Study and Analysis of the Conformation Number and the Integral Dose as Evaluation Tools in Head and Neck Tumors: for Advanced 3-Dimensional Conformal Radiation Therapy Techniques
Abotaleb Hanan A1*, Attalah Ehab M2, El-Hossary Fayez M3 and Ismaiel Mohamed R3
1Sohag armed forced oncology center, Egypt
2Professor of Medical Physics, National Cancer Institute, Cairo University, Egypt
3Professor at faculty of Science, Sohag University, Egypt
Submission:November 11, 2020; Published:December 11, 2020
*Corresponding Address:Hanan Abdelrazek Soliman Abotaleb, Sohag armed forced oncology center, 6 Nile street- Akhmim- Sohag, Egypt
How to cite this article:Abotaleb H A, Attalah E M, El-Hossary F M, Ismaiel M R. Study and Analysis of the Conformation Number and the Integral Dose as Evaluation Tools in Head and Neck Tumors: for Advanced 3-Dimensional Conformal Radiation Therapy Techniques. Canc Therapy & Oncol Int J. 2020; 17(4): 555966.DOI:10.19080/CTOIJ.2020.17.555966
Abstract
Aim: This study was focused on evaluating forward three-dimensional conformal radiation therapy (3DCRT) planning techniques (such as forward-planned multisegments (FPMS), field-in-field (FIF), bellinzona and conpas) by conformation number (CN) of dose to tumor, integral dose (ID) to normal healthy tissues and the other important dosimetric data in each technique. Methods and Material: Fifteen patients of head and neck cancer with different advanced tumors (5 larynx, 6 hypopharynx, 4 oropharynx) were randomly included for this comparative retrospective study. For each patient, five plans were executed by utilizing the four previously mentioned forward planning techniques. Some amendments have been made on both FPMS and Conpas techniques. Two plans were executed by FPMS; the first one was using multiple photon energies referred as FPMS(M) and another identical plan of FPMS but using single photon energy referred as FPMS(S).
Statistical Analysis: Statistically important differences between the competing technique were analyzed by a paired two-tailed T-test for pairwise comparisons and one-way anova test for all the techniques collectively. P values <0.5 were considered statistically significant. The techniques were compared mainly in terms of CN and ID besides, PTV coverage, doses to parotids, spinal cord maximum dose and homogeneity index.
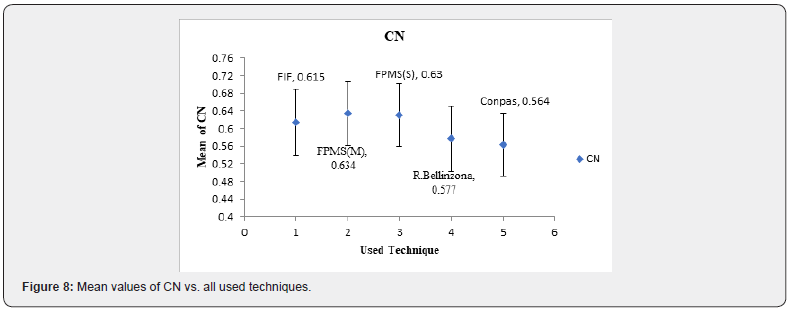
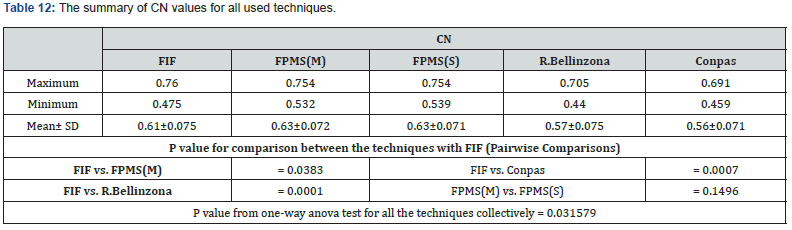
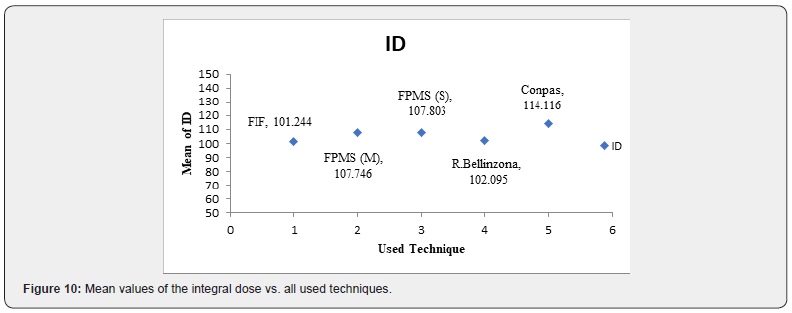
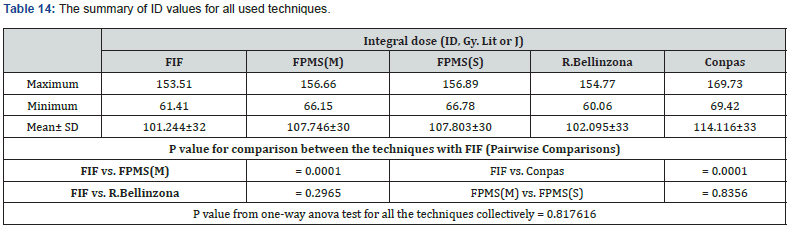
Results: The results revealed that, CN recorded values of 0.634±0.072, 0.630±0.071, 0.615±0.075, 0.577±0.075 and 0.564±0.071 for FPMS (M), FPMS (S), FIF, Bellinzona, and Conpas respectively. ID recorded values of 101.244 ± 32 J, 102.095 ± 33 J, 107.746 ± 30 J, 107.803 ±30 J and 114.116 ± 33 J for FIF, Bellinzona, FPMS(M), FPMS(S) and conpas, respectively.
Conclusion: Considering CN, FPMS demonstrated the highest conformation, FIF was the next followed by R. bellinzona and finally conpas. FIF had the lowest integral dose value, the next was bellinzona, followed by FPMS and finally conpas presented the maximum value.
Keywords: Forward planning; Conformation number; Integral dose; PTV coverage; Homogeneity index; Parotid doses; Head and neck tumors
Introduction
Conformation and congruence of radiation dose is very substantial to reduce the harmful effects on organs at risk (OARs) as much as possible, especially if the matter requires high doses, so the tumor can be controlled. Very sophisticated techniques using inverse planning (IP) as intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) have been evolved to achieve the promising balance between highly required tumor local control and sparing critical organs at risk [1]. The challenge manifests in head and neck tumors, because this region is distinguished by its complex anatomy and a large extension of planning target volume (PTV) with the convex shape embracing the cord; the most vital organ at risk at this location [2]. The former sophisticated techniques have been established principally for head and neck tumors. When and where IMRT or VMAT cannot be used, 3-dimensional conformal radiation therapy (3DCRT) through forward planning is considered worthily strong alternative to the inverse planning [3].
3DCRT with the aid of beam eye view (BEV) lets to use multiple oblique and non-coplanar fields, which together with variations in beams weight, wedges, and multi-leaf collimators (MLC) can fulfil the desired congruence of dose on the tumor with the protection of adjacent normal tissue [4]. Some manuals “forward” iterative 3D planning techniques were done to produce plans simulate those of IP-IMRT for head and neck tumors. Among these attempts; Bellinzona technique [5], Forward-Planned Multisegments (FPMS) [3], 3-D Conformal Parotid Gland-Sparing (conPas) [6], field-in-field (FIF) [7] and oblique photon fields technique (OPFT) [8]. The first four techniques mentioned above were compared in 2013 by Herrassi et al. [1] to investigate the most effective technique which achieves sufficient PTV’s dose coverage while keeping parotid glands and spinal cord sparing. This study compared the first four techniques as herrassi done but also extracted conformation number (CN), integral dose (IN) and homogeneity index (HI) with some amendments on both FPMS and conpas techniques.
Materials and Methods
This retrospective comparative study enclosed fifteen patients of head & neck cancer with different advanced tumors (6 hypopharynx, 4 oropharynx, 5 larynx). Thermoplastic head and shoulders masks have been used to immobilize all patients in supine position. For each patient, computed tomography (CT) axial slices were taken every 3mm. The following structures were drawn on each CT slice; 1- Clinical target volume (CTV) including the primary gross tumor volume (GTV), all regions of microscopic spread around GTV and all node levels at risk (depending on the stage and the site) 2- 5 mm margin was extended outside all-around CTV to obtain the planning target volume (PTV) 3- Spinal canal was delineated to represent the spinal cord and 4- each parotid gland was drawn separately. Linac, DMX (Varian Medical Systems) was the linear accelerator used for treatment sessions with 40 pair multi-leaf collimator and 1cm projection of the leaf width at the isocenter. Just 6 MV and 15 MV photon beams were used. All plans were manipulated and optimized by eclipse treatment planning system version 8.14 with anisotropic analytical algorithm (AAA) for photon dose calculation. 54 Gy to the PTV was used as prescribed dose (2 Gy/ fraction, five fractions / week) as a phase one followed by a boost including high risk volume irradiation by shrinking fields. Just the first phase was processed here. Five plans were executed for each patient by bellinzona technique, FIF, conpas, FPMS (using 6 MV and 15 MV) and another identical FPMS (by 6 MV only), thus 75 plans were performed. Some adjustments were made on both conpas and FPMS techniques. A clarification of each used technique in the following:
Bellinzona technique
Fogliata et al. [5] described this technique in detail in 1999. Herrasi [1] revised it to get benefit from MLC instead of blocks as originally proposed and named it revised bellinzona (R. Bellinzona). Bellinzona or revised bellinzona technique generally consists of five fields (also known as 5- field technique). Fields configuration demonstrated as follows.
Two lateral fields including the entire PTV (gantry angles 90 & 270) encompassing the spinal cord. The couch and gantry positions may be varied by about 5-15° to obtain a better dose distribution.
Two symmetrical fields are set with a posterior obliquity sparing the spinal cord (gantry angles 210 - 220° from right & 140 - 150° from left).
A posterior field (gantry = 180°) also sparing the spinal cord and may be divided into two discrete fields if the spinal cord cannot be totally blocked.
Field-in-field Technique
Portaturi et al. [7] described the original technique in detail in 2006. It consists of six gantry angles (0, 180, 280, 80, 220, and 135). Each angle contains two fields in average, so a total of 10- 14 fields resulted in the plan. The multileaf collimator is mainly responsible for field shaping (leaf thickness = 5mm).
Forward planning multisegments technique (FPMS)
N Lee et al. [3] described this technique in detail in 2004. It intended to remedy the primary tumor and the upper neck nodes of head and neck tumors (with matching field for lower anterior neck and supraclavicular nodes). It is a-seven angle beam arrangement represented as an anterior, two symmetrical anterior oblique (gantry angles = 60°& 300°), two lateral and two symmetrical posterior oblique. Four of the 7 gantry angles comprised several segments. For a given angle, 3 segments may be inserted if the case required, so a total of 13 MLC – shaped segments may be resulted in the treatment plan. Exquisite design of each segment and optimization of the related weights is a necessary matter for the treatment planning. The original technique and herassi [1] used 6 MV and 18 MV photon beams as well as wedges. The deviation of this study from the original technique can be demonstrated in the following; 1- 6MV and 15MV photon beams have been utilized instead of 6MV and 18MV beams, 2- all fields (or segments) are composed to include all PTV (containing the upper neck nodes as well as the lower neck and the supraclavicular nodes) thus abolishing the need for an anterior lower neck matching field, 3- the two lateral field and also the two symmetrical anterior oblique are not fixed at the originally gantry angles used; each of them may be kicked out thus turning the gantry versus the anterior position by about 5-10 for a better dose distribution. Finally, the angles of the two symmetrical posterior beams have been set to be 140 (from left) and 220 (from right) and those only the fields where 15 MV beams have been used, and all other fields (or segments) were optimized with 6MV. In addition to this multiple energy modified FPMS (denoted as FPMS (M)) technique, a congruent plan has been done from this technique for each patient, but only using 6 MV beams (denoted as FPMS (S)) to determine the energy effect.
ConPas technique
Wiggenraad R et al. [6] described this technique in 2005. The principle of this six- to- seven field isocentric setup is formed of two pairs of full- length parallel opposed oblique half- beams including a discrete supraclavicular segment. The planning steps begin by setting the isocenter in the anterior part of the vertebral body midway between the upper and lower borders of the PTV. Subsequently, both posterior oblique fields are setup and converted to half-beams by locking the collimators on the side of the spinal cord. These two half fields are the most substantial components for parotid sparing. At first, the two posterior oblique angles are set at 140° and 220° and they can be adjusted in the beam’s eye view mode, thus the parotid glands maximum sparing could be possible. Thereafter, the two anterior oblique beams are established and converted to half-beams by closing the collimators which are off the spinal cord side. Lastly, the full- length AP beam and the supraclavicular segment are established. Beam weights and wedges are optimized in each beam. In this study a deviation has been done from the original design with respect to the two anterior oblique fields, they were kept including all the PTV. The oblique posterior fields have not been half-beam fields, but just get enough with excluding the cord out of these fields with the conservation of the separate supraclavicular segment. This adjusted conpas trial resembles the oblique photon fields (OPFT) to some extent proposed by Lukarski [8].
In general, during the manipulation for all calculated plans for all techniques, some rules have been applied as the following.
i. The isocenter point was optimized to be within the PTV mean with the aid of the treatment planning system,
ii. The dose normalization was made at the isocenter point and the maximum point was fixed to be at 111.2 % of the prescribed dose,
iii. 0.5 cm bolus was used, where there was a need for it in some cases to eliminate the build-up effect on PTV coverage,
iv. MV beams were used for all techniques, except multiple energies FPMS, for each patient,
v. The beams gantry angles were fixed between the calculated techniques to eliminate the gantry angles effects,
vi. All plans were optimized in which D95 (the dose to the 95% of the target volume) to be 95% of the prescribed dose as much as possible,
vii. The PTV-MLC distance was made to be as close as possible (Not restricted to 0.5 cm),
viii. In all techniques, coplanar beams were used despite non-coplanar beams may provide some additional benefit to seek of simplicity, delivery efficiency and reducing treatment time.,
ix. Finally, for Revised Bellinzona, Conpas and FPMS techniques regarding on the case, where the irradiated regions could not be completely covered by a homogeneous dose with wedged fields, half beam blocks were used.
x. For evaluating statistical significance between the different techniques, two tailed t-test were used for pairwise comparison and one-way anova test for comparing all the techniques collectively. P (≤ 0.05) values were considered statistically significant. Figure 1 displays the Beam’s Eye View (BEV) of each used technique beam setup.
These techniques were dosimetrically compared and estimated to each other through the calculation of their dosevolume histograms (DVHs) and extracting the following parameters:
PTV coverage: According to International Commission on Radiation Units and Measurements (ICRU) No.50 [9], recommendations at least 95% of the PTV must be covered by the prescription dose for conformal planning radiotherapy. Despite ICRU guidelines for dose homogeneity to be with +7 and -5%, head and neck cases deviate from these guidelines and a homogeneity of ±10% was more realistic [5].
Doses to organs at risk
In this case, the critical structures in concern are the spinal cord and the parotid glands. For spinal cord being a serial organ, the acceptable tolerance is that the maximum point does not exceed 45 Gy in the first phase and 50 Gy for the total treatment course. Regarding the parotid gland a strong correlation was found between the mean dose to the parotid gland and the parotid gland function and hence mean dose of the parotid gland ≤ 25-30 Gy or D50% ≤ 30 Gy should be the planning objective if the gland function sparing is desired [10].
Conformation number (CN)
CN is an index proposed by van’t Riet et al. [11]. The conformation number importance rises from its ability to evaluate the treatment plan conformity (dose distribution accordance on the tumor) where the competing plan which produce high dose distribution envelope the irregular tumor shape with sharp dose gradient fall-off outside the tumor volume consequently protecting normal tissue around it. CN can be defined as CN = (TVRI/ TV) → (represents the target coverage quality) × (TVRI/VRI) → (represents the healthy tissue volume receiving a dose greater than or equal to the prescribed reference dose) where TV = target volume, TVRI = target volume covered by the reference isodose and VRI = the reference isodose volume. The radiation therapy oncology group (RTOG) [12] presented a conformity index where CIRTOG = (VRI/TV), but this index does not consider the spatial intersection degree of two volumes or their shapes. Also, Lomax and Scheib [13] presented two conformity indices; the first one CI = (TVRI/TV) which represents the target volume percentage receiving the prescribed dose at least, but it is disadvantage that it cannot consider the adjacent healthy tissues volume. The second conformity index called healthy tissues conformity index = (TVRI/ VRI) which assess the proportion of the reference isodose volume, i.e., implicitly assess only the healthy tissue volume included in the reference isodose. So, the CN’s advantage lies where it can avoid the conformity indices drawbacks as presented before, since it considers the target volume irradiation and healthy tissue irradiation with each other. The conformation number value ranges from zero to one, since a value of one indicates the optimum conformation. A value close to zero indicates either conformation total absence or a very large volume of irradiation relative to the target volume.
Homogeneity index (HI)
There are several definitions for the homogeneity indices but, in general homogeneity index considers the ratio between the maximum and the minimum dose in the target volume [14]. Lower HI values are indicator of a more homogenous target dose. Between these definitions, HI = (D2-D98)/ D50, [15] where, D98 is the dose to 98% of the target volume and is “minimum dose” indicating that 98% of the target volume receives this dose or higher. D2 is the dose to 2% of the target volume and is “maximum dose” indicating that only 2% of the target volume receives this dose or higher. D50 is the delivered dose to 50% of the target volume.
Integral Dose (ID)
for any treatment plan, there is arising question of how large the normal tissues mass or volume which exposed to radiation during radiotherapy course [16]. This question is to refrain any harmful effects due to the adjacent normal tissue radiation dose [16]. Integral dose (ID) gives a description of energy deposition across the entire body [17]. Historically, ID can be considered a physical quantity able to represent the physical aggression and complications risk due to radiotherapy [17]. From of the point of view of past and recent literature data, there is a possible correlation between integral dose and secondary malignancies, with more explanation, the increase of energy deposition in healthy tissues might play a leading role in the induction of secondary cancers [18]. Up till now, the extent of integral dose which may be considered clinically acceptable is not known [19]. Generally, it is recommended to keep ID as minimum as possible provided that tumor coverage and normal tissues sparing are acceptable [19]. Its definition is the total energy absorbed by the body and equals to the product of the mean dose in Gray (1 Gy = 1J/Kg) of the all body and its mass in kilogram (Kg). Since the body mass can be substituted as its volume multiplied by its density, the ID can be translated into: ID = Σ_(k=1)^n▒Vk j D k j ρ k j Since VK j, D k j and ρ k j are respectively the volume, dose and density of voxel K in organ J. For simplicity, if all the voxels are considered to have the same size and the organ can be assumed to have a uniform density, so the former equation can be reduced to: ID = V j D j ρ j where D j is the mean organ dose. For the sake of simplicity, a constant density ρ = 1 g/cm3 was assumed for all different structures [17]. Finally, with a simple expression, the integral dose can be considered as. (Figure 1)

Results
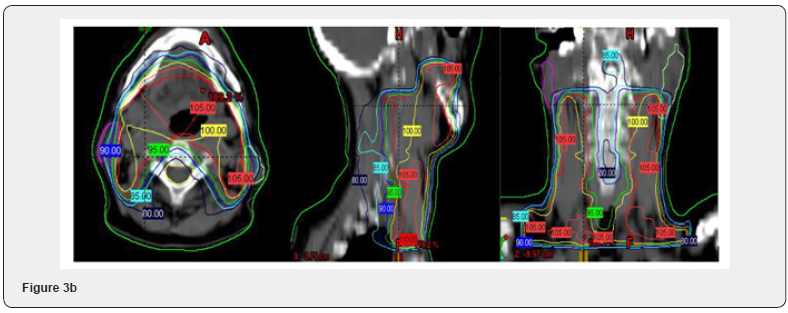
Dosimetric evaluation for overall population will be manipulated. From the first glance, the plan can be evaluated by inspecting the dose distribution on the axial CT slices, slice by slice and on reconstructed multiplanar sections, followed by extracting the important physical parameters from dose volume histogram (DVH), to evaluate all the strengths and weakness aspects of each technique.
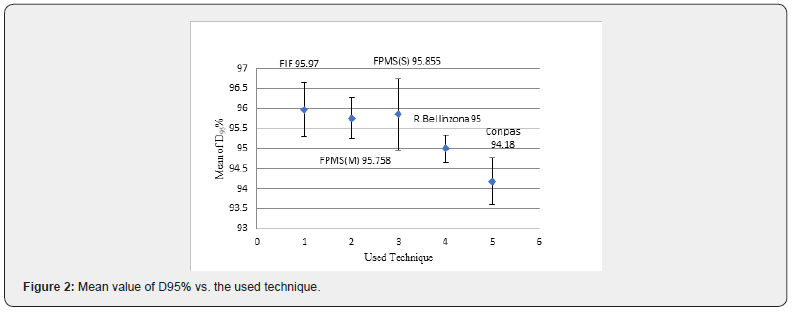
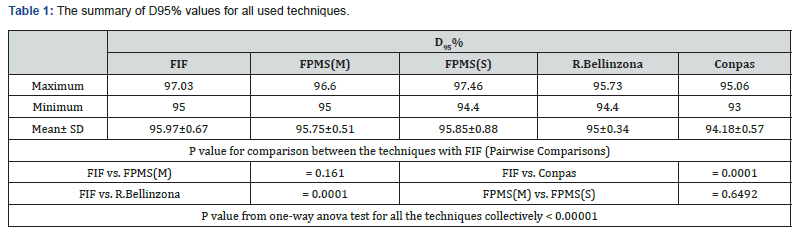
PTV Coverage
Important dosimetric parameters for PTV can be represented in D95%; the prescribed dose percentage value that covers 95% of the target volume (Figure 2 represents the mean value of D95% vs. the used techniques), Dmean; PTV mean dose, near maximum doses expressed by D2 and near minimum doses expressed by D98 are presented in tables 1-4 respectively. From the demonstrated data, it can be discerned that, the PTV coverage is in accordance with the ICRU No. 50 and 62 recommendations [9,20] for all techniques, Since D95% is either very close from 95% of the prescribed dose or above (P<0.00001, for one-way Anova test). In more explanation, FIF and FPMS (whether using single or multiple energies (P = 0.6492, for FPMS(M) vs. FPMS(S))) offer the same PTV coverage and occupy the top ranking (P = 0.161 for FIF vs. FPMS(M)) followed by R. Bellinzona, (P = 0.0001, for FIF vs. R. Bellinzona) and lastly Conpas (P = 0.0001, for FIF vs. Conpas).





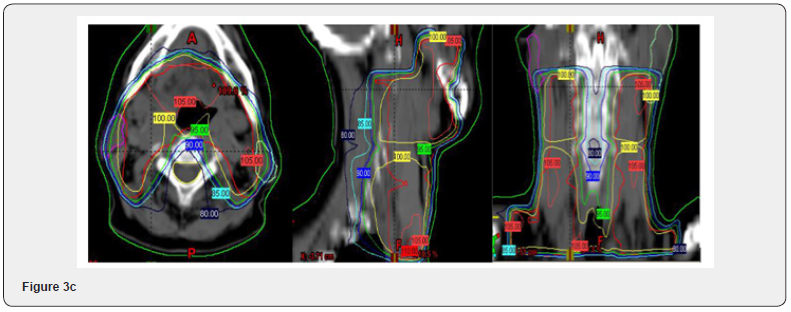
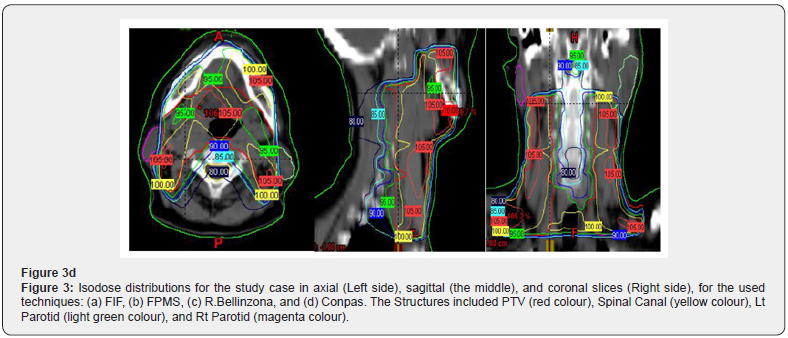
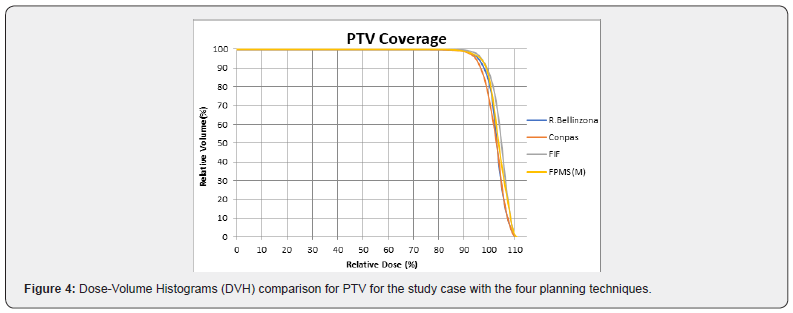
An oropharyngeal case has been chosen as an example for study which is presented in Figure 3. This figure displays the dose distribution in some representative axial, sagittal and coronal slices to demonstrate the ability of each technique to conform the prescribed dose on the target. Moreover, the corresponding DVH is displayed in Figure 4.

Doses to OARs
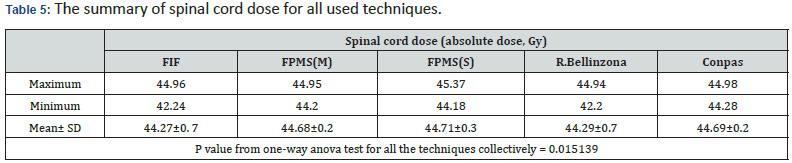
Spinal Cord: table 5 represents the maximum dose to the spinal cord for all used techniques. One can observe from the table that all techniques fulfilled the requirements of dose constraints to the spinal cord, where the maximum dose to the spinal cord should be ≤ 45 Gy in this phase.
Parotid Glands
Various important parotid glands statistical data are represented in D mean%; mean dose to the parotid gland and D50 %; Dose to 50% of the parotid gland volume. With respect to the parotid glands, Xerostomia (dry mouth) is the most radiation induced chronic effect for LAHNC (Locally advanced head and neck cancer) patients. Since the major portion of stimulated saliva is produced by the parotid glands, the parotid glands’ radiation exposure amount plays a vital role in their damage and functional recovery [21]. A strong correlation was found between the parotid glands mean doses and their function. Recently it has been shown that, for parotid mean doses lower than 25-30 Gy (or mean dose received by either parotid should be < 26 Gy, or at least 50% of either parotid glands volume should receive <30 Gy), a function recovery is essential and a return to pre-treatment levels could be achieved in 2 years after RT [10]. Regarding to the parotid glands results demonstrated in this study, it has been found that, in despite the parotid received dose depends strongly on the extension and the disease location, parotid glands appear to be spared to some extent for most of the patients.
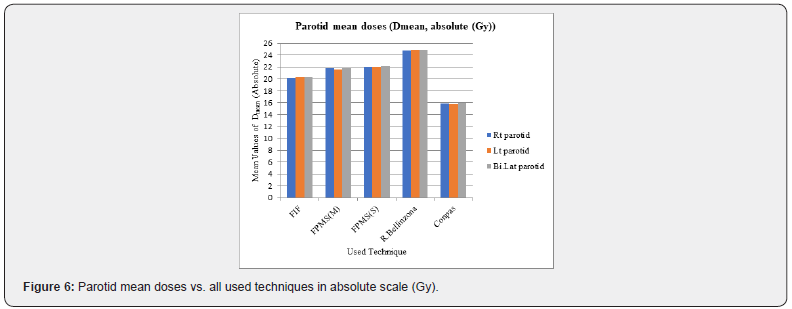
Mean Doses to Parotid Glands
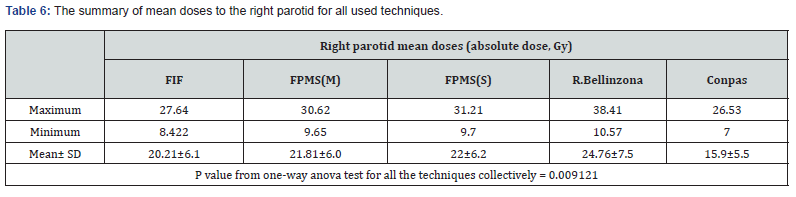
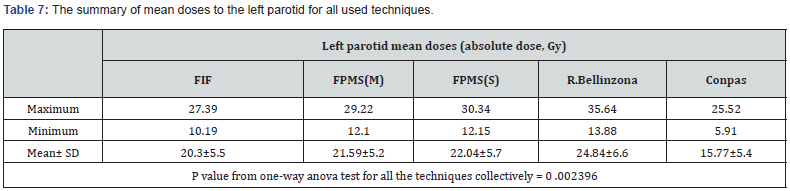
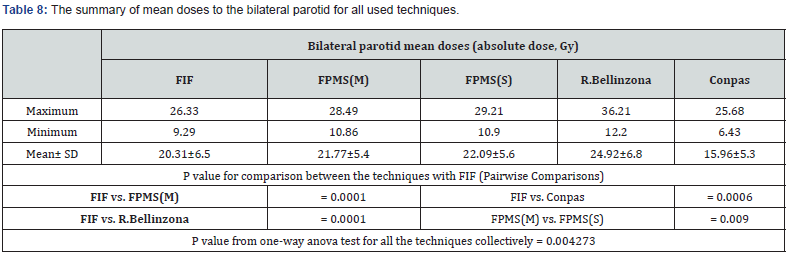
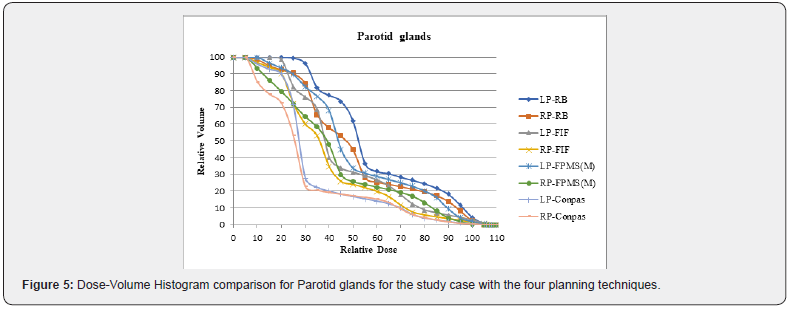
The statistical analysis for the mean doses received by the parotids is tabulated in tables 6-8. A significant differences between the techniques have been observed from the presented tables (P = 0.00427, for one-way Anova test), where the conpas technique offers the best parotid glands sparing. Since the mean value of bilateral parotid mean dose; D mean is equal to 15.96 Gy (29.5% of the prescribed dose), P = 0.0006 for FIF vs. Conpas. The next technique is FIF, where D mean = 20.313 Gy (37.61% of the prescribed dose). The third technique is FPMS, where D mean for FPMS (M)=21.772 Gy (40.3% of the prescribed dose), D mean for FPMS (S) = 22.092 Gy (40.9% of the prescribed dose), P=0.009 for FPMS (S) vs. FPMS(M), P=0.0001 for FIF vs. FPMS (M). Moreover, R. Bellinzona presented the maximum doses to the parotids, D mean = 24.92Gy (46.14% of the prescribed dose), P = 0.0001 for FIF vs. R. Bellinzona. Figure 5 displays the dose volume histogram (DVH) for the study case to demonstrate the differences of the parotid gland’s doses between the used techniques. Figure 6 shows the disparity in the mean values for the parotid mean doses as a function of the used technique.
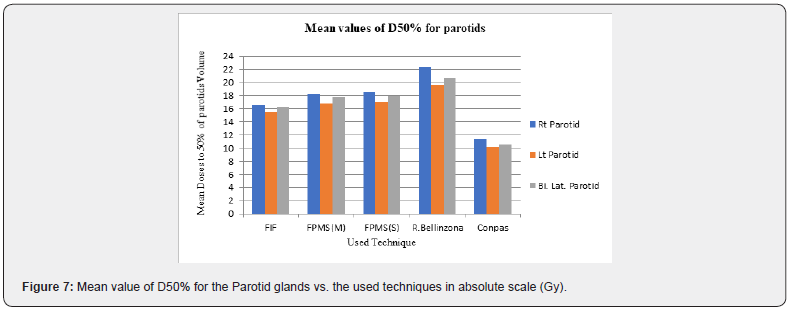
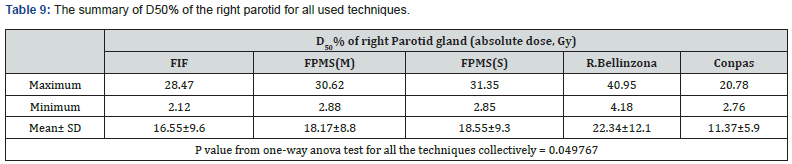
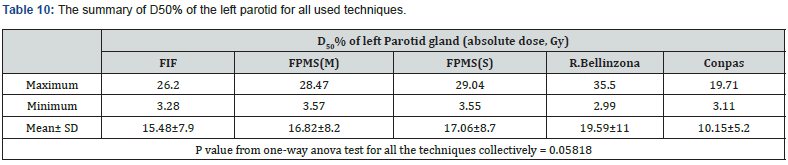
Doses to 50% of Parotids Volume
Doses to 50% of the volume of the parotid glands (D50%) are presented in tables 9-11. For bilateral parotid in conpas technique, the mean of D50% =10.58 Gy (19.6%, of the prescribed dose). In FIF, the mean of D50% =16.27 Gy (30.1% of the prescribed dose). In FPMS(M), the mean of D50% =17.71 Gy (32.8% of the prescribed dose). Finally, in R. Bellinzona, the mean of D50% = 20.73 Gy (38.39% of the prescribed dose). Figure 7 shows the disparity in the mean values of D50% for the parotid glands as a function all used technique.

Conformation number and homogeneity index
Despite 3DCRT sophisticated techniques can conform the dose distribution to the target to some extent that was not formerly possible by conventional 3DCRT, caution must be taken about normal tissues embedded within the target volume especially during dose escalation attempts [11]. Again, the plans dose distribution can be assessed through the isodose lines and the dose volume histogram (DVH). The DVH provides the planner by a numerous important parameter of each volume of interest.
Unlikely, the huge volume of data presented by these histograms; Lines and curves may complicate the matter rather than simplifying it [14]. So, it is nice to present a tool which may be able to assess the treatment plan quality options. The homogeneity and conformity indices are two such tools by them a decision can be taken in favour of a plan which provides simultaneously, maximum tumor coverage homogenously and protects healthy tissues in conformal radiotherapy. Regarding the technique’s conformation, their conformity was assessed in this study using CN. Table 12 offered the summary of CN values. CN recorded values of 0.634±0.072, 0.630±0.071, 0.615±0.075, 0.577±0.075, 0.564±0.071 for FPMS (M), FPMS (S), FIF, R. Bellinzona, and Conpas, respectively. According to CN, the FPMS demonstrated the highest conformation. FIF was the next, followed by R. Bellinzona and lastly Conpas. For Pairwise comparison, the differences were statistically significant since, P = 0.0383 for FIF vs. FPMS(M), P = 0.0001 for FIF vs. R. Bellinzona and P = 0.0007 for FIF vs. Conpas. While there was no significant difference between FPMS (M) and FPMS (S), where P = 0.1496. Figure 8 represents the mean value of CN vs. all used techniques.
Homogeneity Index (HI)
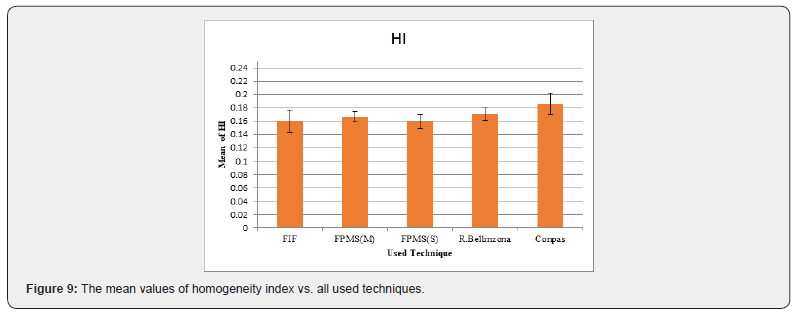
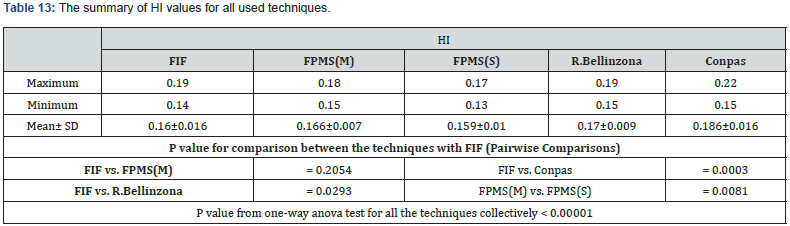
The values summary of HI is listed in table 13. For HI = (D2-D98)/D50; it was found that the highest homogeneity was attained by FPMS (S) = 0.159 ± 0.01, then FIF = 0.16 ± 0.016, the next was FPMS (M) = 0.166 ± 0.007, followed by R. Bellinzona = 0.17 ± 0.009 and lastly Conpas = 0.186 ± 0.016. The statistical difference was found for FPMS (M) vs. FPMS (S), P = 0.0081, for FIF vs. Conpas, P = 0.0003 and FIF vs. R. Bellinzona, P = 0.0293. While there was no significant difference for FIF vs. FPMS (M), P = 0.2054. Figure 9 represents the mean values of homogeneity index vs. all used techniques.
Integral Dose (ID)
The high absorbed dose outside the target, expressed by the integral dose, could be attributed to secondary malignancies, and their incidence may be increased from 1% to 1.75%, so caution must be taken specially in paediatric patients [4]. The ID values summary is listed in table 14. Based on the obtained results; the FIF revealed the lowest integral dose value = 101.224 ± 32.378 J. The next technique was R. Bellinzona = 102.095 ± 33.884 J, followed by FPMS (M) = 107.746 ± 30.717 J. Finally, the Conpas technique offered the maximum integral dose value = 114.116 ± 33.991 J. For Pairwise comparison, the statistically significant differences were found between FIF-FPMS (M) since, P = 0.0001 and FIF- Conpas, P = 0.0001. Whereas there was no significant difference for both FPMS (M) vs. FPMS (S), p = 0.8356 and FIF vs. R. Bellinzona, P = 0.2965. Figure 10 represents the mean values of the integral dose vs. all used techniques.
Discussion
Particularly for head and neck tumours, the delivery of sufficient high doses to the target volume is critical for tumor local control and patient survival [2]. High rates of local control can be achieved with 5-year survival greater than 80% for stage 1 and 2 and 60-70% for stage 3 and 4 tumors [22,23]. Intensity modulated radiation therapy (IMRT) is a recent technique which allows the dose distribution to be highly configured and conformed on the tumor concave shapes, simultaneously with highly sparing for normal tissues adjacent to the tumor, which in turn is very useful especially for H&N tumors because of their complex shapes containing critical organs [2]. IMRT can be split into two wide categories: forward planning versus the inverse planning (IP) [3]. In forward planning, the dosimetrist or physicist chooses the number, weights, energies and angles of beams after that, the dose distribution is calculated by the computer and beam’s-eye views are generated along with dose-volume histograms [3]. As soon as, the beam arrangements are designed, many adjustments and fine tuning are made to optimize the plan. In contrast, the inverse planning begins by defining the desired target dose and normal tissues constraints then the computer undertakes the responsibility of the plan optimization [3]. IP-IMRT has many clinical as well as physical advantages over forward planned IMRT or conventional radiotherapy. But at the same time IP-IMRT has many limitations, which are as follows: 1-It demands a dedicated team of physicists, dosimetrists and therapists who can handle IPIMRT large volumes. 2- Also, not all patients are well candidates for the prolonged treatment time. 3-A stringent quality assurance is another requirement to test the execution of the IMRT delivery system. 4- Scattered and leakage radiation resulted in IMRT treatment session cause an increase of the body integral dose which in turn increase the opportunity for secondary malignancies incidence [4]. 5-Finally, IMRT techniques are not available for all centers. So, some manual “forward” iterative 3D planning techniques (forward intensity modulated radiation therapy) has been developed to overcome some IP-IMRT limitations such as, Bellinzona technique [5] by Fogliata A., et al, 1999, Conpas technique [6] by Wiggenraad, et al.,2005, FPMS technique [3] by Lee et al., 2004 and FIF technique [7] by Portaluri M., et al., 2006. After that Herrassi, et al. [1] 2013 compared between these four techniques to confirm the validity of their implementation with him. The main authors and herrassi presented detailed dosimetric data about these techniques in terms of target coverage, HI, doses to organs at risk. However very poor data about the conformity and integral dose of these techniques have been presented.
In the present work, these techniques have been compared from the point view of the conformity indices and the integral dose which are considered plan evaluation tools with some adjustments on both FPMS (in addition of single energy FPMS presentation) and Conpas techniques as mentioned in materials and methods section. Besides, the other important dosimetric parameters which are very important for the plan evaluation have been presented. For a fair comparison, the gantry angles were fixed between the techniques for each patient. For FIF technique, in the original paper the rang of the prescribed dose was 44-64 Gy (mean 52 Gy, median 50 Gy), the mean dose to the PTV was 96.6% and the maximal dose was 105% of the prescribed dose to the isocenter, the received mean dose by the ipsilateral parotid gland was 46.6 Gy and the mean dose for the contralateral was 38.2 Gy. According to Herrassi work, to the PTV isocenter, the mean dose was 97.7%, a near-minimum dose was 84%, and a near-maximum dose was 104% of the prescribed dose. The parotid glands mean dose was 26 Gy of 54 Gy. In the present work, the PTV mean dose was 103.76%, a near-minimum dose (D99%) was 89.52% (Where D99; is the dose to the 99% of the target volume and is considered to be “minimum dose” , indicating that 99% of the target volume receives this dose or higher), a near-maximum dose (D1%) was 109.87% (where D1; is the dose to the 1% of the target volume and is considered to be “maximum dose”, indicating that only 1% of the target volume receives this dose or higher). The bilateral parotid gland mean dose was 20.313 Gy of 54 Gy. For R. Bellinzona technique, in the original paper, PTV average results were, mean dose of about 100.7%, maximum dose of about 112.8% of the prescribed dose and the parotid median dose of about 97%. According to Herrassi, the mean and maximum PTV doses were 99% and 105.5% respectively, while the parotid median dose was 67%. In the present work, the mean and maximum PTV doses were about 103.33% and 111.2% respectively. The median for bilateral parotid was 38.4%. For FPMS technique, in the original paper the D95% of CTV was 99% of the prescribed dose and the parotid mean dose was 54% of the CTV dose.
According to Herrassi, the D95% of the PTV was 97% and the parotid mean dose was 60 % of the prescribed dose. In the present work with the adjustments to FPMS technique, the D95% of the PTV was 95.75% (for multiple energies) and the bilateral parotid mean dose was 40.3% of the prescribed dose. For Conpas technique, in the original paper, the mean V95% was 91% and the mean parotid dose was about 50% of the prescribed dose. According to Herrassi, V95% was 92% and the mean parotid dose was 48.5% of the prescribed dose. In the present work, D95% of the PTV = 94.18% was extracted instead of V95% and bilateral parotid mean dose was about 30.0% of the prescribed dose, again with the adjustments on Conpas technique. The obtained results in this study of CN and parotids mean were superior to those obtained by Lukarski, et al., 2010 who compared between two different three-dimensional conformal irradiation techniques for head and neck cancer [8]. The classical technique, termed “Electron-Photon fields”, “EPT” and the new technique, termed “oblique photon fields”, “OPFT” their results where all patients were considered as one group were equal to 0.46±0.05, 0.45±0.06 for CN for OPET and EPT respectively. Also, the parotid glands mean doses in (Gy), since the prescribed dose was 50 Gy , were as the following, left parotid = 42.0 ± 9.2, right parotid = 42.6 ± 9.1 for OPET, but with respect to EPT, left parotid = 44.4 ± 7.8, right parotid = 44.3 ± 7.9. Wu Q., et al., 2003 performed a prospective study to test the concept of simultaneous integrated boost intensity modulated radiotherapy (SIB-IMRT) for locally advanced head and neck cancer [24], the prescribed dose was escalated from 68.1 Gy to 73.8 Gy on the patients’ groups. Their average doses to the parotid gland proximal to and distant from GTV were 41.3 Gy and 25.7 Gy, respectively. They displayed the dose distribution for two patients who were treated at 70.8 Gy level, for one of them, the sparing of one parotid was possible, since D50% of the left parotid =17 Gy (24% of the prescribed dose), D50% of the right parotid = 40 Gy (56.49%) and D50% of bilateral parotid = 28 Gy (39.54%). While for the second patient, D50% = 25 Gy (35.3%) for each parotid. In another study, A. Caraman, et al., 2016 compared between 3D conformal, IMRT and VMAT techniques for head and neck cancer of 5 patients [25], the plans were created using the same 6MV photon beams commissioned for Varian clinac ix equipped with a 120-leaf millennium MLC and using the TPS (Treatment Planning System) Eclipse (version 11) and Analitical Anisotropic Algorithm. They assessed the homogeneity index according to ICRU83 formula, which defined HI as (D2%-D98%)/D50%. Their mean HI values were equal to 0.276 (range: 0.25-0.33), 0.12 (range: 0.10-0.17) and 0.096 (range: 0.09-0.11) for 3DCRT, VMAT and IMRT respectively. Comparing the present study results with their 3D-CRT results, it was found that, the obtained mean values of HI were 0.16, 0.166, 0.159, 0.17, 0.186 for FIF, FPMS (M), FPMS (S), R. Bellinzona, and Conpas techniques, respectively; which were much better than their 3DCRT’s HI value. Also, it is important to mention that, when FPMS (M) was compared with FPMS(S), there was no significant statistically differences between most of the measured dosimetric parameters. consequently, 6MV single energy forward planning MultiSegments FPMS(S) is preferred in head and neck tumors to avoid fast neutron contaminations which are associated with high energy.
Conclusion
The conformity indices and the integral dose are very important evaluation tools of the plan quality and should be considered especially for patients who are expected to have long survival lifetime to avoid secondary malignancies incidence risks and at the same time to improve the patient’s quality of life. The present study manipulated four forward planning techniques for head and neck tumors treatment by 3DCRT which are FIF technique, FPMS technique, Bellinzona technique and Conpas technique. Each technique has been evaluated in terms of PTV coverage, doses to organs at risk (OAR), conformation number (CN), homogeneity index (HI), integral dose (ID).
The present analysis revealed the following conclusion:
For PTV coverage: FIF and FPMS (whether using single or multiple energies) offer the same PTV coverage and occupy the top ranking. Moreover, the R. Bellinzona achieved the second ranking and Conpas has the last. With respect to OARs, conpas technique offers the best parotid glands sparing, FIF is the next one, which is followed by FPMS. Moreover, R. Bellinzona presented the maximum doses to the parotids. Considering the CN, the FPMS demonstrated the highest conformation, FIF is the next one which is followed by R. Bellinzona and finally followed by Conpas. Regarding to HI, the highest homogeneity indices were achieved in descending order by FPMS, FIF, R. Bellinzona and lastly Conpas. Lastly for integral dose (ID), FIF revealed the lowest integral dose value, which is followed R. Bellinzona and FPMS. Finally, the Conpas technique offered the maximum integral dose value. Undoubtedly, for any plan evaluation the PTV coverage must be balanced with the other main goals of limiting radiation doses to normal tissues and the parotid glands sparing. So, if the used techniques have been evaluated by considering all the important dosimetric parameters collectively, it will be found that the best choice for the used technique is in favour of FIF technique. At the same time, the other three techniques achieve well the clinical requirements.
References
- Hill et al, (1994) Radiology91: 447-54
- Eisbruch A, Marsh LH, Dawson LA, Carol R Bradford, Theodoros N Teknos, (2004)Recurrence near base of skull after IMRT for Head and neck cancer: Implications for target delineation in high neck and for parotid gland sparing. J Radiation Oncology BiolPhys59(1): 28-42.
- Martinez (1999) Radiology 211:815-828.
- Antolak (1999) IJROBP 44:1165.
- Rosenzweig (2000) IJROBP 48:81-87.
- Mohan (2000) IJROBP 46:619-630.
- Chao KSC, Wippold FS, Ozygit G (2002) Determination of oral delineation on nodal target volumes for head and neck cancers based on pattern of failure in patients receiving definitive and postoperative IMRT. Inj J Radiat OncolPhys53(5): 1174 -1184.






























