreased flexibility of the torso. Neurologic deficits are uncommon [3,4]. A cosmetic or postural deformity or a “hunchback” appearance is observed. Pain can arise within hyper-kyphotic vertebral region. Hyper-kyphosis of the thoracic spine, irregular vertebral endplates, occurrence of Schmorl’s nodes and decimated height of intervertebral disc space, discernible on sagittal imaging, are commonly encountered [3,4].
Implicated adolescents manifest a cosmetic or postural deformity and subacute pain within the thoracic region which worsens upon activity and ameliorates with rest. Typically deformity of spine appears within early to mid-teens [3,4]. Subjects depict physical disability with inability to exercise, work and complete daily activities on account of pain or accompanying physical deformity. Cutaneous pigmentation upon the greatest curvature of hyper-kyphosis can appear due to friction with chairs or seating manifestos. Individuals with Scheuermann’s disease are well muscled [3,4]. Subjects with Scheuermann’s disease demonstrate an enhanced possibility of chronic back pain. Typically, pain within the affected region ameliorates following skeletal maturity [3,4]. Severe instances are exceptionally associated with impaired cardiac and pulmonary function along with serious neurological symptoms [3,4].
Histological Elucidation
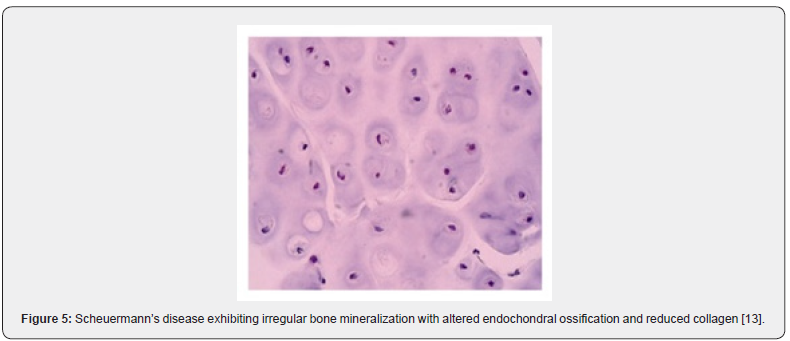
On microscopy, aberrant cartilage of the vertebral endplate, foci of irregular bony mineralization, altered endochondral ossification, reduced collagen to proteoglycan ratio with enhanced proteoglycan values are discerned [5] (Figures 1-6).
Differential Diagnosis
Scheuermann’s disease necessitates a segregation from conditions such as postural kyphosis with flexible postural deformity hyper-kyphosis contingent to secondary disease postsurgical kyphosis ankylosing spondylitis scoliosis [5,6].
Investigative Assay
Upon physical examination, a rigid curve of hyper-kyphosis is observed which accentuates upon forward bending. Hyperkyphosis is unrelieved upon extension, prone or supine position thereby implying a “rigid” deformity. Additionally, cervical, or lumbar lordosis, scoliosis and contracted hamstrings are observed. Although neurologic symptoms are infrequent, a competent neurologic examination is mandated [6,7]. Physical examination of Scheuermann’s disease is comprised of postural assessment with anterior, posterior, and lateral view along with neurological screening to exclude impending paraplegia with clonus and hyperreflexia. Associated scoliosis can be assessed with Adam’s forward- bend test. Evaluation of muscle length, especially of pectorals, hamstrings, sub-occipitals, and flexors of hip joint along with possible contractures of anterior shoulder and hip is necessitated. Evaluation of muscle strength of abdominal, core, gluteal muscles and extensors of trunk is mandated [6,7].
Evaluation of spinal range of motion is necessitated with assessment of planes such as flexion/extension, right/left lateral bending and right/left spinal rotation. Percentage of hyperkyphosis requires assessment upon serial imaging to evaluate degree of disease progression. Investigating the functional range of motion along with degree of deformity aids in appropriate therapeutic intervention and assaying prognostic outcomes [7,8].
Plain radiographs such as antero-posterior or lateral radiographs are essential to evaluate Scheuermann’s disease. Lateral radiographs can appropriately categorize diagnostic criteria such as rigid hyper-kyphosis exceeding 400 and anterior wedging ≥ 5⁰ in three or more adjacent vertebral bodies[7,8].
Additionally, antero-posterior, or lateral radiographs display irregular vertebral endplates, Schmorl’s nodes, lack of height of intervertebral disc space, scoliosis, spondylolysis or spondylolisthesis and herniation of intervertebral disc [7,8]. Magnetic resonance imaging (MRI) can evaluate anatomic alterations or be employed for pre-operative planning. Computerized tomography (CT) is usually unnecessary as are non-diagnostic haematological or biochemical parameters or cogent histological features [7,8].
Therapeutic Options
Scheuermann’s disease can be appropriately managed with non-operative techniques such as stretching, lifestyle modification, physical therapy, and administration of non-steroidal antiinflammatory drugs (NSAIDs). Anti-inflammatory agents are employed for a short duration in young individuals and extended duration in adult subjects with continuous pain [6,8]. Noninvasive therapy is advantageous in asymptomatic individuals or subjects with kyphosis<60⁰ [6,8]. Extension bracing is adopted for kyphosis between 60⁰ to 80⁰ and symptomatic individuals. It is typically required for a period of 12 months to 24 months and delays progression of kyphosis. Skeletally immature individuals are benefitted, and bracing is efficaciously adopted prior to skeletal maturity at around 14 years. Ideally, a brace is applied at puberty for approximately 2 years and removed at skeletal maturity [7,8]. Diverse categories of braces such as Milwaukee brace, kyphologic brace and thoraco-lumbosacral orthosisstyle Boston brace can be employed. Treatment with brace is advantageous in kyphosis between 55⁰ and 80⁰, especially in skeletally immature subjects [7,8].
Adjuvant physiotherapy is recommended in combination with bracing. Physiotherapy is preferably adopted to assist with pain, appropriate spinal posturing, assessment and therapy of muscular imbalance which affects mechanical pull upon the spine [7,8]. Surgical methodologies such as spinal fusion are indicated when kyphosis exceeding > 75⁰ engenders an unacceptable deformity, neurologic deficit, spinal cord compression and severe refractory pain. Symptomatic amelioration as well as melioration of curve deformity is delineated [7,8]. Conservative management is optimal for majority of incriminated subjects. Pain within implicated region ameliorates with emergence of skeletal maturity. However, an enhanced possible occurrence of chronic back pain is observed. Skeletally mature subjects with a kyphotic curve <60⁰ are devoid of long-term sequelae [7,8]. Scheuermann’s disease is associated with complications such as progressive cosmetic deformity, chronic back pain, neurological deficits, and spinal cord compression. Additionally, postoperative complications such as pseudo-arthrosis and persistent pain may ensue [7,8].
Extension-based stretching, stretching of hamstrings, muscle strengthening, adequate body posture and body mechanic techniques are advantageous for treating Scheuermann’s disease. Appropriate employment and handling of braces is recommended. Bracing can be adopted for pain relief in adults where surgical treatment is not recommended [7,8]. Neurologic deficits require an exclusion while treating hyper-kyphosis unresponsive to conservative management. Subjects may depict compromised pulmonary function tests on account of kyphosis [7,8].
References
- Mansfield JT, Bennett M (2020) Scheuermann Disease Stat Pearls International, Treasure Island, Florida, USA.
- Bezalel Tomer, Leonid Kalichman (2015) Improvement of clinical and radio-graphical presentation of Scheuermann disease after Schroth therapy treatment. J Bodyw Mov Ther 19(2): 232-237.
- Berdishevsky Hagit (2016) Outcome of intensive outpatient rehabilitation and bracing in an adult patient with Scheuermann’s disease evaluated by radiologic imaging-a case report. Scoliosis and spinal disorders 11(2): 40.
- Palazzo C, Sailhan F, Michel Revel (2014) Scheuermann's disease: an update. Joint Bone Spine 81(3): 209-214.
- Makurthou AA, Oei L, Salih El Saddy, Stephan J Breda, Martha C Castaño-Betancourt, et al. (2013) Scheuermann disease: evaluation of radiological criteria and population prevalence. Spine (Phila Pa 1976) 38(19): 1690-1694.
- Zaidman AM, Zaidman MN, E L Strokova, A V Korel, E V Kalashnikova, et al. (2013) The mode of inheritance of Scheuermann's disease. Biomed Res Int 2013: 973716.
- Tomé-Bermejo F, Tsirikos AI (2012) Current concepts on Scheuermann kyphosis: clinical presentation, diagnosis and controversies around treatment. Rev Esp Cir Ortop Traumatol 56(6): 491-505.
- Weiss HR, Turnbull D, Silvia Bohr (2009) Brace treatment for patients with Scheuermann's disease - a review of the literature and first experiences with a new brace design. Scoliosis 4: 22.
- Image 1 Courtesy: Spine universe.com
- Image 2 Courtesy: Virtual sports injury clinic.
- Image 3 Courtesy: Scoliosis and spine associates.
- Image 4 Courtesy: Concord orthopaedics.
- Image 5 Courtesy: Hindawi.com
- Image 6 Courtesy: Align Brace.com.






























